Click the blue words to follow us

Introduction
Diabetic foot is one of the most serious complications of diabetes. Diabetic foot ulcers are characterized by difficulty in healing, high recurrence rates, high disability rates, and high treatment costs. Therefore, conducting risk prediction and protective interventions for diabetic patients with high-risk foot ulcers can help reduce the risk of foot ulceration. Diabetic foot aids, as an important auxiliary means to slow down the occurrence of foot ulcers in diabetic patients and extend the recurrence cycle of ulcers, will continuously develop towards digitization and intelligence in the future.
Research Background
Diabetic foot refers to the lower limb infections, ulcer formations, and/or deep tissue destruction caused by diabetic patients due to combined neuropathy and various degrees of lower limb vascular diseases. It is one of the severe complications of diabetes, with high recurrence rates, high disability rates, and high treatment costs. Research shows that the lifetime incidence of diabetic foot ulcers is between 19% and 34%[1]. There are many diabetic patients in our country, and the situation of foot care for patients is severe.
Concentrated plantar pressure and ischemia of foot tissues are important influencing factors causing ulcers in diabetic patients. Especially for diabetic patients with neuropathy, the protective sensation of the foot is weakened or even lost, making them unable to feel discomfort and pain during walking, thus leading to the occurrence and continuous deterioration of ulcers. Therefore, offloading the abnormal high pressure on the plantar surface and improving blood flow perfusion in the feet can help prevent ulcer occurrence and alleviate ulcer deterioration.
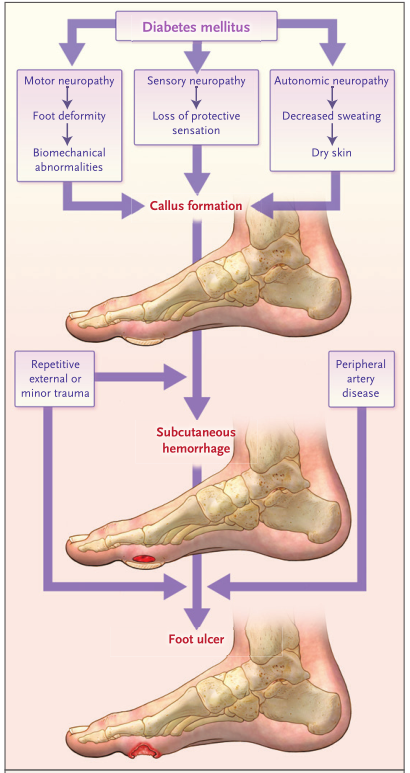
Figure 1: Common pathways of occurrence and recurrence of diabetic foot ulcers (Armstrong et al. 2017)
Current Research Status
1
Methods and Technologies for Risk Assessment of Diabetic Foot Ulcers
Abnormal plantar pressure distribution or stress concentration can further cause damage and ulcer deterioration in the foot tissues of diabetic patients; thus, it is essential to monitor and assess the daily plantar pressure of diabetic patients. Due to the convenience and quantification of measurements, peak plantar pressure (PPP) is commonly used as an indicator to assess the risk of diabetic foot ulcers and the effectiveness of offloading shoes. Owings et al.[2] proposed a safe threshold for the maximum pressure peak inside shoes for diabetic foot patients of 207kPa. This threshold has also been used by many researchers as an indicator to evaluate the effectiveness of insoles in offloading. However, Lavery et al.[3] pointed out that using only PPP as a predictor for ulcer occurrence has low accuracy. Plantar peak pressure gradient (PPG) can further reflect the rate of pressure spatial variation around the plantar PPP area, which is usually related to shear forces during walking and can help predict the risk of ulcer occurrence. Cumulative pressure load considers the magnitude of external mechanical forces and the duration of their application, reflecting the cumulative stimulus degree of physical load on diabetic feet over time. Pu et al.[4] suggested that blood flow response under cumulative pressure load can better reflect the protective response capacity of soft tissues in diabetic feet to external mechanical forces and can be used to assess the risk of ulcer occurrence in diabetic feet. Additionally, some researchers have characterized the stress levels of soft tissues in diabetic feet by calculating the internal tissue stresses on soft tissues and joints using digital models, providing a more direct reflection of changes in soft tissue characteristics.
Timely detection of potential inflammation before skin breakdown can allow for early intervention treatment of foot tissues, reducing the risk of diabetic foot ulcers. Temperature differences in foot skin are often used to reflect internal tissue inflammation. Researchers have measured and validated that when the temperature difference between the two feet is less than 1.5℃, the foot tissues show no pathological characteristics; when the temperature difference between the two feet or a certain area of one foot exceeds 2℃, it indicates local inflammation or infection; if the temperature difference exceeds 3℃, it indicates a diffuse infection in the foot. Additionally, foot skin temperature has also been shown to indirectly reflect the shear forces experienced by the skin, with higher tissue temperatures potentially indicating internal inflammation or excessive shear forces (Figure 2)[5].
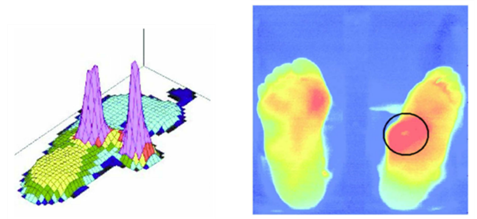
Figure 2: Temperature distribution map of diabetic patients’ feet (Bus et al. 2016)
Microcirculation is one of the most basic sites for the exchange of substances between blood and tissue cells in the human body. The blood supply and oxygenation, as well as the stress response capabilities of microcirculation, are closely related to the health status of diabetic patients’ feet. Indicators such as skin blood flow perfusion, blood oxygen saturation, transcutaneous oxygen partial pressure, and pressure reactive hyperemia can be used to reflect the blood supply and oxygenation levels of soft tissues in the feet, as well as the protective response capabilities of foot microcirculation to mechanical stimuli. Microscopic techniques can also be used to assess the diameter, quantity, and distribution of capillaries in skin tissues. Due to the high requirements of sensors measuring microcirculation-related indicators for measurement environments and relative displacements, and the relatively high costs of these sensors, there are few portable microcirculation measurement devices available for foot movement environments. Since skin temperature has a good correlation with skin blood flow, skin temperature parameters can also be used to indirectly reflect the microcirculation blood flow situation at the monitored site.
The humidity of the shoe environment has a significant effect on skin damage. Humidity not only affects the evaporation of sweat from the skin but also alters the mechanical properties of the skin tissues. When environmental humidity increases, the shear forces on the skin are correspondingly increased, making foot tissues more prone to injury. Monitoring the humidity of the shoe environment in diabetic patients helps accurately assess the risk of foot injuries and timely prevent foot damage.
2
Protection Methods and Technologies for Diabetic Foot Ulcers
Re-optimizing the distribution of plantar pressure, enhancing the protective response capabilities of soft tissues and microcirculation to external mechanical stimuli, alleviating foot pain, and promoting angiogenesis and tissue regeneration are effective ways to reduce the risk of ulcer occurrence and promote wound healing in diabetic patients. Currently, commonly used protective methods include pressure offloading aids, exercise therapy, vibration therapy, pneumatic compression therapy, heat therapy, transcutaneous electrical nerve stimulation, and extracorporeal shock wave therapy.
Pressure offloading insoles/shoes are one of the most common foot aids and are frequently used conservative treatment methods for diabetic foot patients. High plantar pressure during daily activities is a critical factor leading to the occurrence and recurrence of foot ulcers. Therefore, the guidelines from the International Working Group on the Diabetic Foot (IWGDF)[6] recommend that diabetic patients use customized shoes to achieve a reduction in peak plantar pressure. Pressure offloading insoles/shoes can be categorized into various types, including total contact insoles, plantar stress optimization insoles, honeycomb pressure relief insoles, forefoot and rearfoot offloading shoes, and flexible fit shoes. According to the different tissue lesions and bone deformities of diabetic patients’ feet, orthotic methods can also be used to stabilize or support deformed feet to prevent further development of deformities and restore normal functional positions, or by deepening the heel cup of the insole, adding metatarsal pads, or creating localized depressions in the insole to accommodate and protect feet with plantar pain or ulcer risk. Other diabetic foot pressure offloading aids include total contact insoles and orthotics, used for promoting ulcer healing, correcting foot deformities, and assisting walking.

Figure 3: Diabetic foot pressure offloading insoles and shoes (Image source: Internet)
Exercise therapy is one of the most effective management methods for diabetic complications and has been proven to improve health indicators such as blood circulation, blood sugar levels, ankle-brachial index, cardiopulmonary endurance, and muscle strength. The American Diabetes Association recommends that type 2 diabetes patients engage in at least 150 minutes of moderate-intensity aerobic exercise per week. Recent research by Pu et al.[7] also found that appropriate exercise doses not only do not increase the risk of foot ulcers but can also reduce the stiffness of soft tissues in diabetic patients’ feet and improve skin microcirculation levels. However, related studies also indicate that for diabetic patients with neuropathy, particular caution should be exercised regarding the intensity of exercise training to avoid excessive load stimulation on the feet, increasing the likelihood of foot injuries.
Vibration therapy can induce the production of NO in endothelial cells and promote the expression of nitric oxide synthase (NOS) by applying vertical and horizontal forces to skin tissues, facilitating microvascular dilation; at the same time, vibration stimulation can also induce the activation of polymodal receptors on the skin surface, triggering the release of neuropeptides and inducing microvascular dilation, thereby increasing blood flow. Furthermore, vibration has been shown to alleviate muscle tissue damage and oxidative damage caused by cumulative mechanical forces, promoting angiogenesis and wound healing. Current studies have found that appropriate frequencies and amplitudes of vibration stimulation can significantly increase skin blood flow in diabetic patients, and the protective effects are related to the duration of the vibration intervals[8]. Additionally, full-foot vibration interventions have been shown to effectively reduce the reactive hyperemia levels after obstructive pressure stimuli on the feet, alleviating stress injuries to the feet. Therefore, vibration, as a new protective treatment method, has promising application prospects.
Pneumatic compression therapy is a physical intervention method that improves blood circulation in limbs by applying uniform and regular mechanical forces to the limbs, mainly by increasing the pressure difference between arteries and veins, enhancing the production of endothelial relaxing substances, and promoting the reflex pauses of small veins and small arteries to increase arterial blood flow. Related studies have proven that pneumatic compression interventions can effectively increase skin blood flow in the feet of diabetic patients, and the therapeutic effects are related to the treatment site, intervention frequency and mode, compression pressure, and the patients’ own pathophysiological indicators[9]. Due to the non-invasive nature, minimal side effects, and good comfort of pneumatic compression therapy, patient compliance is relatively high, and the range of applicability is broad.
Heating therapy: Due to the effects of neuropathy and microvascular disease, many diabetic patients experience impaired temperature regulation. Damage to temperature regulation not only leads to abnormal blood flow distribution and exacerbates peripheral circulation disorders but also affects the timely contraction and relaxation of blood vessels, which over time can lead to increased ischemia in the distal limbs of diabetic patients and an increased risk of foot ulcers. Heating interventions such as water baths, hot compresses, and far-infrared lamps are commonly used methods to raise tissue temperatures, promote peripheral circulation[10], thereby increasing tissue nutrition, reducing infection susceptibility, improving wound healing, and promoting soft tissue repair. Applying heat to the skin can activate nitric oxide synthase to synthesize endothelial nitric oxide, which then diffuses to surrounding smooth muscles to activate cyclic GMP, increasing potassium permeability, relaxing vascular smooth muscles, and enhancing blood flow to the skin.
Transcutaneous electrical nerve stimulation (TENS) is a non-pharmacological, non-invasive treatment method that alleviates pain through peripheral and central mechanisms, primarily by applying electrical currents to nerve fibers via surface electrodes to stimulate nerves, triggering the release of endogenous opioids, altering electrical transmission, and dilating blood vessels. Diabetic patients typically have varying degrees of peripheral neuropathy. Researchers have attempted to apply TENS to diabetic peripheral neuropathy and found that TENS can effectively alleviate patients’ pain[11].
Research reports indicate that extracorporeal shock wave therapy (ESWT) has positively impacted the treatment of flaps and diabetic foot ulcers and has a certain positive effect on promoting wound healing. In animal experiments, ESWT has induced neovascularization and upregulated angiogenic and osteogenic growth factors, including endothelial nitric oxide synthase, vascular endothelial growth factor, and proliferating cell nuclear antigen, thereby improving blood flow perfusion and promoting tissue regeneration. This suggests that ESWT can enhance flap survival and promote diabetic wound healing by increasing angiogenesis and local blood perfusion. Some studies have indicated that ESWT allows mechanical transduction, producing therapeutic benefits for angiogenesis and tissue regeneration in chronic diabetic and non-diabetic foot ulcers through complex biological pathways, but its mechanisms still require further in-depth exploration[12].
3
Smart Diabetic Foot Aids
Smart aids with active monitoring functions are the development trend of conservative treatment methods for diabetic foot in the future. Designing personalized smart monitoring shoes that combine the plantar pressure levels and physiological indicator characteristics of diabetic patients can help prevent the occurrence and deterioration of diabetic foot ulcers. At the same time, when monitoring the foot condition of patients, combining active protective measures can enhance the ability of foot tissues to respond to external mechanical stimuli.
Real-time monitoring of plantar pressure in diabetic patients, with a monitoring system providing immediate feedback on abnormal plantar pressures and accumulated loads, can promptly alert diabetic patients to areas of abnormal stress concentration and excessive accumulated loads, which is particularly important for patients with loss of protective sensation. Due to the relatively mature development of pressure sensor measurement technologies, most current smart diabetic foot aids are equipped with real-time monitoring functions for plantar pressure, providing early warnings of the risk of diabetic foot ulcer occurrence from a biomechanical perspective. Perrier et al.[13] designed a smart sock that can prevent diabetic foot ulcers; this system utilizes digital computational models to deduce pressure indicators from the cumulative pressure exerted during gait and pressure peaks near bony prominences (Figure 4A). Atlas et al.[14] also designed a real-time monitoring device for internal stress in foot tissues for diabetic patients. This device is portable and capable of real-time monitoring, calculating the internal stress levels in specific areas based on the plantar load pressure, and can alert diabetic patients to reduce foot load when stress is excessive (Figure 4B). Pu et al.[15] designed a pressure monitoring insole system that uses data from five pressure sensors to accurately calculate the forces exerted on the plantar surface during daily activities, providing a basis for wearable measurement system designs. Meanwhile, Pu et al.[16] achieved real-time monitoring of foot loading conditions in diabetic patients by analyzing the timing and force characteristics of gait under different daily activity patterns, identifying different movements through plantar pressure waveforms (Figure 4C). The smart shoes developed by Canadian company Orpyx issue timely alerts when abnormal plantar pressures are detected in diabetic patients, potentially reducing the incidence of diabetic foot ulcers (Figure 4D)[17].
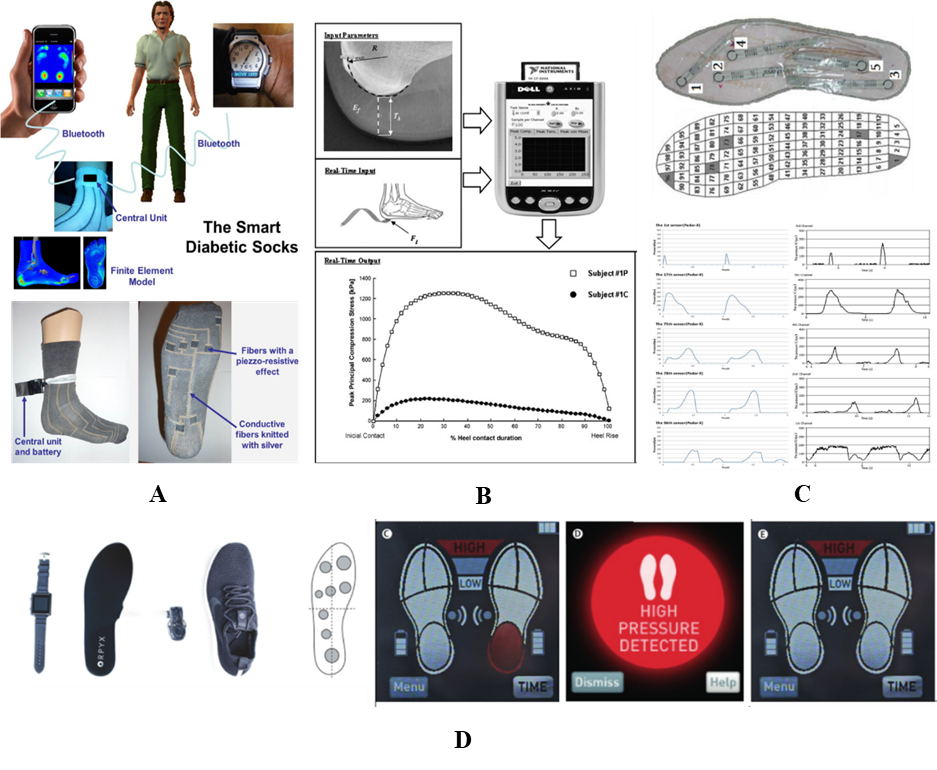
Figure 4: A: Smart socks (Perrier et al. 2014); B: Foot pressure monitoring operation diagram (Atlas et al. 2009); C: Gait motion recognition based on plantar pressure (Pu et al. 2014); D: SurroSense Rx smart insole system (Orpyx Medical Technologies, Calgary, AB, Canada; Abbott et al. 2019)
The development of smart insoles and shoes is closely related to the development of sensors within the shoes. In recent years, monitoring indicators for diabetic feet have gradually shifted from a single measurement of plantar pressure or foot temperature to monitoring multiple physiological indicators of the skin. For example, James developed a multi-variable scalable sensor platform that can utilize low-cost Raspberry Pi and Arduino devices to collect real-time data on acceleration, rotation, skin electrical response, environmental temperature, humidity, force, skin temperature, and bioimpedance signals[18]. Pascali et al.[19] proposed a smart multi-sensor hardware and software monitoring platform for diabetic patients that can simultaneously monitor glucose levels based on temperature, pressure, and sweat, and assessed the effectiveness of a temperature sensor array in detecting early signs of subcutaneous inflammation or ischemic damage through finite element simulations on a 3D model of the insole-foot component.
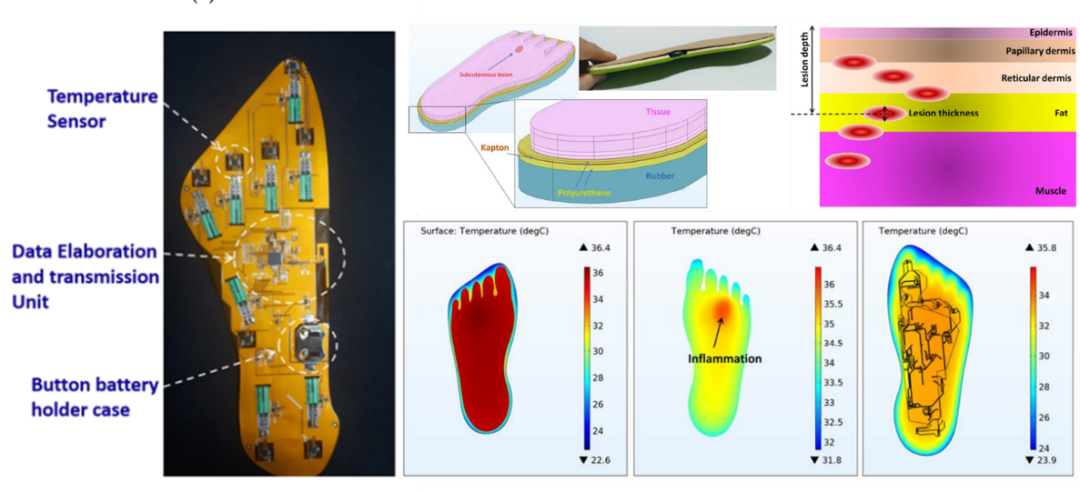
Figure 5: Smart multi-sensor hardware and software monitoring platform and finite element evaluation of skin inflammation damage (Pascali et al. 2021)
In addition to the risk warnings for foot ulcers, smart diabetic foot aids with active protective functions will be an important development direction in the future. Complications of diabetes also include peripheral vascular disease and diabetic peripheral neuropathy, which are significant influencing factors for the occurrence and development of foot ulcers. Smart foot aids that combine various active protective technologies are significant for improving ischemia in diabetic feet and enhancing sensory nerve functions. The School of Biological and Medical Engineering at Beihang University has independently developed the first smart protective shoe that integrates real-time monitoring of foot physiological indicators and both active and passive protective functions. This smart shoe integrates real-time monitoring insoles for foot temperature-pressure, pneumatic compression protection, vibration protection, and heating protection, enabling personalized monitoring and protection of foot health for diabetic patients in daily life (Figure 6).

Figure 6: Smart shoe for real-time monitoring and active protection of diabetic feet (School of Biological and Medical Engineering, Beihang University)
Research Outlook
Abnormal plantar pressure and soft tissue ischemia are significant factors leading to the occurrence and deterioration of diabetic foot ulcers. Pressure offloading insoles and shoes are commonly used conservative treatment methods for diabetic foot patients and have been proven to effectively shorten the healing time of foot ulcers and extend the recurrence cycle of ulcers. Currently, the design and manufacturing methods of diabetic foot pressure offloading insoles and shoes are gradually digitizing, but there is still much room for improvement in functionality and manufacturing processes. Intelligent real-time monitoring and protection are the future development trends of foot aids. By combining the characteristics of plantar pressure distribution and physiological indicators of diabetic patients, it is possible to better assess the health status of foot tissues and accurately predict the risk of foot ulcers in a timely manner. Additionally, based on the results of ulcer assessments and combined with external active protective measures, it will help to timely prevent and control the development and deterioration of foot ulcers.
References
[1] Armstrong D G, Boulton A J M, Bus S A. Diabetic foot ulcers and their recurrence[J]. New England Journal of Medicine, 2017, 376(24): 2367-2375.
[2] Owings T M, Apelqvist J, Stenström A, et al. Plantar pressures in diabetic patients with foot ulcers which have remained healed[J]. Diabetic Medicine, 2009, 26(11): 1141-1146.
[3] Lavery L A, Armstrong D G, Wunderlich R P, et al. Predictive Value of Foot Pressure Assessment as Part of a Population-Based Diabetes Disease Management Program[J]. Diabetes Care, 2003, 26(4):1069-1073.
[4] Pu F, Ren W, Fu H, et al. Plantar blood flow response to accumulated pressure stimulus in diabetic people with different peak plantar pressure: a non-randomized clinical trial[J]. Medical & biological engineering & computing, 2018, 56(7): 1127-1134.
[5] Bus S A. Innovations in plantar pressure and foot temperature measurements in diabetes[J]. Diabetes Metab Res Rev 2016; 32(Suppl. 1): 221–226.
[6] Schaper N C, Netten J, Apelqvist J, et al. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update)[J]. Diabetes/Metabolism Research and Reviews, 2020, 36(S1).
[7] Weiyan Ren, Yijie Duan, Yih-Kuen Jan, et al. Effect of Exercise Volume on Plantar Microcirculation and Tissue Stiffness in People with Type 2 Diabetes [J] Frontiers in Bioengineering and Biotechnology, 2021: 732628(1-10).
[8] Weiyan Ren, Fang Pu, Huiqin Luan, et al. Effects of Local Vibration with Different Intermittent Durations on Skin Blood Flow Responses in Diabetic People[J] Frontiers in Bioengineering and Biotechnology, 2019, 7:310.
[9] Weiyan Ren, Yijie Duan, Yih-Kuen Jan, et al. Effect of intermittent pneumatic compression with different inflation pressures on the distal microvascular responses of the foot in people with type 2 diabetes mellitus [J]. International Wound Journal, 2021: 1-10.
[10] Weiyan Ren, Liqiang Xu, Xuan Zheng, et al. Effect of different thermal stimuli on improving microcirculation in the contralateral foot, BioMedical Engineering OnLine, 2021, 20(14): 1-10.
[11] Jin D M, Yun X, Geng D F, et al. Effect of transcutaneous electrical nerve stimulation on symptomatic diabetic peripheral neuropathy: A meta-analysis of randomized controlled trials[J]. Diabetes Res Clin Pract, 2010, 89(1):10-15.
[12] Yang J-P, Lee Y-N, Son JW, and Han S-K. The Impact of Extracorporeal Shock Wave Therapy on Microcirculation in Diabetic Feet: A Pilot Study. Adv Skin Wound Care. 2019; 3212: 563-567.
[13] Perrier A, Vuillerme N, Luboz V, et al., Smart Diabetic Socks: Embedded device for diabetic foot prevention[J]. Irbm, 2014. 35(2): 72-76.
[14] Atlas E, Yizhar Z, Khamis S, et al., Utilization of the foot load monitor for evaluating deep plantar tissue stresses in patients with diabetes: Proof-of-concept studies[J]. Gait & Posture, 2009. 29(3): 377-382.
[15] Pu F, Yang Y, Fan X, et al., Optimal estimation of total plantar force for monitoring gait in daily life activities with low-price insole system[J]. Journal of Mechanics in Medicine & Biology, 2014. 14(03): 1450037.
[16] Pu F, Fan X, Yang Y, et al., Feedback system based on plantar pressure for monitoring toe-walking strides in children with cerebral palsy[J]. American Journal of Physical Medicine & Rehabilitation, 2014. 93(2): 122-129.
[17] Abbott C A, Chatwin K E, Foden P, et al. Innovative intelligent insole system reduces diabetic foot ulcer recurrence at plantar sites: a prospective, randomised, proof-of-concept study[J]. The Lancet Digital Health, 2019, 1(6): e308-e318.
[18] James C, Andrew C, Geraldine C. Wearable Multimodal Skin Sensing for the Diabetic Foot[J]. Electronics, 2016, 5(3):45.
[19] Pascali C D, Francioso L, Giampetruzzi L, et al. Modeling, Fabrication and Integration of Wearable Smart Sensors in a Monitoring Platform for Diabetic Patients[J]. Sensors, 2021, 21(5):1847.
★
END
★
Authors | Ren Weiyan, Duan Yijie, Liu Wei
(Beihang University)
We warmly welcome experts and scholars to contribute!
Submission email:[email protected]