Research Background
With the increasing number of elderly patients receiving primary percutaneous coronary intervention (PPCI), the management strategies for non-culprit lesions have become controversial. Although multiple studies support that complete revascularization (treating all significant stenosed vessels) can improve prognosis, the benefits for elderly patients (≥75 years) remain unclear due to their comorbidities and shorter life expectancy. This study, based on the DANAMI-3-PRIMULTI trial, aims to explore the impact of age on the prognosis of complete revascularization (guided by FFR) versus a strategy of treating only the culprit lesions.
Study Design and Methods
Study Type: Subgroup analysis of a prospective randomized controlled trial (DANAMI-3-PRIMULTI).
Inclusion Population:
– Core Criteria: STEMI with multivessel disease (non-culprit vessel stenosis ≥50%), randomized after receiving PPCI;
– Grouping:
1. Culprit lesion only group (n=60): PCI performed only on the culprit vessel;
2. Complete revascularization group (n=50): FFR-guided treatment of all non-culprit lesions (PCI for FFR ≤0.80 or stenosis >90%).
Primary Endpoint: Composite endpoint (all-cause mortality, non-fatal reinfarction, ischemia-driven non-infarction-related revascularization), with a median follow-up of 27 months.
Statistical Methods: Cox proportional hazards model, Kaplan-Meier survival analysis, interaction tests.
Key Results
1. Baseline Characteristics Differences:
– Patients aged ≥75 years (n=110, 17.5% of total) had a higher proportion of females (32% vs. 16.6%, p<0.001), more hypertension (58.2% vs. 41.0%, p=0.001), lower hemoglobin (8.3 vs. 8.7 mmol/L, p<0.001), and higher creatinine (87 vs. 74 mmol/L, p<0.001).
– Treatment Strategy: No significant differences in baseline characteristics between the two groups (culprit lesion only vs. complete revascularization).
2. Primary Endpoint:
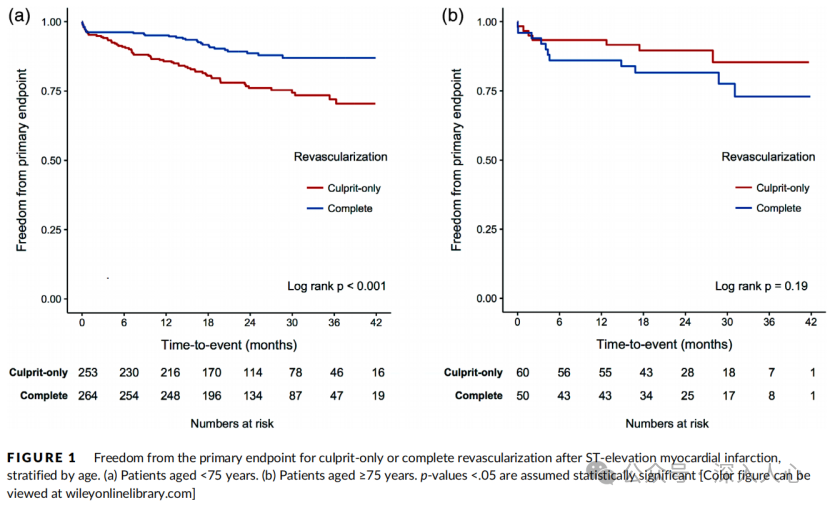
– Patients aged ≥75 years: The incidence of the composite endpoint in the complete revascularization group was 22%, while in the culprit-only group it was 15% (HR=1.49, 95% CI 0.57–4.65, p=0.19), with no significant difference.
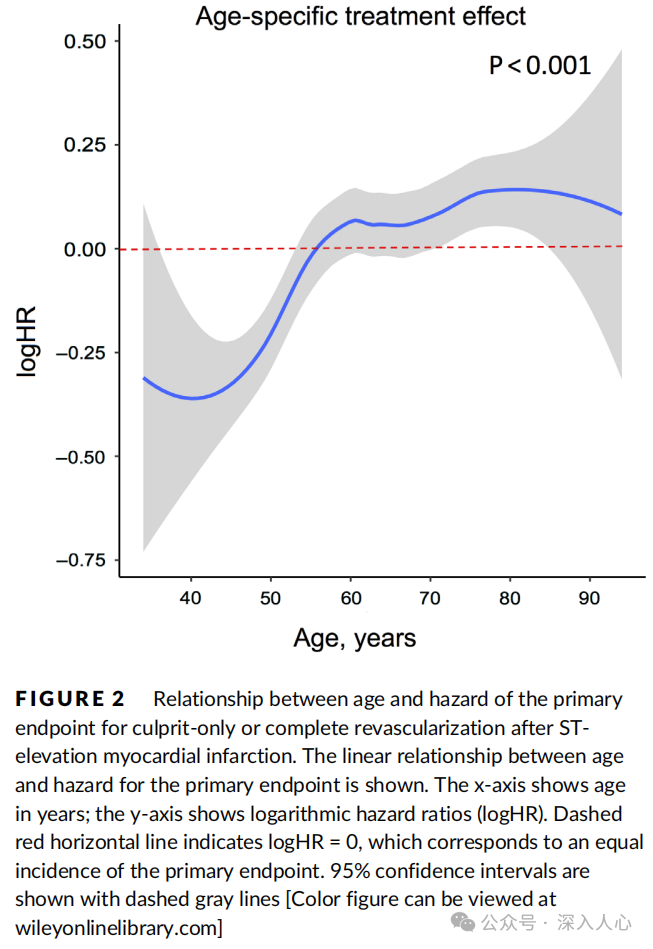
– Age Interaction: There was a significant interaction between age and treatment strategy (p<0.001), with the prognostic advantage of complete revascularization disappearing at age ≥75 (Figure 1).
3. Secondary Endpoints:
– All-cause mortality: 14% in the complete revascularization group vs. 7% in the culprit-only group (p=0.29);
– Reinfarction: 4% in both groups (p=0.80);
– Ischemia-driven revascularization: 4% in the complete revascularization group vs. 5% in the culprit-only group (p=0.50).
4. Safety:
– Bleeding Events: The rate of BARC 1-2 bleeding in patients aged ≥75 years was significantly higher than in those <75 years (70% vs. 55.4%, p=0.006), with a higher rate in the complete revascularization group (80% vs. 61.7%, p=0.04);
– Contrast-Induced Nephropathy: No difference between the two groups (15.5% vs. 14.5%, p=0.54).
Discussion and Clinical Implications
1. Limitations of Complete Revascularization in Elderly Patients:
– Prognosis Not Improved: This may be related to the high risk of non-cardiovascular death in elderly patients and atypical symptoms leading to lower demand for revascularization;
– Increased Bleeding Risk: Complete revascularization requires multiple procedures, increasing the risk of bleeding (especially BARC 1-2).
2. Importance of Age Stratification:
– Significant Interaction: After age ≥75, the benefits of the composite endpoint from complete revascularization disappear, supporting individualized treatment;
– Symptom-Driven Strategy: For elderly patients, prioritize treating the culprit lesions, and decide whether to intervene on non-culprit lesions based on symptoms or evidence of ischemia.
3. Opportunities for Technical Optimization:
– Radial Artery Access: May reduce bleeding risk;
– Non-invasive Functional Assessment: Combining FFR or QFR to optimize the selection of non-culprit lesions, reducing unnecessary interventions.
Study Limitations
1. Small Sample Size: Only 110 patients aged ≥75, with few events, leading to insufficient statistical power;
2. Selection Bias: Included patients were relatively healthy, not covering frail or very elderly (≥90 years) populations;
3. Follow-up Duration: A median of 27 months may be insufficient to observe long-term differences in heart failure or mortality rates.
Core Conclusion
In patients aged ≥75 years with STEMI and multivessel disease, FFR-guided complete revascularization did not improve the composite endpoint and increased the risk of bleeding, supporting a symptom-driven staged revascularization strategy.
References:The benefit of complete revascularization after primary PCI for STEMI is attenuated by increasing age: Results from the DANAMI-3-PRIMULTI randomized study.Catheter Cardiovasc Interv. 2020;1–8.
Reply087 PDF version of the original text is available.
This public account is a compilation of my study materials; conclusions and opinions are for reference only. Please be cautious when forwarding, and corrections or comments are welcome.