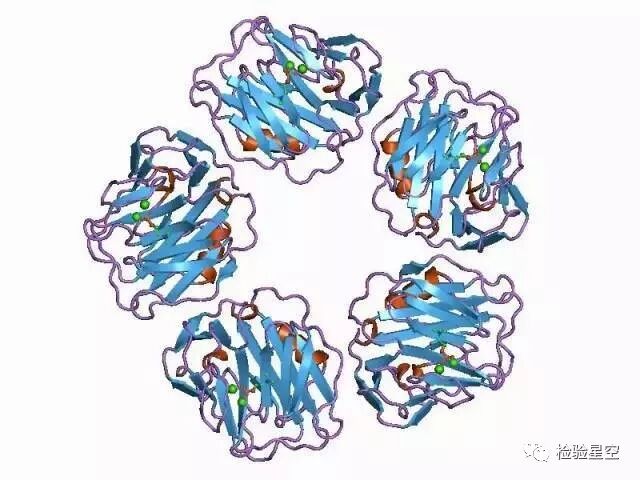
What does C-Reactive Protein look like?
C-Reactive Protein (CRP) is a symmetrical, cyclic pentamer, with a half-life of only 5-7 hours in the metabolic cycle.
▼
The synthesis of C-Reactive Protein in the body
C-Reactive Protein is synthesized in the liver and epithelial cells stimulated by inflammatory lymphokines (interleukin-6, interleukin-1, tumor necrosis factor TNF).
What is the role of C-Reactive Protein?
CRP has been widely used as an indicator of infection and inflammation. When we go to the hospital with a cold or fever, in addition to a complete blood count, many doctors prefer to look at the CRP level, mainly to differentiate between viral and bacterial infections.
1 C-Reactive Protein and Erythrocyte Sedimentation Rate (ESR)
Before the discovery of CRP, ESR was a commonly used non-specific inflammatory indicator and is still often used as an indicator for chronic infections or malignancies in various organs.
CRP testing can and will replace ESR in many diagnostic fields because C-Reactive Protein can reflect changes in inflammation more quickly and is a standardized immunoturbidimetric assay, providing reliable results.
ESR is a complex phenomenon influenced by various factors. It is related not only to the inflammatory state but also to red blood cell count, plasma osmotic pressure, red blood cell morphology, and hemoglobin content; the reference range for ESR varies with gender and age, and pregnancy and obesity also affect it. As an inflammatory indicator, CRP has incomparable advantages over ESR.
2
C-Reactive Protein and White Blood Cell Count (WBC)
In differentiating bacterial or viral infections, CRP is more accurate than WBC. WBC shows many inconsistencies when determining the efficacy of antibiotics against bacterial infections.
CRP is well-suited for detecting acute bacterial infections and determining antibiotic efficacy, especially in cases of neutropenia or during immunosuppressive therapy.
So, is C-Reactive Protein only applicable in this context?
C-Reactive Protein is one of the most important and sensitive markers of the acute phase response in the human body. Its clinical significance extends far beyond just acute infections.

C-Reactive Protein is much more powerful than you think!
1 The “Compass” for distinguishing bacterial and viral infections
CRP has been proven to be very useful in differentiating bacterial and viral infections. CRP levels increase during bacterial infections, while they do not increase during viral infections, and the degree of increase correlates with the severity of the bacterial infection. In cases of viral infections, CRP levels are normal or low, but adenoviruses and certain herpes viruses can cause significant tissue damage, leading to a mild increase in CRP.
C-Reactive Protein is one of the few diagnostic indicators that can reliably determine early in an infection whether it is bacterial or viral, to decide whether to initiate antibiotic treatment.
For many patients with viral infections, unnecessary antibiotic use can be avoided, as antibiotics are ineffective against viral infections and can lead to the potential danger of bacterial resistance.
2 A “Effective Means” to monitor antibiotic treatment
When a severe bacterial infection is suspected, the usual practice is to immediately start antibiotic treatment without considering whether CRP or other inflammatory indicators have not increased. The liver takes 6-12 hours to synthesize C-Reactive Protein, so it is not advisable to use CRP to detect the presence of bacterial infection in the first few hours after infection occurs.
For newborns suspected of sepsis, dynamic monitoring of C-Reactive Protein within 24-48 hours can serve as reliable evidence for whether to stop antibiotic treatment, while blood cultures require 48-72 hours of incubation time, and sepsis cannot be ruled out before the culture results are available.
Dynamic monitoring of C-Reactive Protein
When treating bacterial infections with antibiotics, dynamic monitoring of C-Reactive Protein is the most useful method. The amount of C-Reactive Protein in the blood increases with the rise of inflammatory factors, with a delay of several hours; the lymphokines secreted by active lymphocytes soon return to normal, but if treatment is ineffective, C-Reactive Protein can remain at high levels, and if the infection worsens, its concentration will also rise.
Dynamic monitoring of C-Reactive Protein provides earlier alerts for complications and assessments of treatment efficacy than clinical signs, and is more clinically significant in cases of neutropenia and immunosuppressive states.
Different clinical states of C-Reactive Protein
1 The “Weather Vane” for the severity of infection
Severe infections such as sepsis, endocarditis, osteomyelitis
Many diseases have a bacteremia stage, such as pneumonia, bacterial meningitis, typhoid fever, and purulent arthritis, where symptoms are almost identical to those of viral infections. When inflammatory symptoms are not obvious, a significantly elevated CRP (>100mg/L) indicates the presence of bacterial or fungal infection.
However, some patients may have only slightly elevated CRP during bacterial infections or may even remain below the threshold; this is especially true within 6-12 hours after infection occurs. Compared to ESR, CRP is more sensitive in diagnosing infectious meningitis, especially in the early stages of the disease (>12 hours), and drops back to normal faster than ESR after the pathogen is eliminated.
Significantly elevated CRP (>100mg/L) indicates the presence of severe bacterial infection.
Meningitis
It has been confirmed that testing CRP during meningitis is very useful, as it can distinguish between bacterial and viral meningitis, with a sensitivity of 96%, specificity of 93%, and a negative predictive value of 99% in children over 3 months old; no other laboratory indicators can reach this level.
Less than 20mg/L indicates viral meningitis.
2 A “Tool” to differentiate pneumonia and bronchitis
Pneumonia
Respiratory infections are challenging because many lower respiratory tract infections are mixed infections. Combining medical history and physical examination with CRP measurement helps in differential diagnosis.
For suspected pneumonia, CRP is considered the first-line screening method, with CRP greater than approximately 60mg/L indicating bacterial pneumonia.
Bronchitis
Acute bronchitis is rarely caused by bacterial infections and seldom leads to significant CRP elevation. Therefore, CRP measurement can help differentiate pneumonia from bronchitis. Testing CRP can reduce unnecessary antibiotic treatment for acute bronchitis and upper respiratory infections without specific indications. CRP is recommended as a diagnostic tool when distinguishing pneumonia from bronchitis in lower respiratory tract infections.
3 Indicating the severity of acute pancreatitis
CRP is used to assess the severity of acute pancreatitis. When CRP exceeds 250mg/L, it indicates extensive necrotizing pancreatitis.
4 Accurate diagnosis and treatment of maxillary sinusitis and pharyngitis
Maxillary sinusitis
Haemophilus influenzae is the most common cause of acute maxillary sinusitis, with CRP around 20mg/L; higher CRP concentrations (>40mg/L) suggest possible infections by purulent streptococci or pneumococci, which, if not treated promptly, may develop into an abscess.
Elevated CRP can serve as a good standard for using antibiotics, much better than simple clinical examination.
Bacterial pharyngitis
Measuring CRP can improve the diagnostic accuracy of throat infections, significantly increasing the accuracy of diagnosis compared to simple clinical examination, leading to appropriate treatment. Unnecessary or excessive use of antibiotics can lead to an increase in resistant strains; measuring CRP can reduce this occurrence. The CRP threshold for differentiating between bacterial and non-bacterial pharyngitis is approximately 35mg/L.
5 Indicators for differentiating urinary tract infections
CRP is a reliable laboratory indicator for distinguishing between general lower urinary tract infections (cystitis) and more severe upper urinary tract infections (pyelonephritis).
CRP greater than approximately 100-140mg/L indicates pyelonephritis.
6 Also predicts the risk of cardiovascular disease
Studies have found that high-sensitivity CRP levels are an important risk factor for cardiovascular morbidity and mortality.
High-sensitivity CRP is clinically used mainly to assess cardiovascular risk. Explaining this in a single sentence may seem inadequate. Let’s approach it from another angle: when a patient has minor cardiovascular lesions, but clinically has not yet developed cardiovascular disease, myocardial cells are damaged (this damage is subtle and unnoticed), leading to a slight increase in high-sensitivity CRP levels.

Post-surgical infection and trauma
Tissue damage
During extensive burns, CRP significantly increases; if there is no infection, it will decrease after three days and continue to decline during the healing period of over a month. If an infection occurs during this period, CRP will rise again, so CRP can be used to monitor the entire course of the disease.
Elevated CRP can alert to sepsis in burn patients for timely treatment.
Surgery
CRP increases within 6 hours post-surgery; if there are no complications, it should decrease to normal within two to three days. If an infection occurs post-surgery, CRP will not decrease for a long time.
Patients with elevated preoperative CRP have a significantly higher incidence of postoperative infections and longer hospital stays than those with normal preoperative CRP.
Appendicitis
The diagnosis of acute appendicitis is often based on the physician’s examination of clinical symptoms, with a misdiagnosis rate of about 15%-25%.
Patients with perforated appendicitis often have CRP exceeding 100mg/L, while non-perforated cases show only mild elevation, above 20mg/L. If both WBC and CRP are normal, the likelihood of acute appendicitis is low.
Using CRP as an auxiliary diagnostic indicator for acute appendicitis helps reduce unnecessary surgeries. In cases where the diagnosis is uncertain, clinical examination and CRP measurement are appropriate, and CRP is recommended as a routine test for suspected appendicitis.
CRP >100mg/L suggests possible perforation.
Significance of bedside CRP testing (POCT)
Rapid diagnosis
When ill, early treatment is crucial.
CRP is valuable for both diagnosis and treatment, and the speed of measurement is very important for doctors, which has driven technological advancements. Nowadays, CRP testing can be performed not only in clinical laboratories but also at primary healthcare points, becoming one of the bedside testing items, with results available within 5 minutes.
Children
Young children are prone to respiratory infections and often visit small clinics or primary hospitals for initial diagnosis; rapid CRP testing can help differentiate between viral and bacterial infections, reducing unnecessary antibiotic treatment.
Only a small sample is needed (just 5 microliters), and it can be tested using capillary blood, making it very convenient (serum or plasma can also be used).
Older adults
Older adults may have severe infections without fever or elevated WBC counts; measuring CRP can help detect bacterial infections.
Guiding appropriate antibiotic use
With the continuous increase of resistant strains, it has become even more important to perform CRP testing on all suspected bacterial infections to appropriately avoid antibiotic misuse, as antibiotics are ineffective against viral infections.
Treatment
Because CRP testing is easy to perform and provides rapid reports, patients can receive appropriate treatment plans at the first visit, with targeted medication leading to early recovery.

● Characteristics and clinical significance of blood routine histogram● What drugs affect clinical test results?● Summary of reasons for unqualified clinical test specimens● Prevention and authoritative elimination of PCR laboratory contamination● Management methods for large-scale COVID-19 nucleic acid testing laboratories (trial)● COVID-19 nucleic acid testing work manual for medical institutions (trial second edition)● Detailed process for handling occupational exposure of medical staff (HBV, HCV, TP, HIV)
If you find this useful, please click “Read“! Click the original text for more valuable content!
Click the original text for more valuable content!