
Antibody-drug conjugates (ADCs) are formed by linking monoclonal antibodies that target specific antigens with small molecule cytotoxic drugs through linkers, combining the powerful killing effect of traditional small molecule chemotherapy with the tumor targeting ability of antibody drugs.ADCs consist of three main components: the antibody responsible for selectively recognizing cancer cell surface antigens, the drug payload responsible for killing cancer cells, and the linker that connects the antibody and the payload.
ADCs have become a popular class of drugs for treating hematologic malignancies and solid tumors, undergoing extensive preclinical and clinical research. However, like most cytotoxic drugs, the duration of objective responses or clinical benefits from ADCs as a monotherapy is still limited due to the emergence of resistance mechanisms. Therefore, combinations of ADCs with other anticancer drugs have become an important direction in ADC drug development.
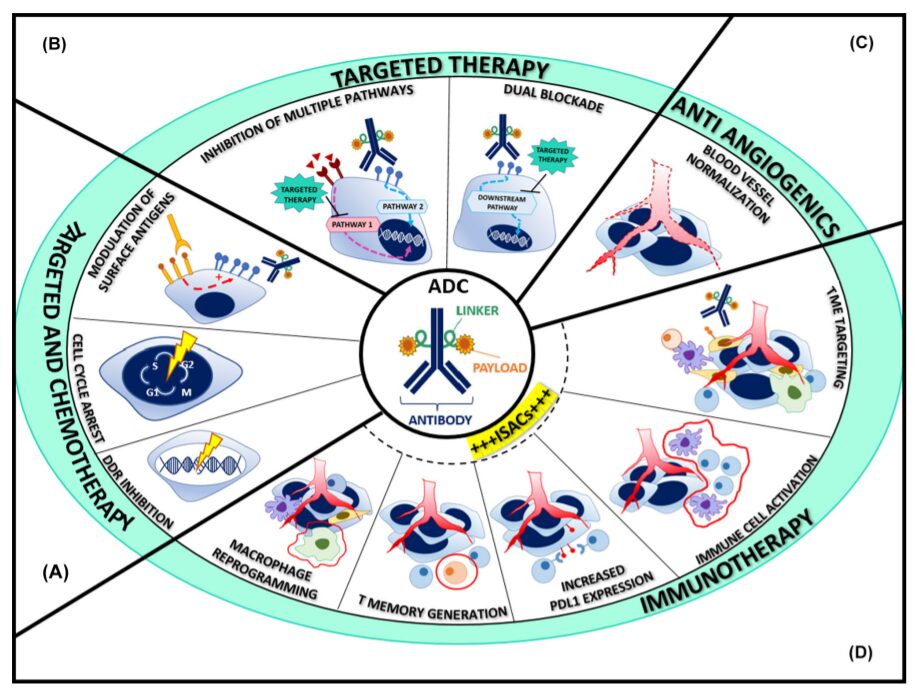
Currently, regulators have approved combinations of ADCs with chemotherapy/chemotherapy-immunotherapy for hematologic tumors, and the FDA has granted breakthrough therapy designation for enfortumab vedotin and pembrolizumab. The most attractive drugs to combine with ADCs are those that have additive or synergistic effects on tumor cells or their microenvironment without unacceptable overlapping toxicities. Combinations with anti-angiogenic drugs, HER2-targeted drugs, DNA damage response agents, and immune checkpoint inhibitors (ICIs) are currently actively researched directions.
ADC Combination Chemotherapy
The optimal combination of ADCs with chemotherapy drugs requires a better understanding of the unique cell cycle interactions and the regulation of surface antigen expression by cytotoxic partners. So far, an increasing number of preclinical and clinical data show good application prospects and provide valuable insights for guiding further drug development.
Cell Cycle Interactions
DNA damaging agents that act on the S phase and cause G2/M phase arrest (such as antimetabolites, platinum, and topoisomerase inhibitors) can be combined with microtubule inhibitors. The successful combination of carboplatin with mirvetuximab soravtansine, anetumab ravtansine, or luveltamab tazevibulin in ovarian cancer models illustrates this concept. In early clinical trials, ADCs based on ravtansine combined with carboplatin or doxorubicin showed significant efficacy in platinum-sensitive and resistant ovarian cancer patients, as well as ADCs based on deruxtecan combined with capecitabine or cisplatin in gastric and lung cancer patients.
Design of Administration Timing
Administration timing may relate to the design of drug combinations. Microtubule protein polymerization is a key component of the ADC internalization mechanism, and the G2/M phase arrest mediated by DNA damage may require some time for microtubule disruption sensitization to occur. Studies in colorectal, lung, and breast cancer models have well demonstrated this, where continuous administration of SGN-15 (Lewis Y antigen-doxorubicin) and paclitaxel caused more DNA fragmentation than simultaneous administration. This observation suggests that adjusting the administration timing, particularly delaying the administration of DNA damaging agents after anti-microtubule drugs, could enhance therapeutic efficacy.
Regulation of Surface Antigens
Chemotherapy drugs can regulate the expression of surface antigens targeted by ADCs. In this regard, gemcitabine has been shown to upregulate HER2 expression in pancreatic adenocarcinoma cells, where the combination of gemcitabine and trastuzumab emtansine exhibited enhanced potency. Intertwined with the aforementioned cell cycle interactions, HER2 upregulation occurs particularly in the G2/M population, resulting from gemcitabine-mediated DNA synthesis inhibition.
Overlapping Toxicities
ADCs are essentially chemotherapy; therefore, the efficacy improvement of combination regimens is often hindered by unacceptable toxicities. Major toxicities are driven by the metabolites of cytotoxic payloads, which must be carefully considered when designing combination strategies. These toxicities include peripheral neuropathy caused by MMAE and DM1 derivatives, ocular toxicity caused by MMAF and DM4, gastrointestinal effects of DM1 or topoisomerase inhibitors, or hepatotoxicity caused by calicheamicin derivatives, along with nearly universal neutropenia and thrombocytopenia.
Two phase 2a/b studies demonstrated this, investigating the combination of trastuzumab emtansine with docetaxel or paclitaxel in HER2+ advanced breast cancer, where more than half of the patients needed dose reductions or discontinuation of taxanes. Newer, more tumor-selective ADCs, such as mirvetuximab soravtansine and datotomab deruxtecan, show milder toxicities, making them ideal partners for chemotherapy drugs with different mechanisms of action.
ADC Combination Targeted Drugs
Compared to standard chemotherapy, ADCs have improved therapeutic indices and increased activity against selective tumor populations, making them ideal partners for targeted drugs. Various combination strategies can be envisioned to overcome treatment resistance and clonal heterogeneity, invoke stronger inhibition of oncogene-dependent signaling pathways, increase the availability of surface antigens, and make low antigen-expressing tumors sensitive, while modulating the tumor microenvironment.
Replacing Chemotherapy with ADCs
So far, many studies have attempted to replace standard chemotherapy with ADCs as combinations with targeted drugs, but the results have been disappointing. Clinical trials such as KAITLIN, KRISTINE, and MARIANNE were designed based on the synergistic antitumor activity of trastuzumab emtansine combined with pertuzumab; however, they did not show enhanced efficacy compared to paclitaxel, trastuzumab, and pertuzumab in neoadjuvant and metastatic settings. Similarly, in ovarian cancer, the efficacy of combining anetumab ravtansine with bevacizumab was lower than that of paclitaxel.
Tyrosine Kinase Inhibitors (TKIs)
Dual-target blockade by adding TKIs can provide greater selectivity and potentially improve therapeutic indices. In the TEAL study, the combination of trastuzumab emtansine, pan-HER2 inhibitor lapatinib, and albumin-bound paclitaxel showed improved responses in neoadjuvant therapy for HER2+ breast cancer patients compared to standard paclitaxel, trastuzumab, and pertuzumab. The combination of trastuzumab emtansine and tucatinib (a more selective anti-HER2 TKI) achieved a 47% objective response rate (ORR), including a 36% brain-specific response rate in patients with advanced disease who progressed after prior taxane and trastuzumab treatment. Next-generation ADCs and TKIs may yield better outcomes.
Targeting ADC Resistance
Increasing evidence supports that targeted drugs can simultaneously target known ADC resistance mechanisms. For example, as HER2-dependent malignant transformation of breast epithelial cells relies on cyclin D1, CDK4/6 inhibitors have been used in combination with trastuzumab emtansine in HER2-resistant patients. Additionally, another key cell cycle regulator, PLK1, has recently been identified as an upregulated target in acquired and primary trastuzumab emtansine-resistant models, with its inhibitor volasertib resensitizing trastuzumab emtansine in vitro and in vivo. On the other hand, ADCs may also be effective combinations for modulating targeted drug resistance mechanisms. For instance, the combination of osimertinib and trastuzumab emtansine produced additional antitumor effects, where trastuzumab emtansine was able to delay or overcome resistance to osimertinib in EGFR-mutant non-small cell lung cancer models.
Regulation of Surface Antigens
Some TKIs have been shown to regulate surface antigens, potentially promoting further ADC activity and making low antigen-expressing tumors sensitive. In this regard, lapatinib, neratinib, tucatinib, and poziotinib have been shown to enhance the efficacy of trastuzumab emtansine. However, the specific mechanistic principles remain unclear. Among them, lapatinib increases HER2 abundance through strong transcriptional upregulation and reduction of ubiquitination, neratinib decreases surface HER2 abundance by stimulating internalization and endocytosis, the effects of tucatinib on cell surface HER2 remain elusive, while poziotinib upregulates exon 20 mutations without upregulating wild-type HER2, indicating that the synergistic mechanism is unrelated to surface HER2 density.
Anti-Angiogenesis
Anti-angiogenic agents can promote ADC penetration and tumor cell exposure. The combination of anetumab ravtansine or mirvetuximab soravansine with bevacizumab showed complete response efficacy in preclinical models of ovarian cancer. A recent phase 1b study combined mirvetuximab soravansine and bevacizumab for heavily pretreated, platinum-resistant, FRα-high ovarian cancer patients, where 39% ORR exceeded the benchmark of the pivotal AURELIA trial (27%).
DNA Damage Response Agents
Developing synthetic lethality by combining drugs targeting DNA damage response (DDR) with ADCs carrying DNA damaging agents may be a promising strategy for treating genomically unstable tumors.
Traditionally, the combination of DDR drugs with chemotherapy has been hindered by intolerable toxicities, while the superior activity and tolerability of next-generation ADCs carrying topoisomerase I inhibitor payloads make them more suitable as partners. Several clinical trials are exploring this strategy, including niraparib and trastuzumab duocarmazine, talazoparib and sacituzumab govitecan, as well as olaparib and trastuzumab deruxtecan. In addition to PARP inhibitors, the selective increase of ADCs against chemotherapy will undoubtedly expand the range of combinable DDR drugs, such as the ongoing clinical trial of the ATR inhibitor berzosertib combined with sacituzumab govitecan (NCT04826341).
ADC Combination Immunotherapy
Combination strategies of immunotherapy and ADCs have recently entered clinical trials. Although preclinical data and results from early clinical studies indicate enhanced antitumor activity, randomized clinical trial results supporting this approach over standard treatment are still awaited.
Anti-PD-1/PD-L1 and Anti-CTLA-4 Antibodies
Increasing evidence suggests that ADCs may enhance the efficacy of immunotherapeutic agents. The mechanisms involved are diverse, including enhancing immune memory and the expression of immune regulatory proteins (such as PD-L1 and MHC). Some ADCs have shown greater efficacy in preclinical models with intact immune systems, supporting their immunomodulatory function.
Multiple HER2-targeted ADCs, including trastuzumab emtansine, trastuzumab deruxtecan, and disitamab vedotin, have been tested in vitro and in vivo in combination with ICIs, confirming synergistic activity associated with enhanced homing and immune effector activation. The KATE2 study is the only published randomized trial testing ADC plus ICI, comparing the efficacy of trastuzumab emtansine combined with atezolizumab versus trastuzumab emtansine combined with placebo in pretreated HER2+ breast cancer patients. The combination therapy failed to improve progression-free survival (8.2 vs 6.2 months, P=0.33), indicating that adding ICIs to HER2-targeted therapy may only benefit the PD-L1 positive population. Despite disappointing results observed in this randomized trial, clinical explorations in various tumors are still ongoing.
Moreover, increasing preclinical evidence suggests that combination therapies may restore immune sensitivity. For instance, in models of ICI-refractory melanoma and non-small cell lung cancer (NSCLC), the AXL-specific ADC enapotamab vedotin was tested in combination with anti-PD-1 antibodies, where the ADC enhanced ICI activity by inducing T cell infiltration and enhancing antigen presentation, leading to pro-inflammatory changes in the TME.
ADC Combination with Other Immunotherapies
Polatuzumab vedotin has been shown to enhance CD20 expression on tumor cells through increased AKT and ERK signaling, supporting its combination with anti-CD20 antibodies (such as rituximab) and CD20/CD3 bispecific antibody therapies. Additionally, combinations of ADCs and immunomodulators are also being explored in other diseases, such as multiple myeloma. In preclinical models, the combination of belantamab mafodotin with OX40 agonists generated synergistic antitumor activity, increasing the infiltration and activation of T cells and dendritic cells within tumors. Belantamab mafodotin combination regimens, such as the DREAMM-5 study (NCT04126200), are actively being investigated in clinical settings, combining with various immunotherapeutic agents including (anti-ICOS antibodies, OX40 agonists, and γ-secretase inhibitors) as well as anti-PD-1 antibodies. Preliminary results indicate good activity of the combination with anti-ICOS antibodies in heavily pretreated patients.
Furthermore, ADC designs can target not only cancer cells but also elements of the TME, such as immune cells or fibroblasts, thereby altering immune responsiveness. For instance, ADCs targeting CD73 have shown encouraging preclinical activity. Additionally, when used in combination with pembrolizumab in preclinical models, ADCs targeting cancer-associated fibroblasts have demonstrated enhanced CD8+ T cell-mediated antitumor activity.
As monotherapies, ADCs have demonstrated antitumor efficacy and have been approved for various solid tumors and hematological malignancies. Both academia and industry are currently engaged in extensive efforts to develop the next generation of ADCs by identifying new targets and enhancing their pharmacological effects, as well as combination therapies based on current ADCs.
However, thus far, the success of combination approaches using first- and second-generation ADCs has been limited, which may be attributed to several factors, such as non-specific expression of targets leading to adverse reactions in normal tissues, overlapping toxicities, insufficient efficacy across different tumor clones, and emerging resistance mechanisms. Therefore, a profound understanding of the pharmacology of ADCs and related predictive biomarkers is needed, along with preclinical evaluations in well-characterized patient-derived xenograft models, to select the most promising ADC-based combinations. It is believed that future ADC-based combination therapies will show bright prospects.
References:
1. Antibody-drug conjugates: in search of partners of choice. Trends Cancer. 2023 Feb 4
Disclaimer
The push rules of the WeChat public account have changed again. If you don’t click on “Looking” or haven’t marked it as “Starred”, we may just disappear into the vast sea of articles~ Click here, don’t miss the latest news from DuDu!👇👇👇