Research Background
In patients with ST-segment elevation myocardial infarction (STEMI), approximately 50% have multivessel disease (MVD), which is associated with a poor prognosis, especially when there are three-vessel lesions or chronic total occlusions. Although emergency PCI is the standard treatment for STEMI, there is still controversy regarding the management strategy for nonculprit lesions (complete revascularization vs. treating only the culprit lesions). Previous studies have shown that complete revascularization may reduce the risk of ischemia-driven reintervention, but its impact on hard endpoints (death, reinfarction) is inconsistent.
This study aims to explore: which patient subgroups can benefit from FFR-guided complete revascularization?
Research Methods and Design
– Study Type: Post-hoc subgroup analysis of a randomized controlled trial (DANAMI 3-PRIMULTI study).
– Population: 627 STEMI patients with successful treatment of the culprit vessel and at least one nonculprit lesion (visual stenosis ≥50%).
– Grouping:
– Intervention Group: FFR-guided complete revascularization (PCI performed when nonculprit lesion FFR ≤0.80 or visual stenosis ≥90%).
– Control Group: Treatment of only the culprit vessel.
– Stratified Analysis:
– Number of vascular lesions (2-vessel vs. 3-vessel lesions).
– Degree of stenosis in nonculprit lesions (<90% vs. ≥90%).
– Lesion location (proximal vs. distal).
– Primary Endpoint: Composite endpoint of all-cause mortality, reinfarction, and ischemia-driven reintervention.
Key Results
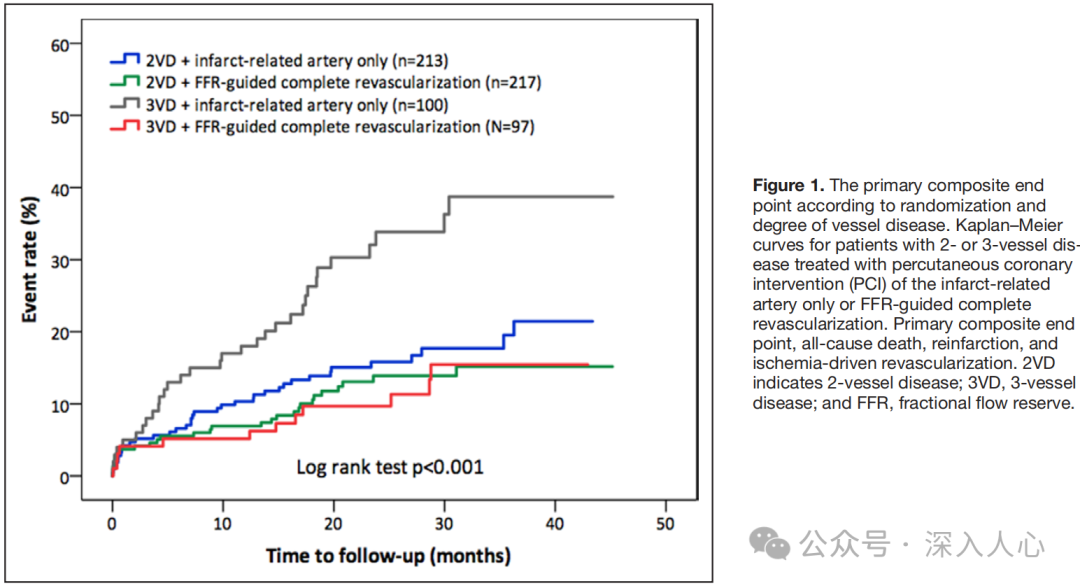
1. Patients with three-vessel lesions benefit significantly:
– The risk of the primary endpoint in the complete revascularization group was reduced by67% (HR 0.33, 95% CI 0.17-0.64, P=0.001).
– No significant difference in patients with two-vessel lesions (HR 0.77, P=0.29).
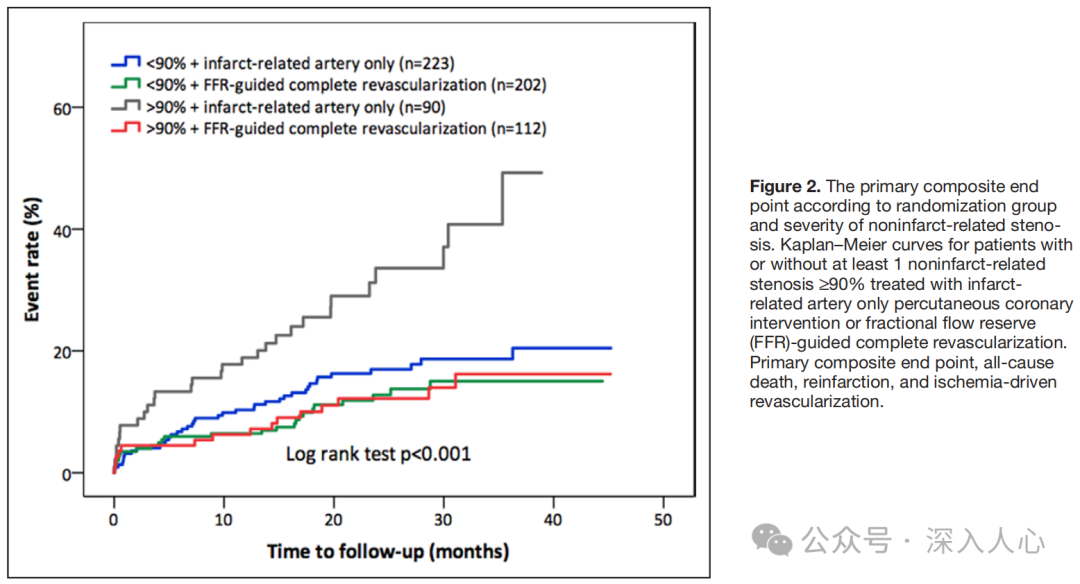
2. Patients with severe stenosis (≥90%) benefit significantly:
– Patients with nonculprit lesions ≥90% stenosis had a 68% reduction in the risk of the primary endpoint (HR 0.32, 95% CI 0.18-0.62, P=0.001).
– Patients with stenosis <90% showed no significant benefit (HR 0.72, P=0.21).
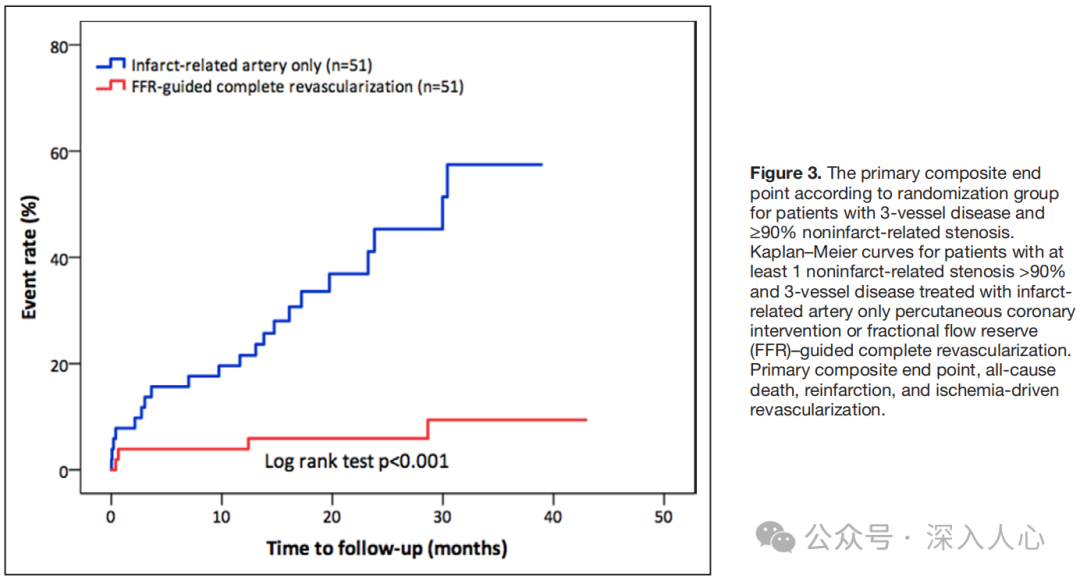
3. High-risk subgroup (three-vessel lesions + stenosis ≥90%) showed the most significant effect:
– The incidence of the primary endpoint decreased from 41% to 8% (relative risk reduction of 76%, HR 0.13, P<0.001).
– There was also a trend towards a decrease in the risk of death/reinfarction (HR 0.32, P=0.09).
4. Lesion location (proximal/distal) does not affect the benefit.
Clinical Significance
– Precise screening of high-risk patients: STEMI patients with three-vessel lesions and severe stenosis (≥90%) should prioritize FFR-guided complete revascularization to significantly reduce the risk of adverse events.
– Avoiding overtreatment: For patients with two-vessel lesions or mild stenosis (<90%) in nonculprit lesions, treating only the culprit lesions is safe.
– The value of FFR: Even with visually severe stenosis, FFR can optimize decision-making (some severely stenosed lesions may not be functionally significant).
Limitations and Controversies
– Post-hoc subgroup analysis: There is a risk of multiple comparisons, requiring prospective studies for validation.
– Sample size limitations: The power of subgroup analysis for hard endpoints (death, reinfarction) is insufficient.
– Timing of FFR measurement: In the study, FFR was measured 2 days post-PCI, which may avoid acute microcirculation interference, but the feasibility of this in clinical practice needs attention.
Practical Recommendations
1. Patients with three-vessel lesions + severe stenosis: FFR-guided complete revascularization is recommended.
2. Patients with two-vessel lesions or mild stenosis: Prioritize treatment of the culprit lesions, with nonculprit lesions managed based on symptoms or functional assessment.
3. Application of FFR: Even with visually severe stenosis ≥90%, it is recommended to assess functional significance with FFR to avoid unnecessary stent implantation.
Conclusion
This study provides a stratified strategy for the treatment of STEMI with multivessel disease: high-risk patients (three-vessel lesions + severe stenosis) should undergo complete revascularization, while low-risk patients can be managed conservatively. The precise guidance of FFR plays a key role in optimizing revascularization decisions, and larger studies are needed in the future to validate the long-term impact on hard endpoints.
References:Fractional Flow Reserve–Guided Complete Revascularization Improves the Prognosis in Patients With ST-Segment–Elevation Myocardial Infarction and Severe Nonculprit Disease A DANAMI 3-PRIMULTI Substudy (Primary PCI in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease: Treatment of Culprit Lesion Only or Complete Revascularization).
Circ Cardiovasc Interv. 2017;10:e004460. DOI: 10.1161/CIRCINTERVENTIONS.116.004460.
Reply084 PDF format of the original text is available.
This public account is a compilation of my study materials; conclusions and opinions are for reference only. Please be cautious when forwarding, and corrections and comments are welcome.