Since the first use of cytotoxic chemicals to treat cancer, oncologists have been searching for ways to improve efficacy without significantly increasing overall toxicity to patients. One of the methods attempted to enhance the killing effect on tumor cells is the use of cytotoxic agents with potency at picomolar or lower levels (such as microtubule inhibitors or DNA alkylating agents). However, these compounds lack sufficient therapeutic windows for cancer treatment.
The invention of monoclonal antibodies has provided the possibility of utilizing their strong specificity as a mechanism to create antibody-drug conjugates (ADCs) through chemical coupling with cytotoxic effectors, thereby selectively delivering cytotoxic drugs to cancer cells.
Although this “simple concept” faces many challenges in clinical practice, it has catalyzed active research in the field since the FDA approved Brentuximab vedotin (BV) in 2011 and Trastuzumab emtansine (T-DM1) in 2013. Currently, there are at least dozens of ADC candidates undergoing clinical evaluation worldwide.
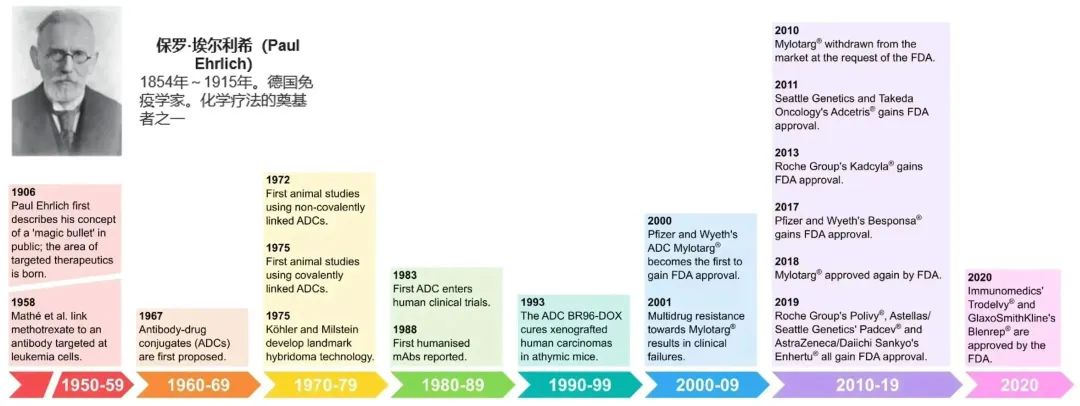
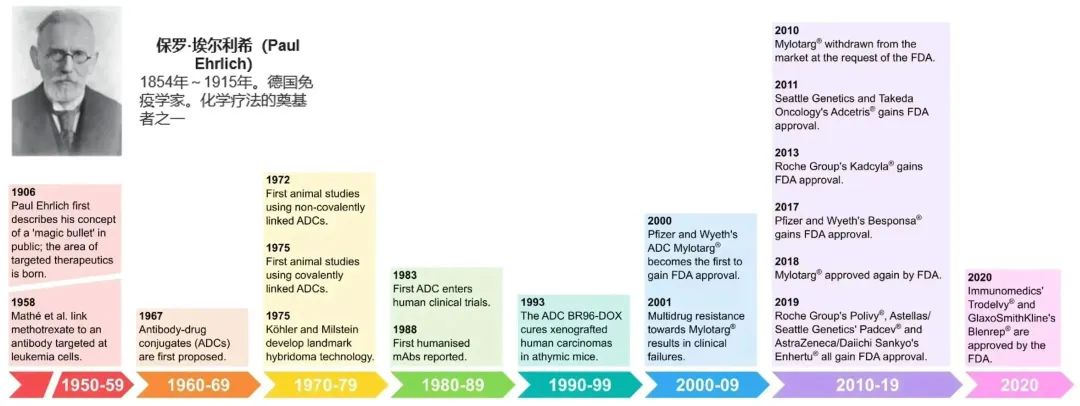
Figure 1. History and milestones of ADC drug development (1906-2020)[1]
1.1 Structure and Mechanism of ADC Molecules
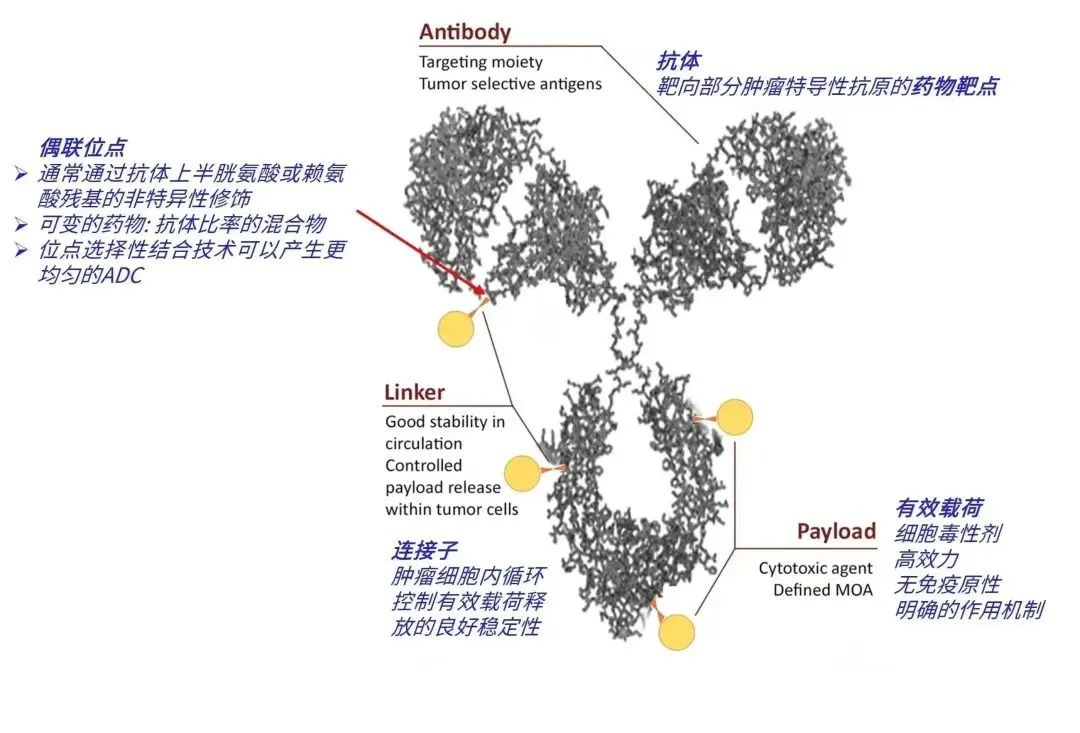
ADC molecules consist of monoclonal antibodies, linkers, and payloads (Figure 2).
Figure 2. Structural illustration of ADC molecules: General structure of ADC molecules composed of monoclonal antibodies (gray) linked with cytotoxic payloads (gold) using cleavable/non-cleavable linkers (orange)[2]
Figure 3 illustrates the main mechanism of action of ADC drugs. ADC molecules enter tumor tissue from the vascular system, bind to tumor cell surface targets, and then internalize through the endosomal-lysosomal pathway, where the linker is cleaved and/or the antibody is degraded to release the payload, which ultimately diffuses into the cytoplasm to reach its target (microtubules), disrupting microtubule dynamics. Other widely used payloads, such as Calicheamicin targeting DNA, must further diffuse from the cytoplasm to the nucleus (not shown in Figure 3)[3].
If the cytotoxic metabolites can freely pass through the cell membrane and diffuse, they can enter adjacent cells and exert a bystander effect.
Figure 3. Mechanism of action of ADCs equipped with payloads (Auristatin, Maytansine)[3]
1.2 Market and Sales of ADC Drugs
The first ADC drug Mylotarg® was approved by the FDA in 2000. Since 2019, the number of approved ADCs has more than doubled, with five ADCs approved between 2019 and 2020.
Table 1. ADC drugs approved worldwide as of 2020[4]
Currently, the sales of approved ADC drugs are showing a good growth trend across various regions globally. From 2016 to 2020, the sales of ADC drugs in the US increased from $329 million to $1.47 billion, with a compound annual growth rate of 45%; the ADC drug markets in Europe and Japan also showed compound annual growth rates of 13% and 21%, respectively[5].
Figure 4. Sales of major ADC markets globally (2016-2020)[5]
In China, six ADC drugs have been approved, among which Yantai Rongchang Biopharmaceutical’s Vadastuximab talirine was approved by the NMPA in June 2021, becoming the first domestically produced ADC new drug.
Mylotarg® (Gemtuzumab ozogamicin) is the first ADC drug approved globally, co-developed by Pfizer and Wyeth, which received accelerated approval from the FDA as early as 2000 for the treatment of first relapse acute myeloid leukemia in patients aged over 60 with CD33+ who are unsuitable for cytotoxic chemotherapy. Shortly after its approval, it was voluntarily withdrawn from the market in June 2010 due to safety concerns. After updating clinical data and adjusting specifications, Mylotarg® was reapproved by the FDA in 2017 after adjusting the original dosing regimen from 9 mg/m2 to 3 mg/m2, marking a successful return after 17 years of refinement[4,6].
Figure 5. Product appearance of Mylotarg® (left, sourced from the internet) and schematic diagram of its molecular structure (right)
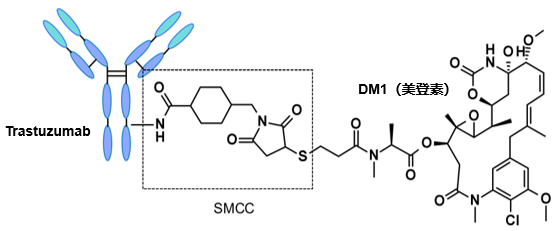
Kadcyla® (Ado-trastuzumab emtansine) was co-developed by Roche and ImmunoGen and was approved by the FDA on February 22, 2013, for the treatment of HER2-positive metastatic breast cancer in patients who have previously received trastuzumab® and taxane chemotherapy, making it the first ADC approved for solid tumors globally. Kadcyla® is a second-generation ADC that utilizes a humanized monoclonal antibody and a more effective cytotoxic drug, reducing immunogenicity and enhancing the potency of the cytotoxic drug.
Clinical studies have confirmed that compared to the control group, the median progression-free survival (PFS) of patients treated with Kadcyla® (9.6 months) showed significant improvement, and the overall survival (OS) also increased (29.9 months vs 25.9 months). In January 2020, this drug was successfully approved in China, becoming the first ADC drug approved for marketing in the country. In 2021, Kadcyla® achieved global sales of $2.18 billion, ranking first in ADC drug sales[4,6].
Figure 6. Product appearance of Kadcyla® (left, sourced from the internet) and schematic diagram of its molecular structure (right)
Considerations in the Pharmaceutical Research of ADC Drugs
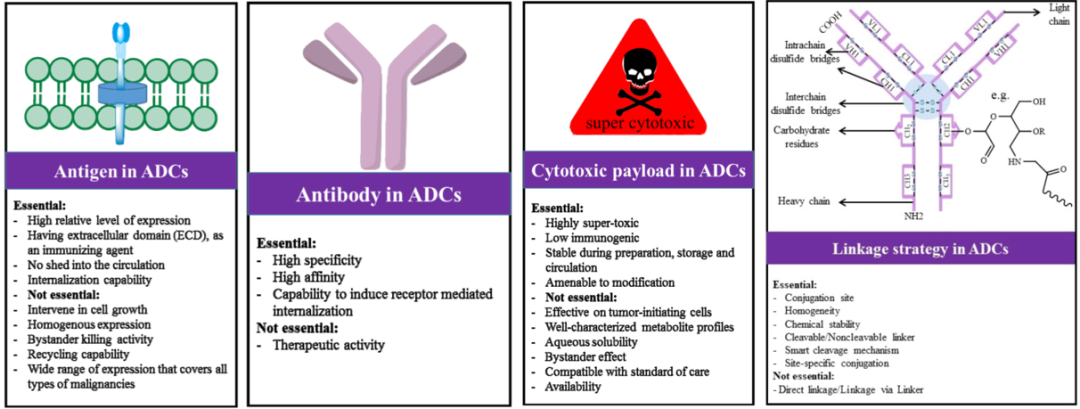
ADC molecules have complex and exquisite structures, and their molecular design needs to consider multiple factors, including antigen, antibody, payload, linker, and coupling strategy[7]. Various specific considerations are shown in Figure 7.
Figure 7. Design considerations for ADC drugs[7]
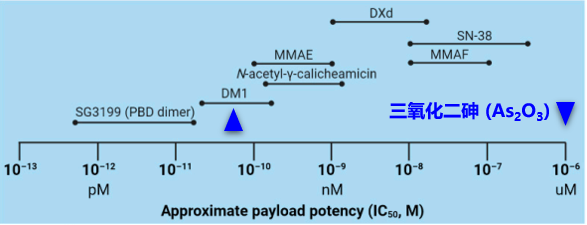
The payload is a key component that enables ADCs to exert cytotoxic effects and must meet several key requirements: (1) High cytotoxicity, typically with an IC50 value at low nanomolar or picomolar levels (see Figure 8); (2) Clear target and mechanism of action; (3) (Potential) chemical attachment sites.
Figure 8. Common effective concentration ranges of ADC payloads
DM1/DM4 derivatives or Auristatin (MMAE/MMAF) are commonly used microtubule inhibitors. Other types of cytotoxic drugs include enediyne (Calicheamicin), maytansine derivatives, pyrrolobenzodiazepines (PBD), and indolinobenzodiazepines, which target the minor groove of DNA; in addition, there are quinoline alkaloids (SN-38) that inhibit DNA topoisomerase I.
In 114 completed or ongoing clinical trials, the drugs used as payloads lack diversity, with only seven payload formulations reported (four additional trials are ongoing, with structures not reported). Six of the seven payload mixtures are derived from natural products, indicating the critical value of natural products in the types of ADC payloads[8,9].
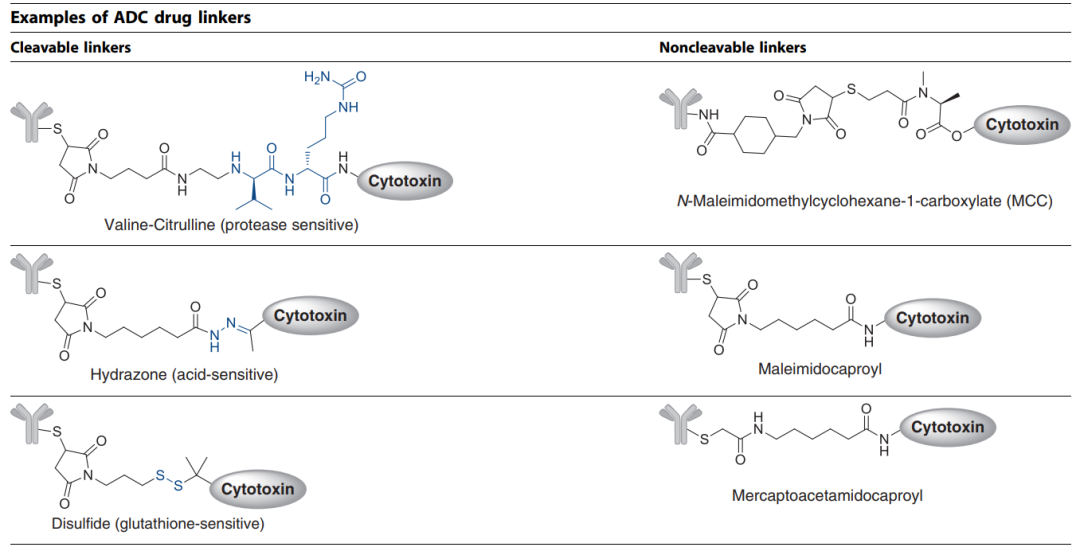
One of the biggest challenges in ADC development is selecting the appropriate linker to attach the cytotoxic payload to the antibody. The chemistry of the linker affects various properties of the ADC, including toxicity, specificity, stability, and potency. Common linker technologies and release mechanisms for ADCs are shown in Table 2.
Table 2. Linker technologies and release mechanisms for ADCs
Linkers can be broadly categorized into cleavable (where the payload can separate from the antibody at the tumor site) or non-cleavable (where the payload and antibody remain linked, with the antibody degrading after internalization), as shown in Figure 9.
Figure 9. Two main types of ADC linkers (cleavable and non-cleavable)[10]
Common cleavable linkers include chemically reactive linkers, acid-labile linkers, reducible chain linkers, and enzyme-cleavable linkers. Non-cleavable linkers release cytotoxic payloads during the lysosomal degradation of antibody-drug conjugates in the tumor environment, bypassing non-specific dispersion of toxic formulations. One advantage of non-cleavable linkers is improved stability in plasma, reducing off-target toxicity.
Mylotarg® used an acid-unstable hydrazone linker strategy. Theoretically, the hydrazone should be stable in blood circulation at physiological pH and undergo selective hydrolysis under more acidic conditions after internalization (the pH of endosomes is 5.0–6.5, and that of lysosomes is 4.5–5.0). However, reports have indicated that the linker of Mylotarg® exhibits some instability, leading to premature release of the payload in plasma circulation, which may cause off-target toxicity. Benefiting from knowledge accumulated in clinical practice in recent years, Pfizer reduced the dosage of this drug and modified the administration scheme, ultimately receiving FDA reapproval in 2017[2,11].
2.3 Drug-Antibody Ratio (DAR)
The average number of effective payload molecules per antibody is commonly referred to as the drug-antibody ratio (DAR). DAR determines the amount of “effective payload” that can be delivered to tumor cells and can directly affect safety and efficacy. High drug loading often leads to rapid plasma clearance, while ADCs with lower DAR exhibit weaker activity.
The design of successful ADCs in clinical practice depends not only on the potency and ratio of the payload, stability of the linker, and release of the payload, but also on the choice of coupling technology.
In the past decade, all ADCs approved by the FDA have been composed of ADC mixtures with different numbers of drugs attached at various positions on the monoclonal antibody. The industry has now developed a range of new coupling strategies aimed at controlling the linkage positions and quantities of the payloads while maintaining structural integrity and homogeneity[5,10].
Figure 10. Random and site-specific coupling strategies: Randomly coupled ADC products include chemical isomers (a), while site-specific coupling methods produce relatively homogeneous product distributions (b)[10]
2.5 Stability of ADC Drugs[12]
The drug concentration in marketed ADC formulations is often below 20 mg/mL, as their high selectivity and efficacy avoid the need for high concentrations. Lower concentrations reduce the risk of aggregation, which is particularly important for ADC molecules with hydrophobic payloads, as the solubility of ADCs may decrease compared to the antibody itself. However, since ADC drugs are often administered via infusion in clinical settings, low concentrations in infusion bags can also pose problems, especially as hydrophobic payloads increase the risk of drug loss due to adsorption to plastic surfaces.
Liquid formulations for ADC products may face stability issues, while lyophilized formulations can reduce linker degradation during storage. Currently, almost all approved ADC drug formulations are in lyophilized form.
Another interesting phenomenon is that some ADC formulations may be more photosensitive than traditional antibodies, such as Mylotarg®, Besponsa®, and Enhertu®, which all use brown vials as their packaging materials.
Table 3. Formulation information for several approved ADC drugs
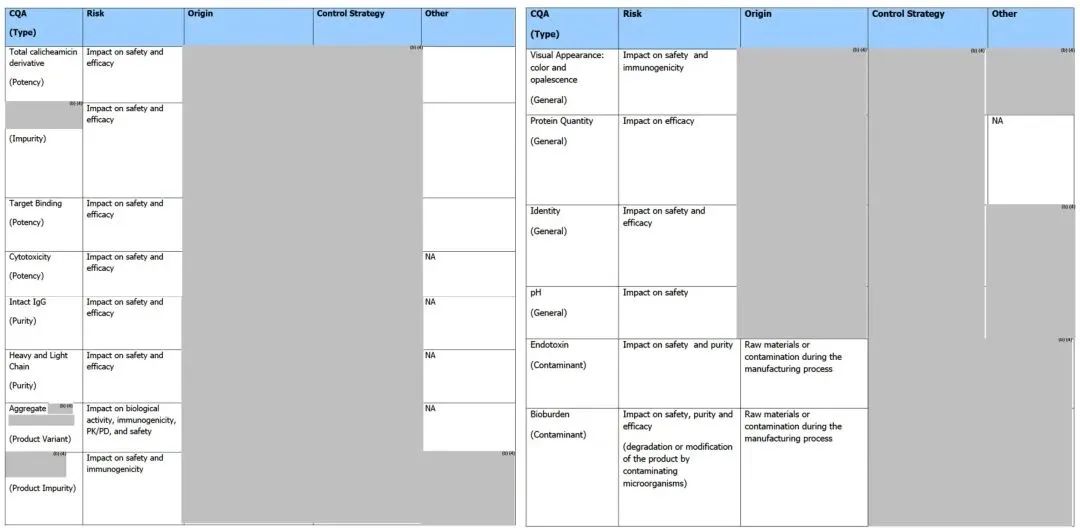
2.6 Key Quality Attributes (CQA) of ADC Drugs
ICH Q8 R2 defines and explains key quality attributes as: “Key quality attributes are physical, chemical, biological, or microbiological properties or characteristics that should be within appropriate limits, ranges, or distributions to ensure the desired product quality (safety, efficacy).” Therefore, understanding the CQA of ADC drugs is of great significance for the development of ADC drugs, and some common key quality attributes of ADC drugs are shown in Table 4.
Table 4. Key Quality Attributes of ADC Drugs (Partial) [13]
Tables 5 and 6 present detailed CQA information for the marketed ADC product Mylotarg® in its raw and finished forms for reference.
Table 5. Raw CQA of marketed ADC product Mylotarg® (FDA Review Report: FDA Product Quality Review Report_BLA 761060 Mylotarg)
Table 6. Finished CQA of marketed ADC product Mylotarg® (FDA Review Report: FDA Product Quality Review Report_BLA 761060 Mylotarg)
Additionally, unlike the information disclosed by the FDA, the EMA marketing review report for Mylotarg® (EMA/155284/2018_ Mylotarg Assessment report) shows that its raw liquid quality standards include general attributes, identification, purity, biological activity, product-related impurities, and safety testing. Moreover, the structural characterization of the raw liquid includes information on post-translational modifications, charge & size heterogeneity, coupling sites, coupling degree of calicheamicin derivatives, higher-order structure, and biological activity.
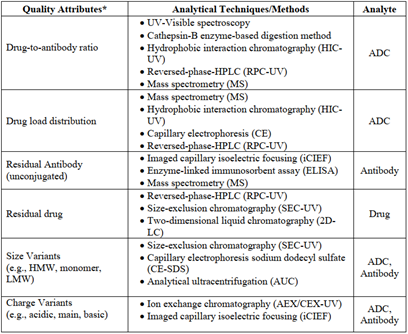
2.7 Analytical Techniques Related to ADC Drugs
Generally, analytical tools used for conventional antibody drugs may also be applicable to ADC drug analysis, but not all methods can be seamlessly switched. For example, if the payload of the ADC has UV absorption or if the sample is highly heterogeneous; or, in size exclusion chromatography (SEC), if the ADC has a hydrophobic payload structure, it may require the addition of organic solvents to the mobile phase to reduce strong hydrophobic interactions with the chromatography column.
Here are several unique quality attribute analyses for ADC drugs:
Determination of Drug-Antibody Ratio (DAR)
UV-visible spectroscopy is a simple and practical determination method, but it has prerequisites for use: 1) The payload should contain a UV-visible chromophore; 2) The payload and antibody should exhibit distinct and separated maximum absorption peaks in their UV-visible spectra; 3) The presence of the payload should not affect the absorption characteristics of the antibody portion, and vice versa.
Hydrophobic interaction chromatography (HIC) relies on the number of hydrophobic payloads attached to the antibody to separate conjugates. The least hydrophobic unconjugated antibody is eluted from the column first, while the conjugate with the highest DAR is eluted last. Besides DAR, this method can also provide information on the conjugation level of ADCs, making it a classic chromatographic technique for ADC drug analysis.
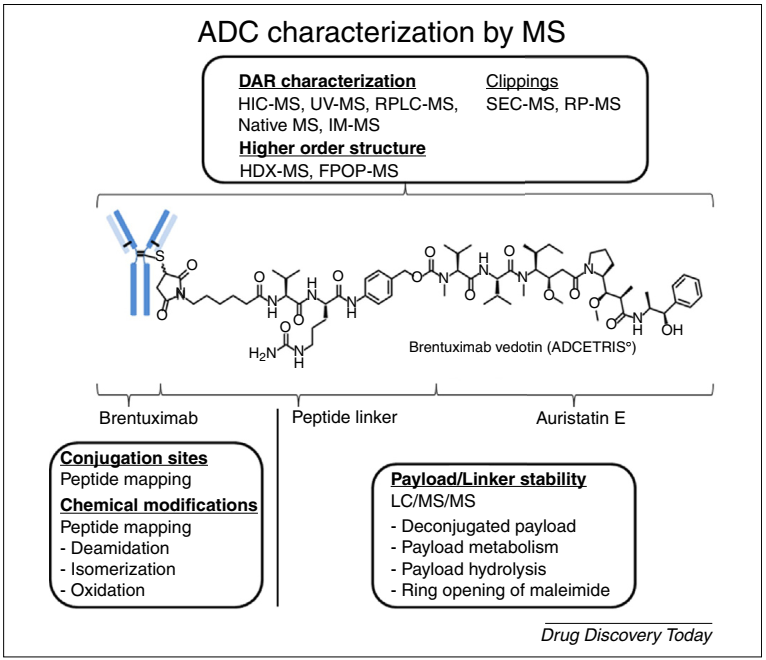
Mass spectrometry is a powerful technique for characterizing the structure of ADCs, allowing for the separation, identification, and quantification of molecular species, and can also be used to determine DAR.
Determination of Payload Distribution
The overall payload distribution can be analyzed via mass spectrometry for complete molecular weight analysis, and for ADCs with less heterogeneity produced through cysteine or other site-specific coupling, hydrophobic interaction chromatography can also be used for characterization. To determine the payload distribution at each conjugation site, more comprehensive analyses such as reduced mass spectrometry peptide mapping are required.
Reversed-phase high-performance liquid chromatography (RPC) or capillary electrophoresis (CE) can provide information on the distribution of payloads on the light and heavy chains under reducing conditions as orthogonal testing methods.
Determination of Unconjugated Antibody
The level of unconjugated antibody is a key parameter in process control, as it can directly affect the efficacy of ADC drugs. Mass spectrometry is a commonly used tool for the quantification of unconjugated antibodies. Due to the inherent lipophilicity of the payload or linker, the binding of (hydrophobic) payloads can also change the hydrophobicity of the protein molecules, thus hydrophobic interaction chromatography can also be used to determine the levels of unconjugated antibodies in ADC samples.
Because the binding of the payload to the antibody can greatly alter the surface and overall charge distribution, techniques such as intact column imaging capillary isoelectric focusing (icIEF) can also be considered as alternative analytical tools. Other methods worth trying include: reversed-phase high-performance liquid chromatography, capillary electrophoresis, enzyme-linked immunosorbent assay (ELISA), etc.
It is worth mentioning that mass spectrometry analysis technology is a powerful tool for structural characterization of ADC drugs, playing an indispensable role in applications such as ADC drug process development and quality analysis. Common uses of mass spectrometry in ADC drug quality analysis are detailed in Figure 11.
Figure 11. Mass spectrometry-based structural characterization strategies for ADCs: Deep characterization can be performed on intact ADCs, monoclonal antibodies, cytotoxic payloads, or linker structures[14]
2.8 Process Development and Production of ADC Drugs[15]
Compared to any other active pharmaceutical ingredient (API) category, the quality of ADC drugs is more constrained by the manufacturing process. A well-established production process is essential to reproducibly produce a heterogeneous subset of compounds. To ensure process consistency, numerous parameters of the coupling process need to be studied and controlled. The selection of appropriate processing, storage, and handling conditions during production should be based on the physicochemical stability study data of intermediates and ADCs.
Refined process development also requires experienced and well-trained personnel, along with suitable experimental equipment.
To conduct more experiments with minimal materials, mini-jacketed vessels for coupling experiments at milligram scale have proven to be very useful, as this reaction model has been shown to simulate reaction performance at scales of hundreds of liters; however, for purification processes, gram-scale operations are required to assess tangential flow filtration (TFF) conditions.
The biggest challenge in ADC drug production may be the design, construction, and operation of a biomanufacturing environment that allows for the safe handling of potent cytotoxic drugs and their contaminants (e.g., transfer of materials containing toxic substances, disposal of contaminants). Therefore, personnel training should be strengthened to ensure proper use of equipment and adherence to safety concepts; additionally, a personal protective equipment plan should be established to cover residual risks that engineering controls cannot eliminate, as well as emergency plans for toxic compound spills.
Cleaning of equipment is another critical activity in the manufacture of potent cytotoxic drugs. Disposable technologies can reduce cleaning operation costs, but materials are often expensive, and leachable and extractable data may also need to be provided. Therefore, glass or stainless steel containers are typically preferred for coupling reactions.
Cleaning validation of ADC production lines requires highly sensitive detection methods, as traditional TOC and HPLC methods for detecting residual cytotoxic agents may not provide sufficient sensitivity, and may require the use of validated ELISA or LC-MS analytical methods.
Prospects and Challenges of ADC Drugs
Despite the complex design of ADCs, the prospects of this therapeutic topic have attracted great interest in recent decades. The robust pipeline of ongoing clinical research and the continuously approved ADC drugs are the best evidence of a bright future[10]. In addition to the current widespread application in oncology, the ADC concept also has potential applications in other therapeutic areas, such as treating methicillin-resistant Staphylococcus aureus infections, vancomycin-resistant intracellular Staphylococcus aureus infections, or anti-inflammatory[1].
The preclinical lead selection methods for ADC candidates typically rely on systematic in vitro evaluations of various antibodies, linkers, and cytotoxic payloads, while it remains to be seen whether in vitro models are sufficient to predict drug responses. Early in vivo studies may be crucial before further understanding ADCs[10].
One of the main challenges for ADC drugs is off-target toxicities, resulting from the premature release of cytotoxic small molecules into the bloodstream. Clinically reported off-target toxicities include hepatotoxicity, thrombocytopenia, peripheral neuropathy, neutropenia, anemia, and ocular toxicity, among others. Additionally, the complex potential mechanisms of drug resistance in ADCs remain to be elucidated; and identifying resistance mechanisms to ADCs in the context of combination therapies with other administered compounds presents a significant challenge[10,11,16].
Although there are many challenges in the design, process, and product development and clinical practice of ADC drugs, more clinical trials and basic research on existing ADCs will pave the way for addressing issues related to tumor markers, antibodies, cytotoxic payloads, and coupling strategies, making the future of ADC drugs promising.
About Yian Jishi’s ADC Process Development Service
The ADC development laboratory of Hangzhou Yian Jishi Biopharmaceuticals officially started operation in September 2023 and can undertake various ADC drug development work at the laboratory scale. We welcome both new and old partners to contact us:
Small-scale preparation of ADC materials based on lysine or cysteine coupling
Development, optimization, and transfer of ADC coupling and purification processes
Preparation of toxicology batch ADC materials
Development of ADC formulations and lyophilization processes
Development, validation, and transfer of ADC analytical methods
Structural and functional characterization and stability studies of ADC products
Preparation of submission documents (M2 and M3 modules) and registration support
Figure 12. Some equipment in the ADC laboratory of Hangzhou Yian Jishi Biopharmaceuticals
[1] Antibody–Drug Conjugates—A Tutorial Review. Molecules 2021, 26, 2943
[2] Antibody-Drug Conjugate-Based Therapeutics: State of the Science. JNCI J Natl Cancer Inst (2019) 111(6): djz035
[3] Antibody–Drug Conjugates for Cancer Treatment. Annu. Rev. Med. 2018. 69:191–207
[4] The Chemistry Behind ADCs. Pharmaceuticals 2021, 14(5), 442
[5] “Pharmaceutical Economic Report”
2021.08.30. http://www.yyjjb.com.cn/yyjjb/202108/202108301543244324_10892.shtml
[6] Antibody–Drug Conjugates—A Tutorial Review. Molecules 2021, 26, 2943
[7] Antibody-Drug Conjugates: Possibilities and Challenges. Avicenna Journal of Medical Biotechnology, Vol. 11, No. 1, January-March 2019
[8] Introduction to Antibody-Drug Conjugates. Antibodies 2021, 10, 42
[9] An Insight into FDA Approved Antibody-Drug Conjugates for Cancer Therapy. Molecules 2021, 26, 5847
[10] Antibody–drug conjugates: current status and future directions. Drug Discovery Today, Volume 00, Number 00, Dec 2013
[11] Antibody–Drug Conjugates: The Last Decade. Pharmaceuticals 2020, 13, 245
[12] Antibody-drug conjugates- stability and formulation. European Journal of Pharmaceutics and Biopharmaceutics 139 (2019) 168–176
[13] Challenges and new frontiers in analytical characterization of antibody-drug conjugates. MAbs. 2018 Feb/Mar;10(2):222-243
[14] Characterization of antibody–drug conjugates by mass spectrometry: advances and future trends. Drug Discovery Today, Volume 00, Number 00, April 2016
[15] Chapter 29: Challenges in the Development and Manufacturing of Antibody–Drug Conjugates,489-497
[16] Advances and Limitations of Antibody Drug Conjugates for Cancer. Biomedicines 2021, 9, 872