
Research Background
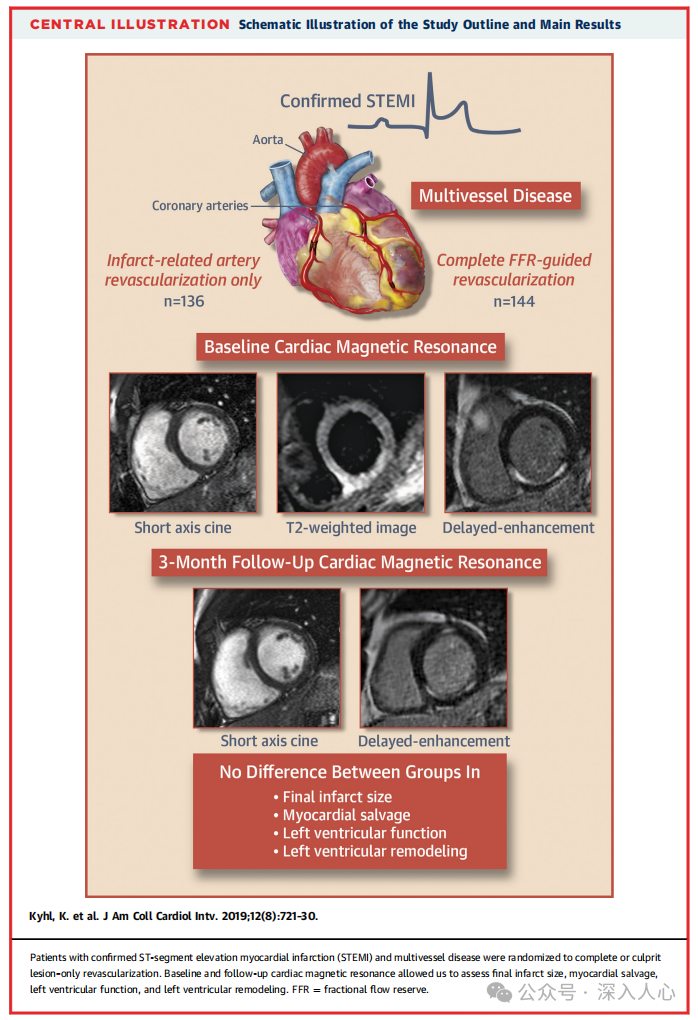
Patients with ST-segment elevation myocardial infarction (STEMI) combined with multivessel disease (MVD) account for approximately 45% of all STEMI patients, and they have a poorer clinical prognosis. Previous studies (such as PRAMI, CvLPRIT) have shown that complete revascularization (treating all significantly narrowed vessels) can reduce major adverse cardiovascular events (MACE) compared to treating only the culprit lesion, but its effects on left ventricular (LV) function, infarct size, and remodeling remain unclear.
Core Question: Does FFR-guided complete revascularization improve LV function, infarct size, and remodeling in STEMI patients with multivessel disease?
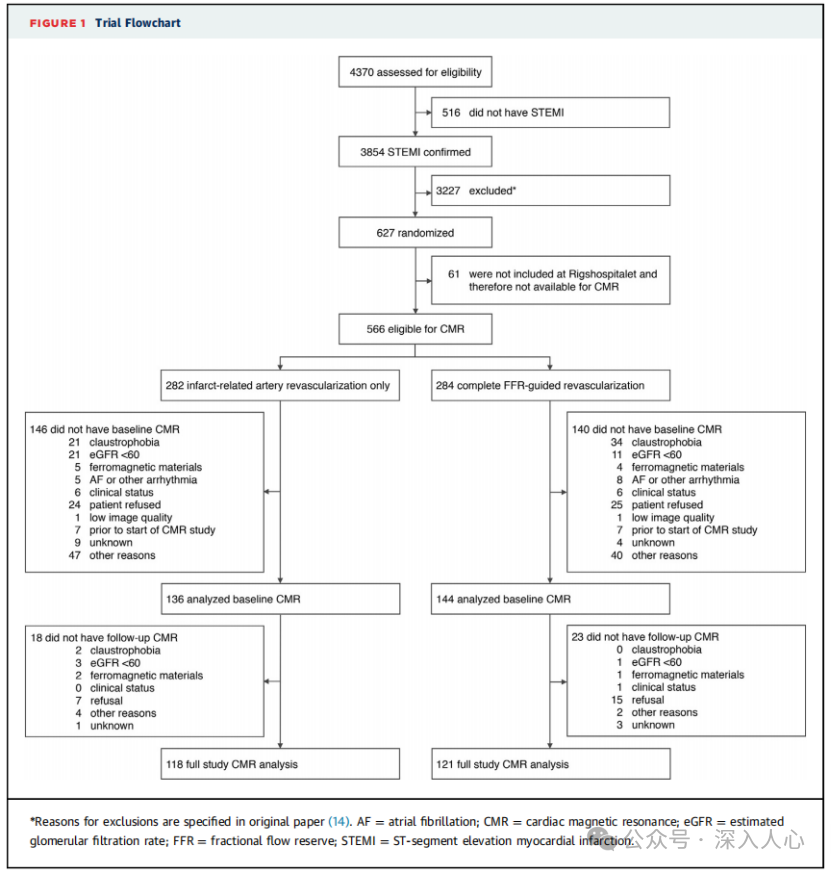
Study Design and Methods
Study Type:A predefined subgroup study of the DANAMI-3-PRIMULTI trial, a multicenter, randomized controlled trial.
Inclusion Criteria:
-Core Criteria: First STEMI (symptoms ≤12 hours), multivessel disease (non-culprit vessel stenosis ≥50%);
-Exclusion: Cardiogenic shock, need for CABG, contrast agent allergy, etc.
Grouping Strategy:
1. Complete Revascularization Group (n=144):FFR assessment of non-culprit vessels within 2 days after PCI of the culprit vessel (FFR ≤0.80 or stenosis >90% underwent PCI);
2. Culprit Lesion Only Group (n=136): Only PCI of the culprit vessel was performed.
Assessment Methods:
-Cardiac Magnetic Resonance (CMR): Assess LV ejection fraction (LVEF), LV end-systolic volume (LVESV), infarct size, and new non-culprit infarction at baseline (1 day post-PCI) and at 3 months follow-up.
Primary Endpoints:LVEF, LVESV, final infarct size, and new non-culprit infarction rate at 3 months.
Key Results
1. Baseline Characteristics and Treatment Strategies:
-No significant differences in baseline characteristics (age, diabetes, anterior wall infarction ratio, etc.) between the two groups;
-The complete revascularization group had a higher average number of implanted stents (2 vs. 1, P<0.001) and a longer total stent length (35mm vs. 18mm, P<0.001).
2. Comparison of CMR Parameters:
-Final infarct size: Complete revascularization group 11% vs. culprit only group 12% (P=0.62);
-LVEF: 59% vs. 58% at 3 months (P=0.39);
-LV remodeling: No difference in LVESV change (-7ml vs. -7ml, P=0.99).
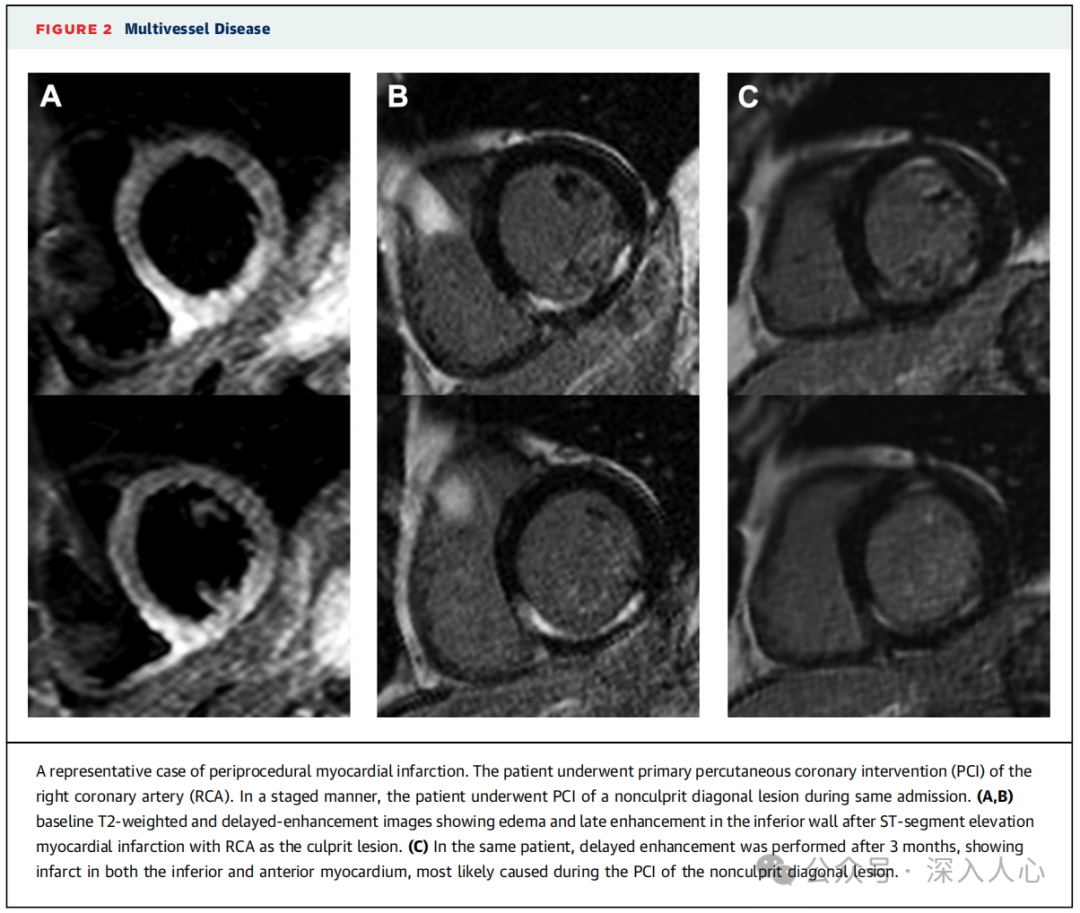
3. New Non-Culprit Infarction:
-The new non-culprit infarction rate was slightly higher in the complete revascularization group (4.9% vs. 0.8%, P=0.12), possibly related to intraoperative complications (such as type 4a myocardial infarction).
4. Subgroup Analysis:
-Regardless of whether there were three-vessel lesions, anterior wall infarction, or infarct size, there were no differences in LVEF, LVESV, and infarct size between the two groups.
Discussion and Clinical Implications
1. FFR-guided complete revascularization did not improve cardiac structure and function:
-Although complete revascularization may reduce subsequent ischemic events (as shown in the original DANAMI-3-PRIMULTI study), it did not translate into improvements in LV function or remodeling;
-Possible reasons: The supply area of non-culprit vessels is small, or the low ischemic burden lesions selected by FFR have limited impact on overall cardiac function.
2. Potential Risks of New Non-Culprit Infarction:
-The higher rate of new non-culprit infarction in the complete revascularization group (though not statistically significant) suggests that interventional procedures may lead to additional myocardial injury;
-Clinicians need to weigh the long-term benefits of complete revascularization against perioperative risks.
3. Comparison with Other Studies:
-PRAMI trial: Complete revascularization also did not improve LV function, but had a higher perioperative myocardial infarction rate;
-CvLPRIT trial: Complete revascularization increased the risk of multivessel infarction, but the follow-up time was shorter.
Study Limitations
1. Sample Size and Follow-up Time:
-Only 280 patients were included, limiting statistical power;
-3 months of follow-up may be insufficient to observe long-term LV remodeling.
2. Selection Bias:
-Some high-risk patients (such as those with heart failure or renal insufficiency) were excluded due to inability to complete CMR, which may underestimate the true differences.
3. Differences in Clinical Endpoints:
-The study primarily focused on imaging parameters and did not directly correlate with clinical endpoints (such as heart failure, mortality).
Conclusions and Future Directions
-Core Conclusion: In STEMI patients with multivessel disease, FFR-guided complete revascularization did not improve LV function, infarct size, or remodeling, but may increase the risk of perioperative myocardial infarction.
-Practical Recommendations:
-For patients with multivessel disease, the potential benefits of complete revascularization (reducing re-ischemia) should be weighed against the risks (procedure-related injury);
-Prioritize the treatment of high-risk non-culprit lesions (such as FFR ≤0.80, anatomically complex lesions).
-Future Research: Larger sample sizes and longer follow-up trials are needed to assess the long-term impact of complete revascularization on heart failure and mortality, and to explore the optimization value of new functional tools (such as QFR).
This study reveals the limitations of complete revascularization through precise assessment with CMR, suggesting that clinical decision-making should go beyond anatomical revascularization to focus on comprehensive optimization of function and prognosis.
References:Complete Revascularization Versus Culprit Lesion Only in Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Disease A DANAMI-3–PRIMULTI Cardiac Magnetic Resonance Substudy.J Am Coll Cardiol Intv 2019;12:721–30
Reply085Available in PDF format.The public account is a compilation of my study materials, and the conclusions and opinions are for reference only. Please be cautious when forwarding, and feel free to correct or leave a message.