
Source: Xiaoyao Shuo Yao
Antibody-drug conjugates (ADC) are a powerful cancer treatment method that combines monoclonal antibodies targeting specific antigens with small molecule cytotoxic drugs linked by a linker. ADCs utilize the specificity of antibodies for their target antigens, combined with the potency of cytotoxic drugs, to selectively kill tumor cells expressing the target antigens. They possess the strong killing effect of traditional small molecule chemotherapy while maintaining the tumor-targeting capability of antibody drugs.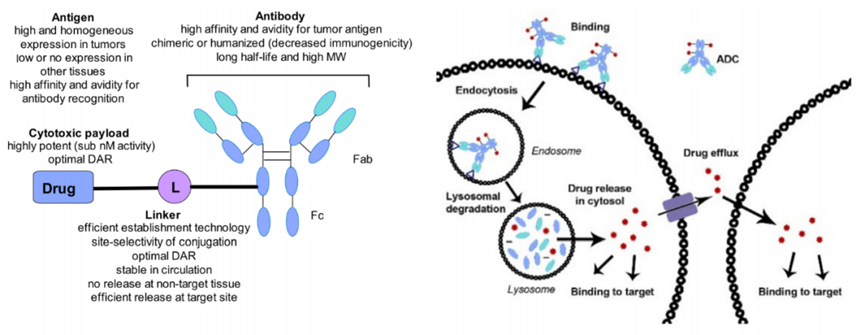
In the development of ADCs, selecting target antigens that are highly expressed on malignant cells but lowly expressed on normal tissues and immune cells is considered key to achieving selectivity and efficacy while minimizing off-target toxicity. Additionally, the selection of antigens for ADCs must consider several factors related to the expression patterns and biological characteristics of the target antigens.
The use of highly effective cytotoxic payloads in ADCs requires rational target antigen selection, aimed at maximizing tumor selectivity and anti-tumor efficacy while minimizing off-target dose-limiting toxicity. Therefore, delivering the payload as much as possible to cancer cells while balancing factors such as safety and efficacy is crucial for ADC design.
According to currently accepted principles, an ideal target antigen for effective ADCs should be expressed on the surface of tumor cells at sufficient density and uniformity while being minimally expressed on normal cells to limit off-target toxicity and optimize the therapeutic index. In addition to specificity and overexpression, the best target antigens also need to be extracellular to allow antibody binding to the antigen epitope. Furthermore, the efficacy of ADCs often depends on effective target-mediated internalization, and the internalization rate and lysosomal transport kinetics after the tumor antigen binds to the ADC may directly affect payload release and cancer cell killing.
It is also crucial to understand that the antigen target primarily directs the recycling or lysosomal targeting pathways. The recycling of the antigen-ADC complex back to the plasma membrane is believed to affect the effective delivery of the ADC to lysosomes and may hinder the release of the payload into the cytoplasm, thereby impairing the efficacy of the ADC. Finally, another factor affecting the efficacy of ADCs is the rate at which antigens are removed from the cell surface, typically mediated by proteases produced by tumor cells, a process known as antigen shedding.
Target Expression Levels
The antigen expression threshold level required for ADC activity varies significantly based on several parameters, many of which remain unexplained. The expression level is known to depend on the specific target, recognized antigen epitopes, and cancer indications, which is particularly evident for ADCs targeting solid tumors. For instance, clinical experience assessing the efficacy of Kadcyla in HER2-positive metastatic breast cancer indicates that the survival rate is better in the high-expression subgroup compared to the HER2 low-expression subgroup.
However, the prominent efficacy of Enhertu in patients with HER2-low breast cancer suggests that there is no broadly applicable target antigen expression threshold to ensure ADC efficacy. In vitro and in vivo experiments have shown that some HER2-negative cell lines may still maintain active HER2 signaling and be sensitive to anti-HER2 therapies. This indicates that lower levels of pro-tumor signaling resulting from low surface expression of HER2 may still support tumor growth. Other targets also vary; for example, selecting patients with only high expression of the FRα target antigen appears to be associated with therapeutic benefits. In clinical studies of renal cell carcinoma, the ADC target CD70 showed only limited correlation between antigen expression levels and sensitivity to CD70-targeted ADCs.
Overall, preclinical studies and clinical evaluations targeting several cancer types with ADCs suggest that there is no universal paradigm linking antigen expression levels to ADC activity. Therefore, it is necessary to empirically determine the ideal cut-off value for antigen expression for each tumor type and ADC.
Off-Target Toxicity
The most common toxicity observed clinically with ADC treatment is due to off-target effects, and the off-target tumor toxicity of ADCs may be influenced by target antigen selection.
To mitigate toxicity, the physiological role of the target antigen and the mechanisms through which it exerts this role must also be considered. Therefore, preclinical toxicity studies of new ADC targets must not only investigate the differential expression of the target between tumors and normal tissues but also the physiological functions of the target to identify potential toxicities. For example, the CD44 antibody bivatuzumab conjugated with DM-1 used in a Phase I trial for squamous cell carcinoma reported fatal skin toxicity, possibly attributed to the expression of CD44 in healthy keratinocytes.
However, while the expression of target antigens in normal cells is an important consideration, it does not necessarily preclude the development and eventual success of ADCs. For instance, although TROP-2 is expressed at high levels in some normal tissues, Trodelvy has been successfully developed and received FDA approval for the treatment of metastatic triple-negative breast cancer. This suggests that for anti-TROP-2 ADCs, the difference in antigen expression in normal tissues compared to malignant tissues may be sufficient to avoid severe toxicity. Additionally, it is believed that the intracellular rather than surface expression of TROP-2 in normal cells, or its expression in areas such as ducts or glandular epithelial lumens where antibodies or ADCs cannot access, may play an important role.
Antigen Shedding
When selecting ADC targets, the rate of antigen shedding may be an important consideration. In antibody-based therapies, antigen shedding refers to the removal of surface-expressed target antigens, a process typically mediated by proteases as a means of functional regulation. Early studies on immunotoxins indicated that increased antigen shedding could reduce the amount of ADCs available for targeting and binding to tumors, thereby impairing ADC efficacy. However, other studies using mathematical and experimental models suggest that the effect of high antigen shedding rates on ADC efficacy may depend on several factors, including ADC internalization rates, ADC recycling rates, and the rate of extravasation through the tumor microenvironment. For instance, the same models for anti-mesothelin and anti-CD25 immunotoxins indicate that increased shedding rates enhance the efficacy of the former but reduce the efficacy of the latter.
For hematologic tumors, lineage-specific biomarkers such as CD19, CD20, CD22, CD33, BCMA, and CD79 are widely and uniformly expressed at high levels on malignant blood cells and have been extensively explored as candidate targets for ADC development. Additionally, the target antigens of approved ADCs are easily internalized after binding, which is also an important feature that contributes to ADC efficacy.
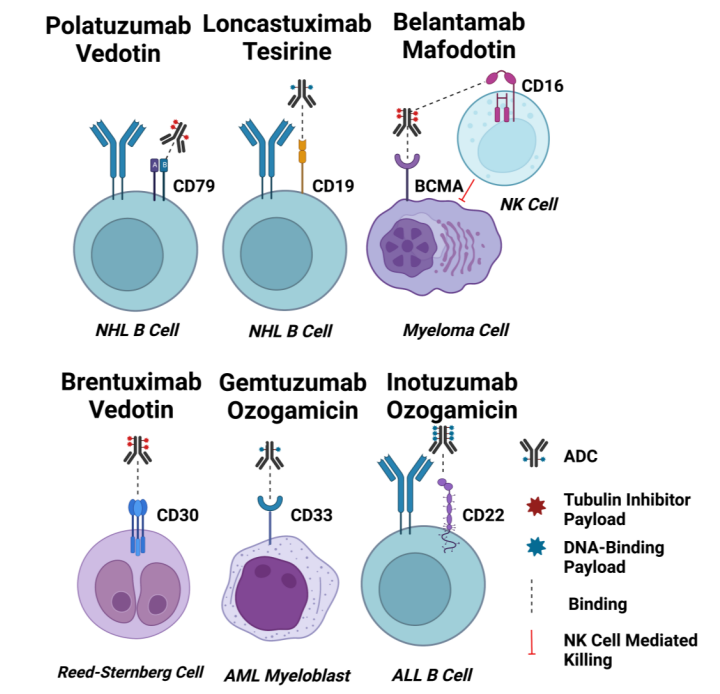
CD33
CD33 is a 67 kDa transmembrane glycoprotein receptor and a member of the sialic acid-binding immunoglobulin-like lectin (SIGLEC) family, typically expressed on normal myeloid cells. Due to its preferential overexpression on AML cells, it is the target of Gemtuzumab ozogamicin. The intracellular immune receptor tyrosine-based inhibition motif (ITIM) of CD33 regulates its internalization, which can be activated through clathrin-mediated endocytosis (CME). There is no correlation between the expression level of CD33 and its internalization rate in AML cells. CD33 is a slowly internalizing antigen, and cross-linking CD33 does not enhance its internalization. Lack of response to GO in AML patients may be related to dysfunctional internalization of the CD33 receptor.
CD22
CD22 is a 140 kDa transmembrane glycoprotein and, like CD33, is a member of the SIGLEC family, sharing several structural features with it. The key difference is that CD22 is much larger than CD33, as it has multiple Ig domains and ITIM/ITIM-like motifs. CD22 expression is limited to B cells, and its expression level is elevated in most progenitor cells of various B-cell malignancies (including ALL).
CD22 undergoes internalization via CME. Ligand-like natural ligands accumulate intracellularly through structural rapid internalization via CD22. These ligands are categorized and degraded in lysosomes, while CD22 recycles back to the cell surface. Moreover, ligands induced internalization of CD22 activates intracellular pools, replenishing or increasing the expression levels of CD22 on the cell surface. Therefore, CD22 possesses good internalization characteristics for ADCs.
CD19
CD19 is considered a pan-B-cell marker and is a major signaling component of the surface multimeric complex in mature B cells. CD19 expression is highly conserved in most B-cell malignancies, and it also has rapid internalization kinetics without shedding into circulation, making it an ideal ADC target antigen.
CD79b
CD79b is expressed only in immature and mature B cells and is overexpressed in ≥80% of malignant B cells. CD79a and CD79b are two non-covalently associated transmembrane proteins that mediate signaling and internalization. For the latter, the CD79a-CD79b heterodimer serves as a scaffold controlling BCR internalization. BCR internalization is mainly accomplished through CME and mediated by AP-2. Interestingly, CD79a directly interacts with the μ subunit of AP-2, thereby activating CD79b and leading to the internalization of the entire BCR complex.
Additionally, CD79a can internalize as a monomer, but CD79b cannot. If the proximal membrane tyrosine (Y195) of CD79b is mutated, the binding of AP-2 to CD79a is blocked, and internalization is also inhibited. Mutations in Y195 have been observed in 18% of activated B-cell-like DLBCL specimens. Overall, evidence suggests that the internalization activity of CD79b depends on the internalization of the entire BCR complex rather than its internalization as a monomer.
BCMA
BCMA or CD269, also known as TNFR superfamily member 17, transmits signals that induce B cell survival and proliferation. BCMA has a molecular weight of only 20.2 kDa, and its ligand-binding extracellular region has a “cabbage” conformation composed of six CRDs. In addition to multiple myeloma, BCMA is also expressed in many hematologic malignancies, such as Hodgkin lymphoma and non-Hodgkin lymphoma.
However, little is known about the precise internalization pathway utilized by BCMA. Regarding internalization, sialylation is a regulatory function that may induce BCMA to utilize CME for internalization.
CD30
CD30 is a 120 kDa transmembrane glycoprotein that belongs to the tumor necrosis factor receptor (TNFR) superfamily. Its extracellular portion consists of six extended conformations of cysteine-rich domains (CRDs). CD30 is expressed on activated T cells and B cells, as well as various lymphoid tumors (including Hodgkin lymphoma and ALCL).
CD30 does not possess internalization; instead, it sheds due to proteolytic cleavage, which is mediated by matrix metalloproteinases (MMPs). Shedding is a characteristic of CD30 biology, and high concentrations of circulating soluble CD30 can serve as a serum marker for monitoring tumor progression. For ADC efficacy, elevated circulating levels of CD30 appear to sequester injected ADCs, thereby reducing the number of ADCs that can localize to CD30-positive tumor sites. Thus, the lack of internalization suggests that CD30 is not an ideal ADC target.
ADCs designed for the treatment of solid tumors target a range of antigens, often including tumor-associated membrane proteins or receptors that may be associated with pro-tumor pathways. To date, the FDA has approved ADCs for the treatment of solid tumors targeting HER2, TROP2, Nectin-4, FRα, and TF.
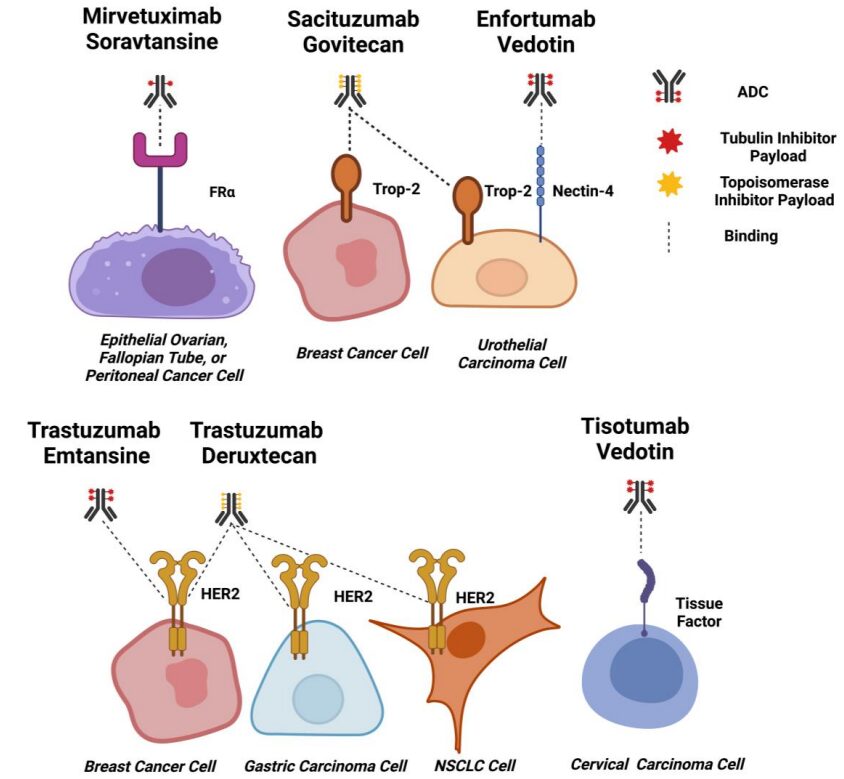
HER2
HER2 is a 185 kDa transmembrane glycoprotein that belongs to the EGFR family. Amplification of the HER2/neu gene is a known driver of human malignancies and metastasis. Due to the role of HER2 in cancer, it has been targeted for therapy for decades. HER2 has also been a target for ADCs, with T-DM1 and T-DXT both approved for HER2-positive metastatic breast cancer patients.
HER2 internalization occurs through multiple mechanisms, primarily CME, with co-immunoprecipitation clearly showing that HER2 directly interacts with AP-2; additionally, dynasore can completely block HER2 internalization in SKBR3 cells. Moreover, studies have demonstrated that HER2 can utilize caveolae-mediated endocytosis and CLIC/GEEC pathways for internalization.
TROP-2
Trop2 is a 46 kDa monomeric glycoprotein with selective overexpression, structural internalization, and lysosomal targeting properties, making it a highly attractive target for ADCs. The internalization mechanism of Trop2 is related to CME.
Furthermore, Trop2 binds to various ligands, such as claudin-1, claudin-7, cyclin D1, and IGF1; however, none of these ligands have been shown to be internalized upon binding or interaction with Trop2. Therefore, the internalization of Trop2 is more pronounced in tumor cells compared to normal cells, indicating that Trop2 is a good target for ADCs.
Nectin-4
Nectin-4 is a 66 kDa type I transmembrane protein primarily involved in promoting cell-cell contact. Nectin-4 is an attractive ADC target because studies have shown that it is overexpressed in several tumor types but is nearly absent in normal adult tissues.
Currently, there is no information on the internalization of natural ligands or mAb/ADC complexes with nectin-4; however, studies on the internalization of nectin-4 by pathogenic binding can provide insight. Nectin-4 is also a receptor for the measles virus, and studies have shown that the measles virus enters MCF7, HTB-20 breast cancer, and DLD-1 colorectal cancer cells via macropinocytosis. Viral entry requires PAK1, while the dynamin inhibitor Dynasore does not affect viral entry. Additionally, cells expressing dominant-negative caveolin proteins do not eliminate viral internalization. Based on these indirect studies, nectin-4 exhibits strong internalization activity required for viral receptors.
TF
TF (Tissue Factor), also known as coagulation factor III or CD142, is a transmembrane glycoprotein with pro-coagulant activity that has the ability to induce intracellular signaling through the proteolytic enzyme factor VIIa (FVIIa). TF is believed to promote cancer progression through FVIIa-dependent intracellular signaling pathways that regulate cell survival, proliferation, metastasis, and angiogenesis. It is upregulated in various solid tumors and tumor vascular systems due to hypoxia-induced signaling.
This antigen’s internalization properties make it an ideal choice for developing TF-targeted ADCs. Additionally, reported mechanisms of surface TF expression induced by TF-FVIIa complexes, where the formation of TF-FVIIa complexes leads to TF release from the Golgi apparatus, followed by transport to the membrane, results in enhanced surface TF expression. If this effect can be induced by anti-TF ADCs, it could allow repeated targeting of malignant cells expressing TF.
FRα
FRα (Folate Receptor α) is a membrane-bound folate receptor involved in the intracellular transport of folate. Once bound to folate, the receptor-ligand complex is internalized through a non-classical lipid raft endocytosis mechanism. FRα is highly expressed in ovarian cancer, breast cancer, endometrial cancer, mesothelioma, and lung cancer, while being nearly absent in normal cells, making this receptor highly suitable for ADC targeting.
Moreover, FRα is believed to assist pro-tumor signaling through folate binding, inducing downstream effects such as activation of STAT3, intracellular transport of FRα as a transcription factor for growth pathways, and intracellular transport of folate for DNA biosynthesis.
When selecting target antigens for ADCs targeting solid tumors and hematologic malignancies, several factors may need to be considered: including (1) the degree of antigen expression in tumors and healthy tissues; (2) the physiological functions of the antigen in normal and tumor cells; (3) the internalization characteristics and mechanisms of the antigen; (4) whether, where, and how the antigen sheds, and the potential impact of shedding on ADC efficacy; (5) antigen circulation and its impact on the mechanism of action of ADC.
Understanding these attributes of target antigens and carefully considering how antigen selection may affect other aspects of ADC performance will help us design the best ADCs for clinical safety and efficacy in treating solid and hematologic tumors.
References:
1. Target Antigen Attributes and Their Contributions to Clinically Approved Antibody-Drug Conjugates (ADCs) in Haematopoietic and Solid Cancers. Cancers (Basel).2023 Mar; 15(6): 1845.
2. Impact of Endocytosis Mechanisms for the Receptors Targeted by the Currently Approved Antibody-Drug Conjugates (ADCs)—A Necessity for Future ADC Research and Development. Pharmaceuticals (Basel). 2021 Jul; 14(7): 674.

Click below “Yao Du”, follow for more exciting content
Disclaimer
The rules for pushing WeChat public accounts have changed again. If you don’t click “Looking” or haven’t set it as “Star Mark”, we may disappear in the vast sea of literature~ Click here, don’t miss the latest news from Yao Du!👇👇👇