
Antibody-drug conjugates (ADC) are formed by linking monoclonal antibodies targeting specific antigens with small molecule cytotoxic drugs through linkers, combining the powerful killing effect of traditional small molecule chemotherapy with the tumor targeting ability of antibody drugs. Since the first ADC, Gemtuzumab-ozogamicin (brand name: Mylotarg), was approved for the treatment of CD33-positive acute myeloid leukemia, several ADCs have been developed for cancer treatment.
The entire development process of ADCs, from selecting the appropriate antibody to the final product, is a daunting and challenging task. Clinical pharmacology is one of the most important tools in drug development, and utilizing this tool helps to find the optimal dose of the product, thereby maintaining the safety and efficacy of the product in the patient population. Unlike other small molecules or macromolecules that typically measure only one component and/or metabolite for pharmacokinetic analysis, ADCs require the measurement of multiple components to characterize their PK characteristics. Therefore, a deep understanding of the clinical pharmacology of ADCs is crucial for selecting a safe and effective dose in patient populations.
Pharmacokinetics is an indispensable part of clinical pharmacology and modern drug development. The main purpose of pharmacokinetic studies is to obtain information about the drug’s absorption, volume of distribution, clearance rate, half-life, accumulation after multiple doses, and the effects of various disease states, age, weight, and sex on drug pharmacokinetics. These pharmacokinetic parameters can be used to design the optimal dosing regimen for patients.
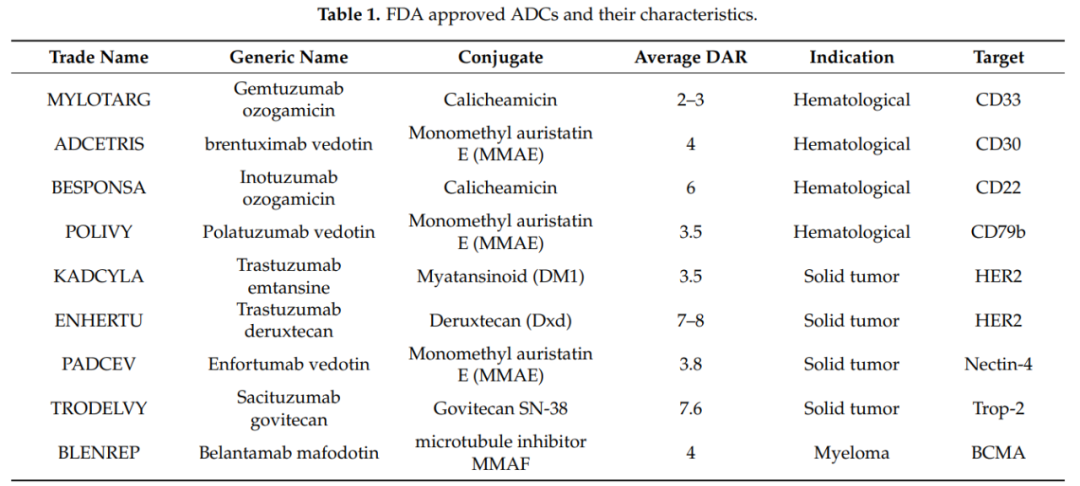
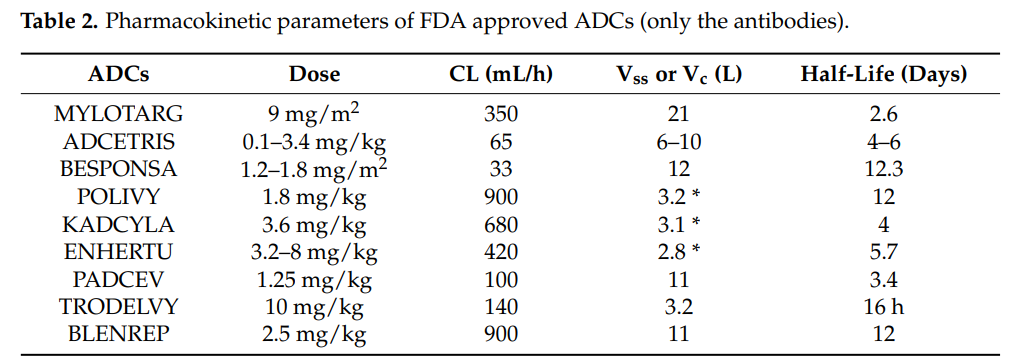
It should be recognized that, unlike small molecules and therapeutic proteins (antibodies or fusion proteins), the PK of ADCs is very complex because ADCs consist of several components. Not only the PK of the monoclonal antibody needs to be considered, but also the PK of the cytotoxic molecule and the physicochemical properties of the conjugate. Since the molecular weight of the monoclonal antibody accounts for over 90%, the PK of different components of the ADC is greatly influenced by its PK. The overall PK characteristics (ADC+mAb) provide the best assessment of ADC stability and integrity. The conjugate and the conjugation site also play an important role in maintaining the stability and PK of ADCs. The following table lists the FDA-approved ADCs and their PK characteristics.
Generally speaking, four processes are involved in the body after administration. These processes are absorption, distribution, metabolism, and elimination.
Absorption
Most antibodies are usually administered via intravenous injection or infusion, and antibodies can also be administered subcutaneously (SC). However, for ADCs, the current administration route is intravenous injection or infusion. Due to the response to the cytotoxic payload and the local deposition of cytotoxic substances, SC administration may not be suitable for ADCs.
Distribution
The distribution of drugs in the body can be described by the volume of distribution. Due to their size and polarity, the distribution of antibodies and ADCs is usually limited to the vascular and interstitial spaces.
The initial distribution of ADCs is generally limited to the vasculature, and their volume of distribution is generally equal to blood volume. Subsequently, ADCs can distribute into the interstitial space. Additionally, the distribution of ADCs is also influenced by the expression of target antigens and endocytosis.
The distribution and accumulation of ADCs in the same tissue can produce adverse (toxic) pharmacological effects due to the release of cytotoxic drugs or metabolites after ADC uptake.
Metabolism
The breakdown/metabolic processes of ADCs in the body include the metabolic processes of the antibody and the metabolic processes of the small molecule drug. Before reaching tumor cells, ADCs release effector molecules either intracellularly (non-cleavable linker) or in the circulation (cleavable linker), and unbound antibodies and antibody fragments follow the metabolic pathways of antibodies to produce amino acids through enzymatic hydrolysis, which are reused by the body.
The free small molecule drugs and/or small molecule drug metabolites linked with amino acid residues that may be formed after the cleavage or metabolic breakdown of ADCs will further undergo hepatic CYP450 enzyme metabolism and may also experience potential drug-drug interactions.
In addition to the intrinsic properties of ADCs, the expression of antigens, receptor/cell density, FcRn-mediated recycling, interactions with Fcγ, receptor-mediated endocytosis, and immunogenicity will also affect the metabolism of ADCs.
Elimination
ADCs are eliminated through metabolic breakdown and excretion. ADCs can enter lysosomes through specific pathways that bind to their targets, where they undergo degradation, releasing small molecule drugs for elimination from the body; they can also be cleared through non-specific pinocytosis, a process involving the neonatal receptor (FcRn) participating in the recycling process.
ADCs, antibodies, large molecular peptides, and amino acid fragments cannot be excreted through glomerular filtration but are reabsorbed and utilized in the form of amino acids. Free small molecule drugs, small molecular peptides, small molecule drugs linked with amino acids, and small molecular antibody fragments can be excreted through glomerular filtration. At the same time, small molecule drugs and metabolites can also be eliminated through enzymatic metabolism or excreted into feces via transporters.
ADCs consist of several components, and to characterize the PK characteristics of these components, several analytical methods are required, as described below:
-
ELISA immunoassays to determine the kinetics of conjugates and total antibodies;
-
TFC-MS/MS for quantification of free drugs/metabolites;
-
High-resolution mass spectrometry for in vivo drug-antibody ratio (DAR) analysis.
Additionally, two types of ELISA immunoassays are used to quantitatively measure analytes of ADCs: the first type measures total antibodies, i.e., ADCs with a DAR greater than or equal to zero. The second analytical method measures drug-conjugated antibodies, defined as ADCs with a DAR greater than or equal to 1.
Other analytical methods include size exclusion chromatography (SEC) and hydrophobic interaction chromatography (HIC). SEC is the most commonly used liquid chromatography (LC) technique for determining the aggregation of antibodies, and this technique can also be used for ADCs. Although HIC is a traditional technique for protein separation, purification, and characterization, it is now being used for ADC characterization and analysis.
The cytotoxic payload of ADCs should possess the following characteristics:
-
The cytotoxic payload should have appropriate lipophilicity.
-
The target of the payload should be located inside the cell.
-
The molecules of the payload should be small in size, lack immunogenicity, and be soluble in aqueous buffers to facilitate easy conjugation.
-
The payload should be stable in the bloodstream.
Currently, commonly used cytotoxic drug effect molecules include microtubule inhibitors (such as auristatins, maytansinoids), DNA damaging agents (such as calicheamicin, duocarmycins, anthracyclines, pyrrolobenzodiazepine dimers), and DNA transcription inhibitors (Amatoxin and Quinolinealkaloid (SN-38)). Several ADC drugs that have been approved for market use employ six different small molecules, of which three ADC drugs utilize MMAE as the conjugated drug, two drugs use Calicheamicin as the conjugated drug, and others successfully applied include MMAF, DM1, SN-38, and Dxd.
The drug-antibody ratio (DAR) refers to the average number of payload molecules attached to a single monoclonal antibody, typically between 2 and 4 molecules. In rare cases, using hydrophilic linkers, payloads can safely achieve a DAR of up to 8, as seen with Enhertus and Trodelvys. DAR is crucial for assessing the efficacy of ADCs; additionally, DAR may affect the drug’s stability in circulation, PK, and toxicity of the ADC.
Studies have shown that ADCs with high DAR values (7 to 14) clear faster and have reduced in vivo efficacy compared to ADCs with DAR values < 6.
The DAR value and its impact on stability and PK also depend on the conjugation site and the size of the linker.
Lysine or cysteine is typically modified to produce ADCs. Lysine is one of the most commonly used amino acid residues for linking substrates to antibodies, as it is usually present on the surface of antibodies and therefore readily conjugated. Mylotargs, Kadcylas, and Besponsas all use lysine bioconjugation technology.
Other amino acids such as cysteine and tyrosine can also be modified, with maleimide-modified cysteine used to synthesize ADCs such as Adcetriss, Polivys, Padcevs, Enhertus, Trodelvys, and Blenreps.
The linker is an indispensable part of ADCs, determining the drug release mechanism, PK, therapeutic index, and safety of the ADC. Early ADC linkers were chemically unstable, such as disulfides and hydrazones. These linkers were unstable in circulation, with short half-lives generally ranging from one to two days. The latest generation of linkers is more stable in systemic circulation, such as peptide and glucuronic acid linkers. The two most common linkers are as follows:
Cleavable Linkers
Cleavable linkers are sensitive to the intracellular environment, releasing free effector molecules and antibodies through metabolic breakdown and dissociation in the cell, such as acid-cleavable linkers and protease-cleavable linkers. They are generally stable in blood but rapidly cleave in low pH and protease-rich lysosomal environments, releasing effector molecules. Additionally, if the effector molecules can cross membranes, they can eliminate tumors by exerting potential bystander effects.
Non-Cleavable Linkers
Non-cleavable linkers are a new generation of linkers that provide better plasma stability compared to cleavable linkers. Because non-cleavable linkers can offer greater stability and tolerance than cleavable linkers, these linkers reduce off-target toxicity and provide a larger therapeutic window.
In 11 clinical trials involving 8 ADCs, the baseline incidence of ADAs ranged from 1.4% to 8.1%, and the incidence of post-baseline ADAs ranged from 0% to 35.8%, values that fall within the range of therapeutic monoclonal antibodies. Overall, the incidence of ADAs in patients targeting hematological malignancies is lower than in those targeting solid tumors; most ADAs are against the monoclonal antibody domain of the ADC. Additionally, in most patients, the semi-antigenic structures of these ADCs do not pose a greater risk of immune response than therapeutic monoclonal antibodies.
Applying modeling approaches can integrate PK, efficacy, and safety data to meet the needs of various stages of ADC drug development, such as: target selection, antibody affinity, linker stability, extrapolation from animals to humans, dose selection and adjustment, exposure-response relationships (exposure-response relationships), DDI studies, etc. Due to the multiple clearance pathways of ADCs (dissociation and metabolic breakdown) and the complex PK characteristics of multiple analytes, their kinetic models are also complex.
Different models have different applications, such as using two-compartment models and PBPK models to describe the stability characteristics of ADCs using parameters like clearance rate, dissociation, and metabolic rate. Currently, non-compartmental models, population pharmacokinetic models, mechanism-based models, and physiology-based models are all applied in ADC pharmacokinetic studies.
Clinical pharmacology plays a very important role in the development process of ADC drugs. Through the continuously evolving bioanalytical techniques, a comprehensive elucidation of the PK/PD characteristics of ADC drugs is crucial for promoting the development of ADC drugs with lower toxicity and higher efficacy. ADC drugs will also undoubtedly demonstrate more powerful advantages in the field of cancer treatment.
References:
1. Clinical Pharmacology of Antibody-Drug Conjugates. Antibodies (Basel). 2021 May 21;10(2):20.


Recommended Reading
-
Chinese Pharmaceutical Industry “Divine Song”!~~ Following the “Song of PD-1”, Drug Times plans to launch “Song of Dual Antibodies” | Attached: 30+ articles on the theme of dual antibodies -
Industry again sees [Gold Diggers]: I will bet one last time! -
Three Academicians Gather! Creating a Source Innovation Mechanism for Biopharmaceuticals Guided by Clinical Value | The Shanghai Source Innovative Drug Summit Forum Successfully Concluded! -
Alzheimer’s Disease, possibly the conclusion of our aging… -
RSV Field Stirs After 60 Years! AstraZeneca/Sanofi, One Shot Ahead! -
Ruo Yongqing leaves Tengsheng Bo Pharmaceutical to join Cloud Top New Drug, the Chinese pharmaceutical industry’s talent war enters a fever pitch. Is this a sign of industry maturity? Please vote! -
From 2.8 million to 3 million, the record for the world’s most expensive drug was broken! It only took 30 days! -
Heavyweight! CDE releases draft for public consultation on ADC clinical development technical guidelines (Attached: ~100 ADC articles) -
With a vast sea of medicine, innovation walks the great road! The 2022 Third China New Drug CMC Summit Forum invites you again to Shanghai! (Second round notice) -
The Biden administration wants to crack down on Chinese CXO? It seems like a typhoon has passed, but only branches and leaves are moving.
