Blepharospasm (BSP) is a focal dystonia characterized by involuntary closure of the eyelids and difficulty in opening them, usually caused by spasms of the orbicularis oculi muscle. Its prevalence varies significantly by region, approximately (20-133)/million, and it is more common in women aged 50-70, with a male-to-female ratio of about 1:2.3. Risk factors include a family history of dystonia, history of head trauma with altered consciousness, and history of blepharitis or keratitis.
The initial clinical symptoms of BSP patients are mild, often presenting as increased blinking or a constant urge to close the eyes, and the condition typically progresses slowly, with late-stage persistent eyelid spasms potentially leading to functional blindness. Symptoms are often triggered or worsened by stress, anxiety, and fatigue, while certain specific actions such as talking, singing, opening the mouth, chewing, or touching the cheek can provide relief, referred to as “sensory tricks.”
Compared to other types of focal dystonia, BSP is more likely to spread to adjacent areas, with more than 50% of patients developing other forms of dystonia within 5 years of onset, commonly oromandibular dystonia (OMD) and Meige syndrome. BSP can be classified into primary BSP (also known as idiopathic BSP) and secondary BSP, the latter often resulting from brain hemorrhage, infarction, vascular malformations, multiple sclerosis, and tardive dyskinesia. This article reviews the research progress on the etiology, diagnosis, differential diagnosis, disease assessment, and treatment options for primary BSP.
01
Pathogenesis

Currently, the specific pathogenesis of BSP has not been fully elucidated. It involves aspects of pathophysiology, pathological anatomy, functional imaging, and genetics, and is not an isolated occurrence but rather the result of multiple contributing factors. The following sections elaborate on the relevant research regarding the mechanisms of BSP occurrence.
1.1 Pathophysiology
Electromyography (EMG) examinations show that the blink reflex frequency is increased in BSP patients. The blink reflex consists of two phases: the R1 phase begins with corneal stimulation, transmitted via the ophthalmic branch of the trigeminal nerve to the brainstem trigeminal nucleus, then to the bilateral facial nerve nuclei, leading to the R2 phase; the R2 phase is the efferent phase of the reflex, carried by the temporal, zygomatic, and buccal branches of the facial nerve, causing bilateral facial expression muscle contractions, with R2 phase signals significantly enhanced in BSP patients compared to healthy subjects. Among them, neurotransmitters such as dopamine, acetylcholine, gamma-aminobutyric acid, and serotonin play important roles in the signal transduction pathway, providing potential therapeutic targets for oral medications.
1.2 Pathological Anatomy
Due to the relative rarity and non-fatal nature of dystonia, there are few pathological studies based on autopsy tissues. In 2021, Fagan et al. conducted a review of related literature and found that the reported brain tissue pathological abnormalities in 12 BSP patients were not consistent. Subsequently, Fagan et al. obtained 7 BSP patients with or without other dystonia from the Maryland University Developmental Disorders Tissue Bank, using 9 patients without BSP or other types of dystonia as a control group. Pathological studies of cerebellar tissue sections revealed that the density of Purkinje neurons in the cerebellum was significantly reduced in BSP patients compared to the control group. This finding is consistent with previous reports of similar results observed in the brain tissue of patients with cervical dystonia, which may underlie certain subtle imaging changes in BSP.
1.3 Functional Imaging
Studies using 18FDG-PET imaging of BSP patients found that, compared to the control group, the most significant areas of increased glucose uptake were the right caudate, inferior frontal gyrus, right posterior cingulate gyrus, left middle occipital gyrus, right fusiform gyrus, and left anterior cingulate gyrus, while the most significant areas of decreased uptake were the left cerebellar hemisphere, thalamus, and inferior frontal gyrus. Functional magnetic resonance imaging (fMRI), utilizing blood-oxygen-level-dependent effects, can acquire neural network activity in different regions and is currently a research hotspot. Baker et al. found that the anterior visual cortex, anterior cingulate cortex, primary motor cortex, central thalamus, and superior cerebellum were significantly activated in BSP patients compared to the control group. Increasing evidence suggests that BSP patients experience extensive reorganization of the brain’s white matter neural network, primarily located in the motor cortex of the head and face and basal ganglia, potentially related to facial hyperactivity. Hou et al. used resting-state fMRI and graph analysis to explore the functional connectivity of brain tissue neural networks in BSP patients, revealing that the local connectivity of the sensorimotor network, cerebellum, and default mode network was reduced, indicating potential pathophysiological mechanisms of BSP.
1.4 Genetics
BSP is mostly sporadic, with about 25% of patients having a family history of movement disorders. Due to the low incidence of BSP, incomplete gene expression, and genetic heterogeneity, identifying specific genetic defects is very challenging. In 2021, Ma et al. compiled a list of possible gene mutations associated with BSP occurrence through literature review, as shown in Table 1.
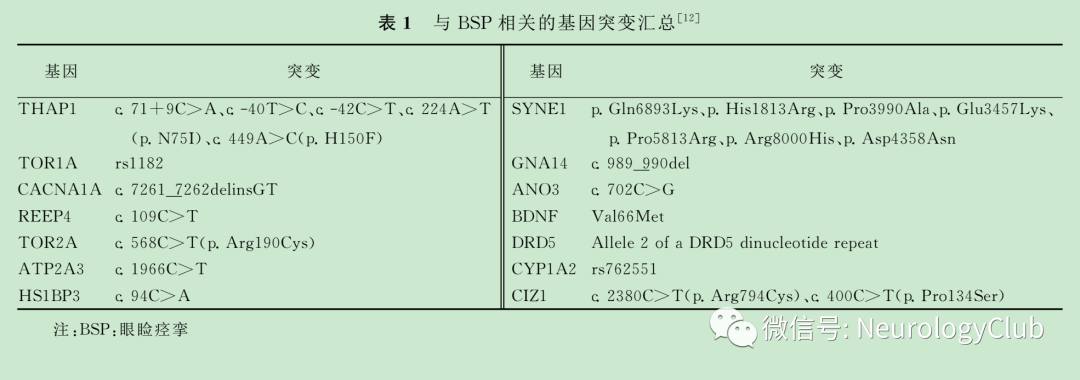
Most of these genes are derived from case reports in different regions, with some from case-control studies or cohort studies. Among them, large-scale clinical studies conducted in Italy and Switzerland showed that TOR1A rs1182 and CYP1A2 rs762551 were significantly associated with BSP. A study on the Chinese population collected clinical diagnoses of 20 BSP patients and analyzed 151 genes related to movement disorders through next-generation sequencing, revealing that 7 patients had SYNE1 mutations, 2 had CIZ1 mutations, 2 had CACNA1A mutations, 2 had LRRK2 mutations, and 2 had FUS mutations, while 2 patients had no mutations in any of the 151 genes, and 7 patients had mutations in 2 genes simultaneously; only 2 patients had a family history of BSP, with SYNE1 and CIZ1 gene mutations detected, suggesting that SYNE1 and CIZ1 gene mutations are the main genetic factors leading to BSP. However, due to the small sample size of current studies and the continuous discovery of new genes related to BSP, the role of genetic factors in the pathogenesis of BSP requires further research. It is noteworthy that despite many gene mutations being found in BSP patients, the mutation rates of these genes are low, necessitating larger-scale whole-exome sequencing studies to identify relevant mutations and functionally validate them.
02
Diagnosis

Currently, there is no unified diagnostic standard for BSP, which is mainly diagnosed clinically based on the patient’s typical symptoms. When symptoms are atypical or in the early stages of the disease, misdiagnosis or missed diagnosis often occurs. A Japanese study showed that approximately 60% of patients consulted at least 5 doctors before diagnosis, and one-third of patients were diagnosed more than 5 years after the onset of symptoms.
A clinical diagnostic model is based on the typical synchronized contraction of the bilateral orbicularis oculi, sensory tricks, and increased blinking, with a sensitivity of 93% and specificity of 90%. Building on previous research, Defazio et al. conducted a large multicenter clinical study, collecting data from 211 BSP patients and 166 healthy controls, comparing the consistency of the blepharospasm screening questionnaire items with clinical diagnoses, finding that the synchronized contraction of the bilateral orbicularis oculi had the highest diagnostic sensitivity (96%), while sensory tricks had the highest diagnostic specificity (92%). However, this diagnostic model has shortcomings, neglecting non-motor symptoms in BSP patients, such as psychological disorders, sleep disturbances, sensory symptoms, and cognitive impairments.
03
Differential Diagnosis

When BSP patients present with atypical symptoms or are in the early stages of the disease, they can be easily confused with dry eye syndrome, chronic conjunctivitis, myasthenia gravis (MG), hemifacial spasm (HFS), tic disorders, tardive dyskinesia (TD), and psychogenic BSP.
3.1 Dry Eye Syndrome
Refers to any cause leading to reduced tear production, abnormal tear quality or dynamics, resulting in symptoms such as dryness, itching, foreign body sensation, visual fatigue, blurred vision, photophobia, and burning sensations. Ophthalmological examinations such as tear secretion tests <5mm and tear film break-up time <10s can assist in diagnosis. Antibody-related tests help determine immune-related causes (such as Sjögren’s syndrome) of dry eye syndrome.
3.2 Chronic Conjunctivitis
Refers to chronic inflammation of the conjunctiva caused by various factors, including bacterial infections, environmental irritants, and poor lifestyle habits, with clinical features including discomfort, white frothy discharge, and conjunctival hyperemia; local application of antibiotic eye drops can relieve discomfort.
3.3 MG
Is an autoimmune disease characterized by impaired synaptic transmission at the neuromuscular junction mediated by antibodies, in which ocular MG presents with ptosis and diplopia, typically worsening throughout the day, with a positive fatigue test and effectiveness of cholinesterase inhibitors.
3.4 HFS
Typically presents unilaterally, affecting not only the orbicularis oculi but also other facial muscles innervated by the facial nerve, such as the buccinator and masseter muscles; the cause is often compression of the facial nerve by distorted blood vessels in the posterior cranial fossa or distal segments.
3.5 Tic Disorders
Commonly occur in children, characterized by frequent motor tics or vocal tics. Most affected children also exhibit attention deficit hyperactivity disorder, obsessive-compulsive disorder, etc.
3.6 TD
Associated with long-term use of dopamine receptor antagonists, patients often have a history of antipsychotic medication use, which can affect the facial and neck regions, causing tongue protrusion, chewing, mouth rinsing, jaw deviation, or neck twisting, and can also affect the limbs and trunk, presenting with chorea-like movements. This has some differences from the clinical phenotype of BSP.
3.7 Psychogenic BSP
Should be considered when patients present with atypical symptoms and no other causes can be identified. Assessing psychological factors and providing interventions before treatment can also improve symptoms.
04
Disease Assessment

Currently, scales used to assess the severity of BSP include the Jankovic Rating Scale (JRS), the Blepharospasm Severity Scale (BSS), the Blepharospasm Disability Scale (BDS), and the Blepharospasm Disability Index (BSDI). In addition to the above scales specifically for BSP, there are also several scales widely used by clinicians to assess the severity of focal dystonia, including the Global Dystonia Rating Scale (GDRS), Burke-Fahn-Marsden Dystonia Rating Scale (BFMDRS), and Unified Dystonia Rating Scale (UDRS). Among these, the most widely used scales are JRS and BSDI. JRS is used to evaluate the severity and frequency of BSP symptoms, while BSDI assesses the impact of BSP on the patient’s daily activities.
05
Treatment

5.1 Oral Medications
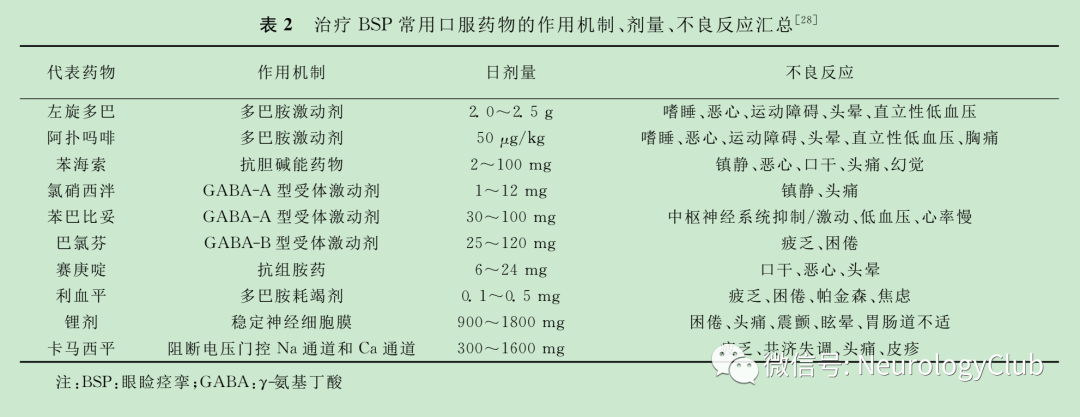
Include dopaminergic drugs, anticholinergic drugs, gamma-aminobutyric acid receptor agonists, antihistamines, and monoamine oxidase inhibitors. Representative drugs, mechanisms of action, common dosages, and side effects are shown in Table 2. A questionnaire study involving 1653 BSP patients found that 43% of those receiving oral medication treatment experienced symptom improvement, with more than half experiencing less than 50% improvement, which is often temporary. Overall, the efficacy of oral medications is uncertain, and drug-related side effects limit their clinical application.
5.2 Botulinum Toxin Local Injection
Type A botulinum toxin (BTX-A) local injection is the first-line treatment for focal dystonia and is also suitable for BSP. Botulinum toxin selectively acts on peripheral cholinergic nerve terminals, inhibiting the release of acetylcholine, resulting in temporary paralysis of the injected muscle. The average onset time of BTX-A is 2-7 days, with effects lasting 3-4 months, and 90% of patients can achieve moderate improvement. A 20-year clinical study showed that BTX-A has good tolerance and safety, even during a follow-up period of up to 29 years. In 2021, Kako et al. observed 88 patients receiving BTX-A local injection, with results showing improvements in quality of life and psychological status among BTX-A treated patients. Systemic weakness caused by BTX-A local injection is extremely rare, while ptosis, blurred vision, or diplopia are relatively uncommon and generally resolve within weeks. It is important to note that most patients require repeat injections to maintain efficacy. Currently, there are no randomized controlled studies to provide the optimal treatment interval and dosage for BTX-A. Some researchers are concerned that long-term BTX-A treatment may lead to the development of neutralizing antibodies, diminishing treatment efficacy. Czyz et al. conducted a 20-year follow-up study on 12 patients with dystonia undergoing long-term BTX-A treatment, finding no antibodies detected in these patients. A meta-analysis included 43 studies involving 8834 patients treated with BTX-A, showing that the occurrence of neutralizing antibodies was significantly related to the duration of BTX-A use, with the highest incidence of neutralizing antibodies among dystonia patients (7.4%) compared to other diseases treated with BTX-A.
5.3 Surgical Treatment
Severely refractory BSP patients may consider surgical treatment. Facial nerve section and frontalis suspension surgery have been eliminated due to poor efficacy and high recurrence rates. Orbicularis oculi resection can remove all muscle tissue involved in BSP while preserving the frontalis muscle necessary for eyelid closure, improving the appearance around the eyes with relatively concealed scarring, achieving a high acceptance rate and good efficacy among severe BSP patients. Timlin et al. followed up 24 BSP patients undergoing orbicularis oculi resection for 24 months, finding that 83% of patients had significant symptom improvement, with reductions in JRS and BSDI scores, while 17% experienced symptom worsening. Overall, orbicularis oculi resection is a good treatment option for patients who do not respond well to oral medications and BTX local injections.
5.4 Transcranial Magnetic Stimulation
Repetitive transcranial magnetic stimulation (rTMS) is a neuromodulation technique that achieves therapeutic effects by modulating cortical and subcortical networks related to clinical symptoms. Kranz et al. conducted a double-blind, placebo-controlled study on 12 BSP patients, stimulating the anterior cingulate cortex, and found that low-frequency rTMS could not only improve subjective symptoms but also showed “normalization” of the blink reflex circuit. A six-month clinical study by Yin et al. indicated that BTX-A combined with rTMS could effectively prolong the duration of symptom relief and significantly improve patients’ depression and anxiety, suggesting that combined treatment methods for BSP may have a better prospect.
5.5 Deep Brain Stimulation (DBS)
DBS can be used for refractory dystonia patients who do not respond well to oral medications or BTX-A treatment. The globus pallidus internus (GPi) and subthalamic nucleus (STN) are classic targets for treating dystonia. Currently, there is a lack of large-scale clinical studies on DBS surgical treatment for BSP, and relevant case reports are also limited. In 2021, Evidente et al. reported a case of a 34-year-old male with secondary BSP caused by long-term use of antipsychotic medications, who did not respond well to drug treatment and BTX-A, and after undergoing GPi-DBS treatment, his symptoms completely disappeared during a 30-month follow-up. Overall, due to limited experience, careful consideration of risks and benefits is required when using DBS to treat BSP. Notably, a study by Pandey et al. showed that 50% of BSP patients may progress to segmental dystonia such as Meige syndrome within 5 years of onset. Numerous studies have confirmed that DBS is effective for treating Meige syndrome with few complications. A meta-analysis included 23 studies with a total of 115 patients, of whom 94 received GPi stimulation and 21 received STN stimulation, showing significant improvement in the movement scores (BFMDRS-M) and disability scores from baseline at the last follow-up. Common complications of DBS surgery include intracranial hemorrhage, infection, seizures, sensory abnormalities, and muscle spasms, requiring long-term regular follow-up and adjustment of parameters based on symptoms.
In summary, the etiology and pathogenesis of BSP have not been clarified, currently believed to be the result of the interaction of genetic and environmental factors, and future research needs to focus more on whole-genome sequencing and gene functional genomics; BSP lacks a unified diagnostic standard, with the characteristics of bilateral orbicularis oculi synchronized contractions and sensory tricks aiding in clinical diagnosis; the JRS and BSDI scales can be used for disease assessment in BSP patients. The first-line treatment for BSP is BTX-A local injection, with variable efficacy of oral medications; for refractory BSP, orbicularis oculi resection may be considered, and rTMS and DBS can also effectively improve symptoms, but large-scale clinical studies are needed for further confirmation.
Chinese Journal of Neuroimmunology and Neurology September 2022, Volume 29, Issue 5
Authors: Wang Xixi, Wan Xinhua (Department of Neurology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences)

