Skip to content
Antibody-drug conjugates (ADC) are formed by the coupling of specific targeting monoclonal antibodies and highly active cytotoxic drugs through linkers. With their unique pharmaceutical properties, ADC drugs exhibit strong anti-tumor activity in the field of cancer therapy, while also offering higher safety compared to traditional chemotherapy.
In recent years, the development of ADC drugs in the field of cancer treatment has been rapid, particularly in the treatment of HER2-positive breast cancer, where ADC drugs have significantly benefited patients, providing strong new treatment options. Despite the excellent clinical performance of ADCs, they still face resistance issues. Reviews have reported that the resistance of ADC drugs is related to antigen expression, ADC processing, and effective payloads. The relevant research content is summarized below for the readers.
ADC Resistance Mechanisms
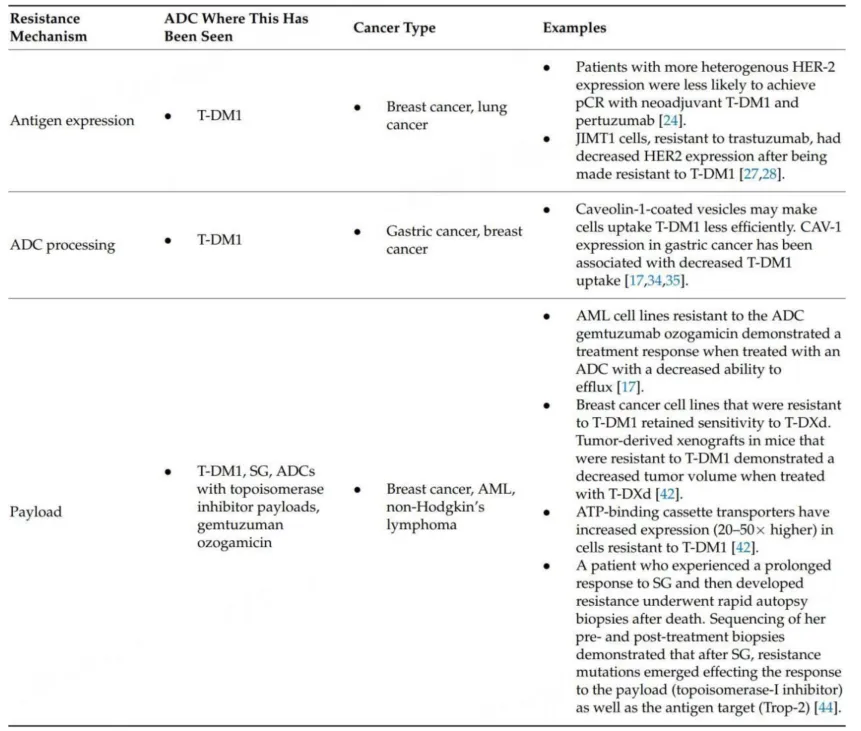
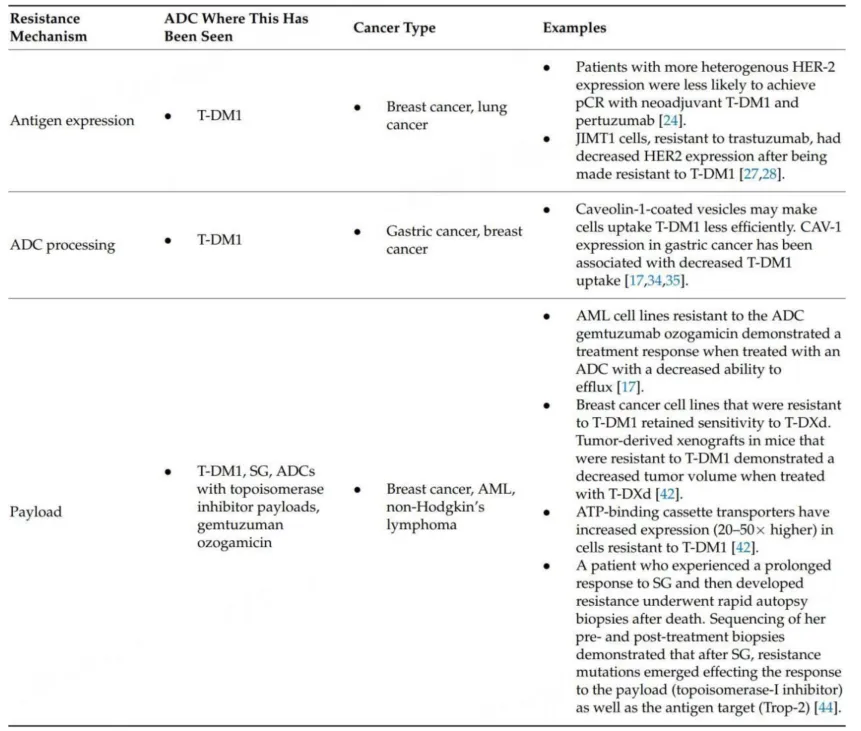
Based on the complex structure of ADCs, potential resistance mechanisms are classified, and the table below summarizes the proposed preclinical and clinical resistance mechanisms, categorized by changes in antigen expression, ADC processing, and effective payload changes. This classification method provides direction for future research and helps further understand these mechanisms and new drug development targets, thereby expanding the efficacy of ADCs.
Table 1. Classification of Resistance Mechanisms
In early trials of T-DM1, it was observed that tumors with higher and more uniform HER2 expression levels were more likely to respond to treatment. Considering that HER2 expression may have heterogeneity, tumor heterogeneity was reported in 16%-36% of cases. For therapeutic drugs requiring homogeneous HER2 expression, any change in HER2 levels may lead to resistance. Further evidence supporting this hypothesis includes the observation that HER2-positive tumors exhibited lower HER2 expression after treatment, and more heterogeneous expression was associated with higher recurrence rates and lower survival rates.
A study of early HER2-positive breast cancer patients receiving neoadjuvant treatment with T-DM1 and pertuzumab found that pre-treatment HER2 heterogeneity (defined as 5-50% of tumor cells with ERBB-2 amplification or HER2-FISH negative areas) could inversely predict treatment response. In fact, among patients with heterogeneity in pre-treatment biopsies, 0% achieved pathological complete response, while 55% of non-heterogeneous patients achieved pCR when treated with the combination of T-DM1 and pertuzumab. Additionally, T-DM1 resistant patients’ circulating tumor DNA (ctDNA) displayed fewer tumor cells with HER2 amplification.
Further evidence supporting the hypothesis that decreased antigen expression mediates ADC resistance comes from preclinical cell lines. Using trastuzumab-resistant JIMT1 cells to construct xenograft tumors responsive to high concentrations of T-DM1, subsequent testing showed a decrease in HER2 expression after periodic T-DM1 treatment. In a gastric cancer cell model, a preclinical example demonstrated the importance of the bystander effect in overcoming decreased antigen expression. These cells developed resistance to T-DM1 and subsequently exhibited resistance to ADCs with non-cleavable linkers while retaining sensitivity to ADCs with cleavable linkers and cell-permeable effective payloads. Similar studies in the JIMT1 cell line identified that restoring HER2 expression could reverse resistance to T-DM1.
In addition to abnormal antigen expression levels, dimerization of the antigen with another cell surface receptor may mediate resistance to ADCs. NRG-1β is a ligand known to induce HER2/HER3 heterodimerization, which can inhibit the cytotoxic activity of T-DM1 in subpopulations of HER2-amplified breast cancer cell lines. This resistance can be overcome by the addition of pertuzumab, an anti-HER2 monoclonal antibody that blocks HER2/HER3 dimerization and downstream signaling. In vitro and in vivo tumor xenograft models showed that the combination of T-DM1 and pertuzumab exhibited a synergistic effect. Another strategy involves the use of bispecific antibodies in ADCs, which recognize different epitopes of the target antigen. This indicates that preclinical studies of REGN5093-M114 (a bispecific MET-targeting ADC being studied in MET-overexpressing EGFR-mutant NSCLC cell lines) have been successful.The structural differences between T-DXd and T-DM1 are significant; T-DXd includes membrane-permeable effective payloads and cleavable linkers. Based on this characteristic, T-DXd exhibits a bystander effect, where the released effective payload can penetrate adjacent tumor cells to exert anti-tumor effects, which is also one of the important mechanisms by which T-DXd overcomes T-DM1 resistance.
Given the impact of antigen heterogeneity on mediating ADC resistance, future strategies to address this resistance may include drugs with dual antibodies (bispecific ADCs). Additionally, combination therapies that enhance antigen expression may be valuable. In a study of ERBB2 amplification or mutation in lung cancer, it was observed that when T-DM1 was combined with the irreversible pan-HER kinase inhibitor neratinib, lung cancer cells showed increased uptake of T-DM1, while a decrease in T-DM1 uptake was observed when using the reversible HER2 inhibitor lapatinib.
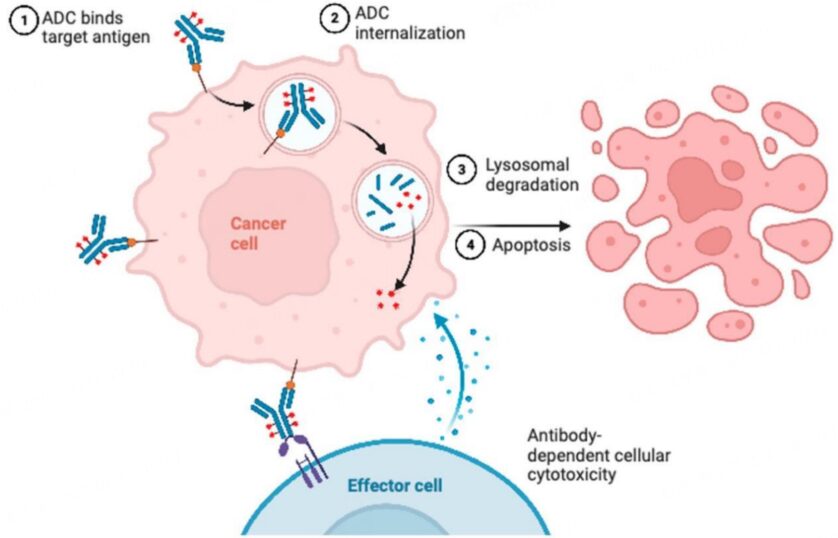
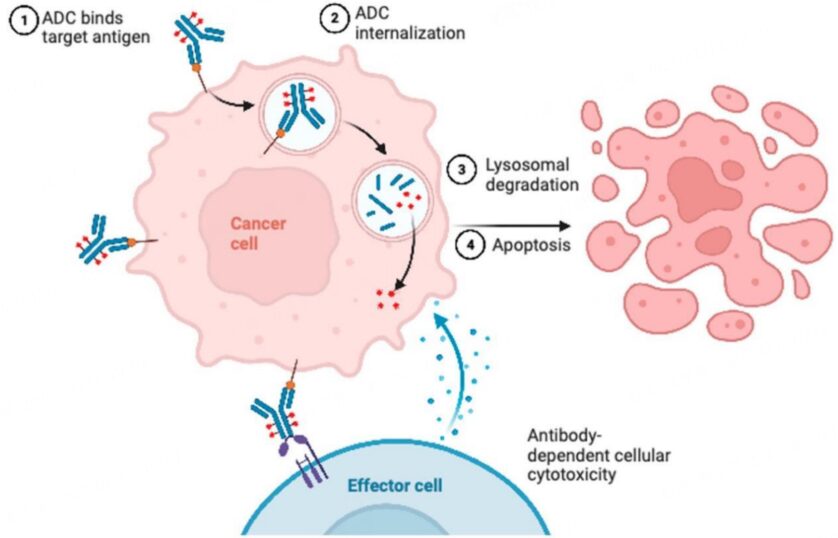
The complexity of ADCs, especially compared to small molecules, provides many possible opportunities for resistance (Figure 1). In many cases, particularly in ADCs with non-cleavable linkers, before ADCs release their effective payloads, they typically bind to target antigens, then internalize into tumor cells, and undergo processing within the cells. In preclinical studies, some reasons for resistance, especially intracellular mechanisms, are difficult to prove as driving factors of resistance, but inferences have been drawn based on observations from treatment resistance models. Proposed hypotheses for mediating ADC resistance involve changes in intracellular uptake and processing. One proposed mechanism involves reduced permeability to cells through barriers before ADCs enter the cells, including increased cellular basement membranes. Another proposed mechanism comes from recent preclinical work demonstrating that abnormal endosomal transport may be involved in T-DM1 resistance.
One mechanism ensuring specificity of ADCs is mediated by clathrin-mediated endocytosis in cells expressing target antigens. In the T-DM1 resistant N89-TM cell line, an alternative uptake mechanism was discovered, where cells utilized caveolin-1 (CAV1)-coated vesicles, which may be less efficient. Consistent with this observation, a recent study in gastric cancer found that tumor CAV1 levels were negatively correlated with T-DM1 tumor uptake. In multiple xenograft models, genetic or pharmacological inhibition of CAV1 increased T-DM1 uptake and acted synergistically with T-DM1. Furthermore, glycosaminoglycan modifications negatively regulate the internalization of tumor antigen CAIX and anti-CAIX ADCs by promoting the binding of CAIX with CAV1 in membrane lipid rafts. Pharmacological inhibition of protein glycosaminoglycan modifications can increase the internalization and cytotoxic activity of anti-CAIX ADCs. In another distinct study, due to changes in pH, it was observed that T-DM1 resistant cells lacked proteolytic activity after ADC reached lysosomes, leading to drug accumulation simulating lysosomal storage disease.
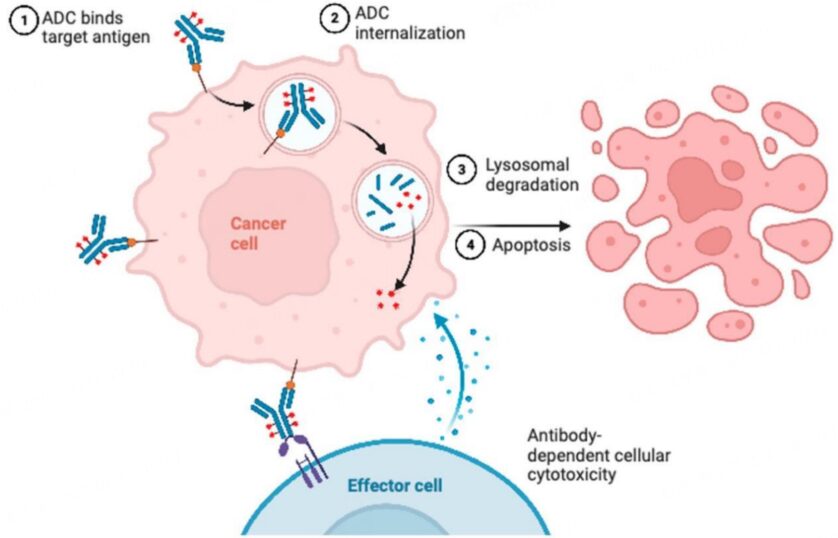 Figure 1. Possible Resistance Mechanisms of ADCs
In the JIMT1-TM cell line resistant to T-DM1, proteins including Rab5B, ATG9a, and HTT were found to be increased, mediating lysosomal processing and vesicle transport. Proteomic analysis showed particularly high protein levels of Rab6 (a protein involved in microtubule-mediated transport) and cytoskeletal tension-related protein PAK4. To extend these findings, live-cell imaging microscopy was used to observe JIMT1-TM cells and the 361-TM cell line. For the 361-TM cell line, compared to the parental cells that were not resistant to T-DM1, ADCs with non-cleavable linkers spent significantly longer in lysosomes, raising concerns about the lower efficiency of ADC processing. Interestingly, this result was not observed in ADCs with cleavable linkers, indicating mechanisms to overcome resistance. In the JIMT1-TM cell line, both ADCs with cleavable and non-cleavable linkers exhibited longer co-localization in lysosomes than parental cells. Unsurprisingly, compared to parental cells, both resistant cell lines showed reduced levels of linker-effective payload metabolites, but it remains uncertain whether this is driven by decreased HER2 expression, reduced ADC processing, or both. Consistent with the view that effective payload release may involve different ADCs depending on linker status, a recent study utilizing CRISPR screening demonstrated that ADCs with cleavable linkers were rapidly processed immediately after ADC uptake and transported to early endosomes, while ADCs with non-cleavable linkers required further lysosomal delivery to successfully release their payloads. Additionally, literature has reported that the depletion of sialic acid promotes the lysosomal delivery of ADCs (potentially by reducing ADC recycling), making cells sensitive to ADC toxicity.
Some observed resistance mechanisms involve the payload itself, which can be overcome by using ADCs with alternative payloads. For example, ADC resistance to topoisomerase inhibitors can be driven by changes in topoisomerase expression or downstream signaling mechanisms. This has also been observed in tumor models of non-Hodgkin lymphoma, where replacing ADCs containing auristatin payloads with those based on anthracyclines helped patients further respond to ADC treatment. Similarly, in breast cancer cells resistant to T-DM1, tumor cells remain sensitive to T-DXd. To track these results, mouse tumor xenograft models were established using cells sensitive and resistant to T-DM1. The xenograft model constructed from T-DM1 resistant cells was insensitive to T-DM1, but when treated with T-DXd, these mice showed reduced tumor volume. The application of this theory includes the development of other HER2-targeted or TROP-2-targeted ADCs, which may provide alternative payloads to overcome payload-related resistance.
Figure 1. Possible Resistance Mechanisms of ADCs
In the JIMT1-TM cell line resistant to T-DM1, proteins including Rab5B, ATG9a, and HTT were found to be increased, mediating lysosomal processing and vesicle transport. Proteomic analysis showed particularly high protein levels of Rab6 (a protein involved in microtubule-mediated transport) and cytoskeletal tension-related protein PAK4. To extend these findings, live-cell imaging microscopy was used to observe JIMT1-TM cells and the 361-TM cell line. For the 361-TM cell line, compared to the parental cells that were not resistant to T-DM1, ADCs with non-cleavable linkers spent significantly longer in lysosomes, raising concerns about the lower efficiency of ADC processing. Interestingly, this result was not observed in ADCs with cleavable linkers, indicating mechanisms to overcome resistance. In the JIMT1-TM cell line, both ADCs with cleavable and non-cleavable linkers exhibited longer co-localization in lysosomes than parental cells. Unsurprisingly, compared to parental cells, both resistant cell lines showed reduced levels of linker-effective payload metabolites, but it remains uncertain whether this is driven by decreased HER2 expression, reduced ADC processing, or both. Consistent with the view that effective payload release may involve different ADCs depending on linker status, a recent study utilizing CRISPR screening demonstrated that ADCs with cleavable linkers were rapidly processed immediately after ADC uptake and transported to early endosomes, while ADCs with non-cleavable linkers required further lysosomal delivery to successfully release their payloads. Additionally, literature has reported that the depletion of sialic acid promotes the lysosomal delivery of ADCs (potentially by reducing ADC recycling), making cells sensitive to ADC toxicity.
Some observed resistance mechanisms involve the payload itself, which can be overcome by using ADCs with alternative payloads. For example, ADC resistance to topoisomerase inhibitors can be driven by changes in topoisomerase expression or downstream signaling mechanisms. This has also been observed in tumor models of non-Hodgkin lymphoma, where replacing ADCs containing auristatin payloads with those based on anthracyclines helped patients further respond to ADC treatment. Similarly, in breast cancer cells resistant to T-DM1, tumor cells remain sensitive to T-DXd. To track these results, mouse tumor xenograft models were established using cells sensitive and resistant to T-DM1. The xenograft model constructed from T-DM1 resistant cells was insensitive to T-DM1, but when treated with T-DXd, these mice showed reduced tumor volume. The application of this theory includes the development of other HER2-targeted or TROP-2-targeted ADCs, which may provide alternative payloads to overcome payload-related resistance.
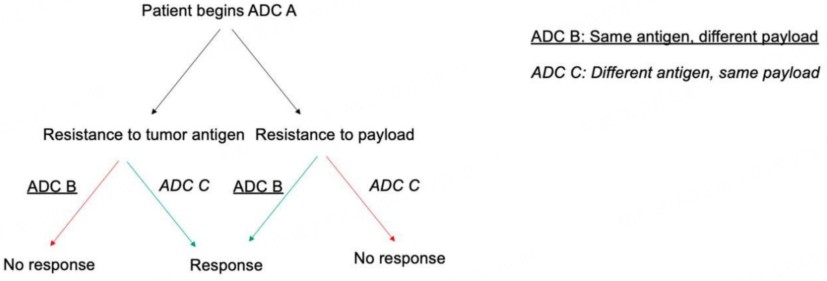
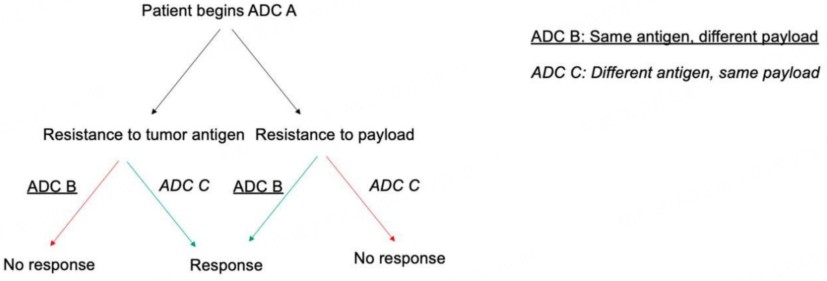
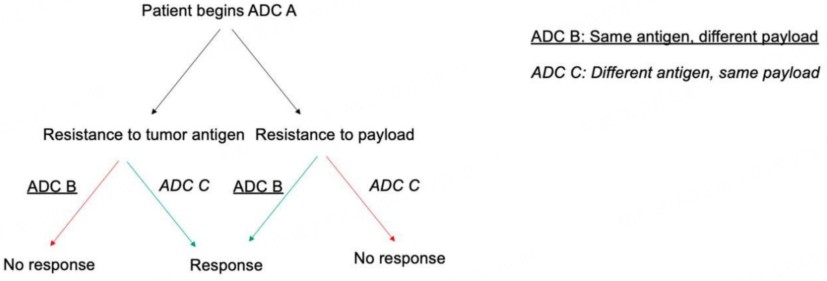 Figure 2. Resistance Mechanisms of ADCs
The ability to perform whole exome sequencing during ADC treatment allows for real-time tracking of resistance mutations’ development and provides theoretical support for future treatments. For instance, a study evaluated the resistance mechanism of a patient who had a prolonged response (over 8 months) to SG, who underwent whole exome sequencing before starting treatment. After progression, rapid autopsy specimens were taken, and pre- and post-treatment specimens were compared with SG. Analysis of mutations occurring after treatment indicated that tumor subclones carried TOP1 mutations (encoding topoisomerase-1, the target of SG effective payload), as well as unique subclones carrying TACSTD2 mutations (encoding TROP-2, the antigen target of SG). These findings suggest the existence of parallel resistance mechanisms against ADC antibodies and effective payloads, indicating that tumor cells may develop resistance to sequential ADCs, including those with similar effective payloads or similar antibody targets. Future innovations in targeting and rapid sequencing may provide personalized treatment guidance based on resistance mutations generated from previous treatments.
Increased efflux of ADC effective payloads mediated by ATP-binding cassette transporters is another potential resistance mechanism. Compared to parental cells, increased expression of transport proteins was observed in T-DM1 resistant cells, up to 20-50 times. This mechanism was observed in AML cell models as a means of resistance to gemtuzumab ozogamicin (GO). Similarly, patients with lower levels of ATP-binding cassette ABCB1 exhibited improved responses to GO. In different cell lines, after developing resistance to T-DM1, increased expression of the gene ABCC1 was noted. Finally, in preclinical models of paclitaxel-resistant cancer cell lines, resistance to ADCs with paclitaxel-derived payloads was associated with ABCB1 overexpression-mediated TUBB3 activation.
Multiple potential preclinical and clinical mechanisms have been proposed to explain these resistance means. Studies have found that cell lines resistant to T-DM1 also exhibit resistance to trastuzumab-directed ADCs with non-cleavable linkers. When the drug efflux pump ABCC1 is reversed or knocked down with siRNA, tumor cells exhibit new sensitivity to ADCs with non-cleavable linkers. Interestingly, in AML cells resistant to GO, a new remission occurred when using the less efflux-potential cytotoxic drug vadastuximab talirine instead. After 9 months of ADC treatment, RNAseq analysis was performed in a preclinical breast cancer mouse model treated with an anti-nectin-4 targeted ADC (named N41mab-vc-MMAE). Additionally, in this model, ABCB1 was upregulated. When ADCs were co-administered with the P-glycoprotein pharmacological inhibitor tariquidar, rapid therapeutic responses were observed, with tolerability significantly better than that of tariquidar combined with docetaxel.
Although the advent of ADCs has provided new treatment options for cancer patients, most tumors eventually develop resistance to these drugs. Recent preclinical models and clinical analyses have attempted to simulate these resistance mechanisms, aiming to develop novel therapeutic strategies that can overcome and improve these resistances. Given the complexity of ADCs, potential resistance mechanisms may involve decreased antigen expression, reduced ADC transport and processing, resistance to cytotoxic effective payloads, and increased drug efflux. Future efforts to overcome initial resistance to ADCs should be based on the mechanisms described. Ongoing research optimizing sequential and combination treatments of ADCs is expected to provide more clues for the best use of these drugs. In summary, relevant explorations illustrate the prospects of translational research in suggesting new treatment options and possibly improving clinical outcomes for patients.
[1] Abelman RO, Wu B, Spring LM, et al. Mechanisms of Resistance to Antibody-Drug Conjugates. Cancers (Basel). 2023 Feb 17;15(4):1278.
[2] Yamazaki CM, Yamaguchi A, Anami Y, et al. Antibody-drug conjugates with dual payloads for combating breast tumor heterogeneity and drug resistance. Nat Commun. 2021 Jun
Scan the WeChat QR code to add the Antibody Circle editor,qualified individuals can join the Antibody Circle WeChat group!
Please indicate: Name + Research Direction!
This public account’s reposted articles are for the purpose of conveying more information, and the source and author are clearly indicated. If any media or individual does not wish to be reposted, please contact us ([email protected]), and we will immediately delete it. All articles represent the author’s views and do not represent the position of this site.
Figure 2. Resistance Mechanisms of ADCs
The ability to perform whole exome sequencing during ADC treatment allows for real-time tracking of resistance mutations’ development and provides theoretical support for future treatments. For instance, a study evaluated the resistance mechanism of a patient who had a prolonged response (over 8 months) to SG, who underwent whole exome sequencing before starting treatment. After progression, rapid autopsy specimens were taken, and pre- and post-treatment specimens were compared with SG. Analysis of mutations occurring after treatment indicated that tumor subclones carried TOP1 mutations (encoding topoisomerase-1, the target of SG effective payload), as well as unique subclones carrying TACSTD2 mutations (encoding TROP-2, the antigen target of SG). These findings suggest the existence of parallel resistance mechanisms against ADC antibodies and effective payloads, indicating that tumor cells may develop resistance to sequential ADCs, including those with similar effective payloads or similar antibody targets. Future innovations in targeting and rapid sequencing may provide personalized treatment guidance based on resistance mutations generated from previous treatments.
Increased efflux of ADC effective payloads mediated by ATP-binding cassette transporters is another potential resistance mechanism. Compared to parental cells, increased expression of transport proteins was observed in T-DM1 resistant cells, up to 20-50 times. This mechanism was observed in AML cell models as a means of resistance to gemtuzumab ozogamicin (GO). Similarly, patients with lower levels of ATP-binding cassette ABCB1 exhibited improved responses to GO. In different cell lines, after developing resistance to T-DM1, increased expression of the gene ABCC1 was noted. Finally, in preclinical models of paclitaxel-resistant cancer cell lines, resistance to ADCs with paclitaxel-derived payloads was associated with ABCB1 overexpression-mediated TUBB3 activation.
Multiple potential preclinical and clinical mechanisms have been proposed to explain these resistance means. Studies have found that cell lines resistant to T-DM1 also exhibit resistance to trastuzumab-directed ADCs with non-cleavable linkers. When the drug efflux pump ABCC1 is reversed or knocked down with siRNA, tumor cells exhibit new sensitivity to ADCs with non-cleavable linkers. Interestingly, in AML cells resistant to GO, a new remission occurred when using the less efflux-potential cytotoxic drug vadastuximab talirine instead. After 9 months of ADC treatment, RNAseq analysis was performed in a preclinical breast cancer mouse model treated with an anti-nectin-4 targeted ADC (named N41mab-vc-MMAE). Additionally, in this model, ABCB1 was upregulated. When ADCs were co-administered with the P-glycoprotein pharmacological inhibitor tariquidar, rapid therapeutic responses were observed, with tolerability significantly better than that of tariquidar combined with docetaxel.
Although the advent of ADCs has provided new treatment options for cancer patients, most tumors eventually develop resistance to these drugs. Recent preclinical models and clinical analyses have attempted to simulate these resistance mechanisms, aiming to develop novel therapeutic strategies that can overcome and improve these resistances. Given the complexity of ADCs, potential resistance mechanisms may involve decreased antigen expression, reduced ADC transport and processing, resistance to cytotoxic effective payloads, and increased drug efflux. Future efforts to overcome initial resistance to ADCs should be based on the mechanisms described. Ongoing research optimizing sequential and combination treatments of ADCs is expected to provide more clues for the best use of these drugs. In summary, relevant explorations illustrate the prospects of translational research in suggesting new treatment options and possibly improving clinical outcomes for patients.
[1] Abelman RO, Wu B, Spring LM, et al. Mechanisms of Resistance to Antibody-Drug Conjugates. Cancers (Basel). 2023 Feb 17;15(4):1278.
[2] Yamazaki CM, Yamaguchi A, Anami Y, et al. Antibody-drug conjugates with dual payloads for combating breast tumor heterogeneity and drug resistance. Nat Commun. 2021 Jun
Scan the WeChat QR code to add the Antibody Circle editor,qualified individuals can join the Antibody Circle WeChat group!
Please indicate: Name + Research Direction!
This public account’s reposted articles are for the purpose of conveying more information, and the source and author are clearly indicated. If any media or individual does not wish to be reposted, please contact us ([email protected]), and we will immediately delete it. All articles represent the author’s views and do not represent the position of this site.