
Surgical robots are integrated operating systems that combine clinical medicine, mechanics, biomechanics, and computer science. Thanks to the development of mechanical control, visual imaging, optoelectronic technology, and artificial intelligence, the application of surgical robots in the medical field has driven surgery towards more intelligent, precise, and minimally invasive directions. While improving surgical outcomes and enhancing the working environment for doctors, surgical robot technology can further reduce patient trauma, achieving safer, more reliable, and highly reproducible surgical treatments.
Despite being called “robots,” surgical robots are still a long way from truly replacing doctors and independently performing surgeries. Currently, they remain in a semi-automatic phase that assists doctors in completing surgeries. Surgical robots, which vary in form based on different pathologies, only replace or enhance the doctor’s hand movements, with operational decisions still requiring the doctor’s judgment. Therefore, after decades of development experience, exploring surgical robots that aim to improve patient benefits while integrating more advanced intelligent technologies presents significant challenges and importance.
The Origin and Development of Surgical Robots
Minimally invasive surgeries help reduce the pain caused by large incisions and speed up postoperative recovery, which is a significant reason for the emergence of surgical robots. At the same time, the precise positioning and movements of robots make them play an essential role in surgical scenarios requiring fine operations. They have already been applied in various fields, including general surgery, neurosurgery, urology, orthopedics, and gynecology. Based on the type of organ targeted in surgery, surgical robots can be categorized into hard tissue robots and soft tissue robots. For hard tissues, they mainly include neurosurgery and orthopedic surgical robots; for soft tissues, they can be divided into laparoscopic surgical robots, natural orifice transluminal endoscopic surgical robots, vascular interventional surgical robots, and percutaneous puncture surgical robots.

Figure 1 Classification of Surgical Robots
In the early stages of surgical robot development, the focus was mainly on exploring the application of industrial robots to surgical robots, with neurosurgery and orthopedics as the primary surgical scenarios, utilizing the high positioning accuracy of industrial robots to perform simple surgical operations.
In 1985, Yik San Kwoh and others used the PUMA 200 industrial robot to complete a neurosurgical brain operation, marking the first application of robotic technology in surgical scenarios and opening the door to the development of surgical robots.
In 1988, the Probot system completed the first prostate surgery assisted by a surgical robot.
In 1992, the Robodoc system designed by Integrated Surgical Systems completed a total hip replacement and became the first to receive FDA certification.
In neurosurgery, surgical robots have achieved a significant transition from traditional craniotomy to minimally invasive surgery. Positioning is a key issue in surgery; traditional neurosurgery uses stereotactic surgical tools that require the patient to wear a head frame while awake, which is very painful, and the surgery is time-consuming with blind spots in the field of view. Surgical robots utilize robotic arms for precise positioning, applicable in treatments for epilepsy, Parkinson’s disease, brain tumors, and intracerebral hemorrhage.
Traditional orthopedic surgeries, such as joint replacement, spinal surgery, and orthopedic trauma surgery, face clinical pain points like poor precision, high osteotomy errors, and high rates of improper screw placement. The use of surgical robots can improve surgical accuracy and stability, reduce damage to nerves and blood vessels, and avoid severe complications such as paralysis.
With the realization of microsurgery and laparoscopic surgery, the development of surgical robots has entered a breakthrough stage, achieving more flexible and precise movements and higher surgical accuracy in response to clinical demands, while remote operation significantly reduces physician fatigue. The main difference between microsurgery and early neurosurgery is that the former no longer stimulates nerves through electrode implantation but performs direct operations on the nerves for treatment. Surgical methods have gradually evolved from open surgery to laparoscopic surgery to natural orifice surgery, moving towards minimally invasive approaches.
In 1993, the Aesop robot developed by the American Computer Motion Company completed the first laparoscopic surgery, and the Zeus system developed on this basis utilized master-slave teleoperation technology.
In 1997, the da Vinci surgical system developed by Intuitive Surgical completed its first human trial and received FDA approval in 2000, significantly improving the precision and flexibility of surgical operations while ensuring minimal patient trauma, garnering widespread attention for the application of robotic technology in surgical scenarios.
To address clinical pain points such as limited instrument movement, the “seesaw effect” of instruments passing through body incisions, poor surgical fields, and physician fatigue in laparoscopic surgery, the da Vinci surgical robot increases intraluminal flexibility through implanted wrist joints, utilizes remote master-slave motion for intuitive operations, and forms an intuitive hand-eye coordination loop through high-definition stereoscopic imaging.
The commercial success of the da Vinci surgical robot has propelled the surgical robot industry into a phase of diversified development, achieving further advancements in joint surgery, spinal surgery, single-port laparoscopic surgery, multi-port laparoscopic surgery, vascular interventional surgery, and neurosurgery.
Technical Analysis of Typical Surgical Robots
Neurosurgery Surgical Robots
In 1985, the team led by Yik San Kwoh at Long Beach Memorial Medical Center used the PUMA 200 industrial robot for stereotactic brain biopsy, guiding the biopsy needle using the industrial robot’s high repeatability and accuracy. However, due to the difficulty in aligning the patient’s head with the robot’s base, the overall accuracy of the surgical system remained low.
In 1991, the Minerva system was one of the first to provide real-time image guidance, automatically performing skin incisions, skull drilling, and instrument operations while utilizing intraoperative CT scans to overcome brain tissue displacement issues. Although this system improved precision, concerns about radiation and operational safety led to its discontinuation.
In 1997, the NeuroMate became the first FDA-approved surgical robot for clinical neurosurgery, featuring a five-degree-of-freedom design that allowed for both frame-based and frameless positioning during surgery.
Based on their operational methods, neurosurgery surgical robots can be categorized into positioning and operational types. Positioning surgical robots include the UK’s NeuroMate, the US’s Pathfinder, and the ROSA ONE Brain.
Operational surgical robots require fine adjustments to the nerves, placing higher demands on the robotic systems than positioning types. Currently, many positioning surgical robots have been industrialized, but most operational robots remain in laboratory stages, potentially needing to overcome issues related to precise operation in MRI environments, including driving, sensing, control, and sterilization challenges. The NeuroArm was the first neurosurgery surgical robot system capable of intracranial operations without interference from magnetic resonance imaging.
Perception and positioning are key technologies for neurosurgery surgical robots, including the perception and positioning of lesions, local areas, and overall environments. The perception and positioning of lesions are achieved through multi-modal three-dimensional visualization imaging processing technologies, including computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), and diffusion tensor imaging (DTI), often used for safer and more effective surgical planning before surgery.
Local perception and positioning are achieved through registration for lesion localization during surgery, which can be done through implantation, adhesive markers, or 3D structured light/surface reconstruction methods. Global perception of the surgical environment is based on intelligent obstacle avoidance and posture compensation technologies, laying the foundation for future automated surgeries.
Orthopedic Surgical Robots
Before the 19th century, orthopedic surgery relied heavily on the experience of physicians. In the mid-20th century, with the development of imaging technology, image-guided surgery allowed for more precise orthopedic operations. By the 21st century, the application of robotics in surgery has ushered orthopedic surgery into the era of robotic intelligent assistance.
The earliest orthopedic surgical robots that achieved technological and commercial application can be classified into passive, semi-active, and active types. Active robots autonomously complete the surgical process, including the robotic doctor from the US in 1986 and the Caspar robot from Germany in 1997. Although these surgical robots appeared early, issues such as safety, surgical efficiency, and preparation time hindered their promotion and application.
As a result, current orthopedic surgeries primarily utilize semi-active and passive robots. Semi-active robots are operated jointly by the physician and the robot, while passive robots do not perform surgical operations on their own, with the physician retaining complete control.
In 1992, Imperial College London developed the first semi-active orthopedic robot, introducing the concept of “haptic perception” and mapping preoperative planning information to the surgical operation area, allowing the robot to provide operational constraints while the physician performs bone shaping operations through dragging.
In a typical orthopedic surgical robot system, the navigation and positioning system employs optical positioning, intraoperative CT, and magnetic navigation for economical and practical registration positioning; the surgical planning system realizes intelligent modeling and planning; and the robotic arm execution system operates through high-performance hardware and motion control that meets clinical needs.
In spinal surgery, current surgical robots primarily target clinical procedures such as pedicle screw fixation, employing medical imaging planning to achieve spatially precise positioning, with robotic arms autonomously completing or guiding physicians in drilling procedures for implantation channels. For trauma orthopedic surgeries, early research mainly applied to long bone fracture reduction surgeries, but due to the diversity of fracture surgery types, trauma orthopedic robots have not yet achieved widespread clinical application or product promotion.
Vascular Interventional Surgical Robots
Vascular interventional surgery involves navigating catheters, guidewires, and other interventional instruments through the patient’s blood vessels under the guidance of medical imaging, following planned paths to precisely reach lesions for treatment.
In traditional vascular interventional surgery, physicians complete the construction of vascular stents, thrombolysis, and drug placement by delivering and rotating guidewires and catheters under fluoroscopic imaging. However, prolonged exposure to radiation poses serious health threats to physicians, while heavy lead protective aprons, hand fatigue, and tremors significantly impact operational precision. Therefore, vascular interventional surgical robots assist physicians in remotely controlling catheters and guidewires, avoiding X-ray exposure and achieving higher operational precision and more stable surgical outcomes.
Early vascular interventional surgical robots were based on magnetic navigation systems.
In 2004, Stereotaxis, Inc. designed the first-generation magnetic navigation system, Telstar, but the system required special guidewires and catheters, making it incapable of performing balloon and stent operations, with limited operational distance and force.
In 2006, the RNS vascular interventional surgical robot system from Israel adopted an electromechanical system, effectively improving interventional surgical precision by designing guidewire navigators to push and rotate guidewires.
Building on the RNS, in 2012, Corindus developed the CorPath 200 robotic system, which was further improved to create the more precise CorPath GRX vascular interventional surgical robot. The Sensi X1 system developed by Hansen Medical adopted a flexible active catheter, while the Sensi X2 system added force feedback at the catheter tip.
Vascular interventional surgical robots can be categorized based on surgical sites into coronary interventions, neuro interventions, and peripheral interventions. The development of general vascular interventional surgical robots allows for the simultaneous execution of multiple surgical procedures, eliminating the need to change catheters and guidewires during surgery, thus reducing hospital procurement costs.
Key technologies in vascular interventional surgical robots include image navigation systems that assess the position of interventional instruments through vascular imaging; active drive catheters that adapt to different vessels and surgical steps; robotic arm structures with high compliance and flexibility for precise and rapid catheter operations; and force feedback systems that relay vascular contact forces to the operator, reducing the risk of vascular rupture.
Percutaneous Puncture Surgical Robots
In traditional percutaneous puncture surgeries, physicians use puncture needles or catheters under medical imaging guidance to directly reach the lesions through the patient’s skin for diagnosis or treatment. Both synchronous and asynchronous scanning and puncturing methods suffer from clinical pain points such as a lack of real-time accurate surgical area information perception, difficulty in hitting targets due to respiratory movements, and a high dependency on physician skills.
Key technologies in percutaneous puncture surgical robots include preoperative medical imaging that captures images of the lesion using CT, MRI, and other technologies. Path planning and navigation positioning systems are another key technology, which can be realized based on optical or electromagnetic systems.
During the puncturing process, appropriate deformation compensation is required to address soft tissue deformation, puncture needle bending, and changes in the puncture path due to applied forces. Additionally, it is necessary to overcome involuntary body movements during surgery; for instance, when puncturing the chest or abdomen, the target position may change with respiratory movements, and involuntary muscle contractions due to pain responses can also affect surface positioning.
Percutaneous biopsy surgical robots have been widely used in breast biopsies, lung biopsies, prostate biopsies, etc. When combined with ablation, percutaneous puncture surgical robots can also be used for tumor ablation.
Laparoscopic Surgical Robots
Laparoscopic surgical robots are currently the most commercially valuable type of surgical robots, with a wide range of applications, mainly in urology, gynecology, general surgery, and thoracic surgery. Taking the da Vinci system as an example, laparoscopic surgical robots typically consist of a physician control console, robotic arms, and imaging systems.
Laparoscopic surgical robots can be divided into multi-port laparoscopic surgical robots and single-port laparoscopic surgical robots. Multi-port robots utilize multiple incisions to complete surgical treatments, making operations convenient and providing a broad surgical field. Single-port robots use only a single incision, resulting in less trauma and faster recovery, offering advantages in performing surgeries in highly focused narrow spaces.
Currently, the multi-port robot market is entirely monopolized by the United States, while the da Vinci SP surgical system leads the single-port robot segment.
Multi-port laparoscopic surgical robots have relatively uniform configurations, consisting of external robotic arms and long rod-shaped surgical tools. The ends of the surgical tools enhance operational flexibility by incorporating wrist joints, with common mechanisms including pulley wire mechanisms, link-driven mechanisms, continuum mechanisms, and narrow-band deformation mechanisms, allowing for wrist joint movements. External robotic arms meet the constraints of remote centric motion, ensuring that straight rod surgical tools pass through a single incision on the patient’s body without pulling on the abdominal wall.
Mechanisms capable of achieving remote centric motion include parallelogram mechanisms, equivalent parallelogram mechanisms using synchronous belts, parallelogram and parallel mechanisms, spherical link mechanisms, pure parallel mechanisms, and spatial guide rail mechanisms. Robotic systems are generally equipped with 3D laparoscopes, and the use of motion sensing and force feedback systems can enhance operational accuracy.
Developing single-port laparoscopic surgical robots is more challenging, as the diameter of the laparoscope is a critical design factor. A single incision must accommodate one visual module and 2-3 surgical arms, with the visual module needing to integrate lighting functions, and the surgical arms requiring sufficient strength and working space.
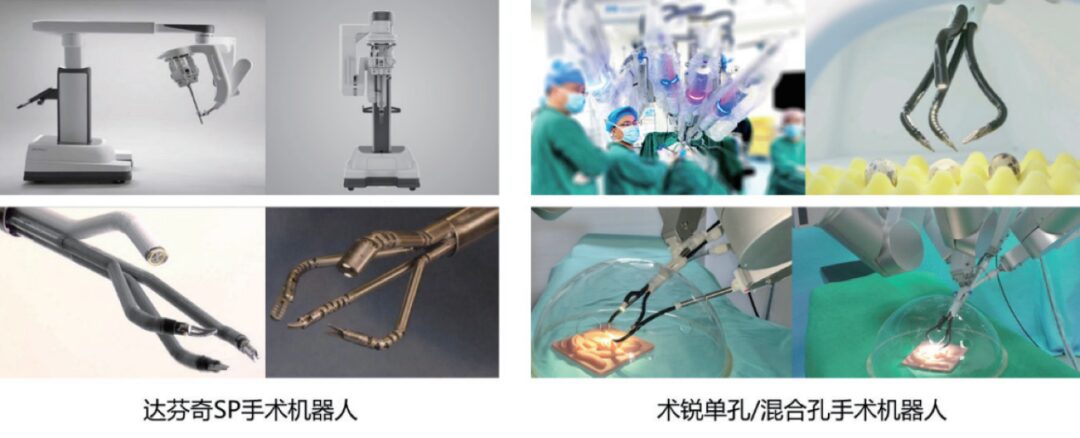
Figure 2 Examples of Domestic and International Laparoscopic Surgical Robots
Based on different driving forms, single-port laparoscopic surgical robots have various implementation methods. In wire-driven systems, the Vinci SP system, developed by Intuitive Surgical in 2014, used a 25mm diameter laparoscope. However, wire-driven multi-joint surgical tools face challenges in accommodating sufficient pulleys, with wires being prone to wear and breakage risks. Motor-embedded systems involve implanting micro-motors within surgical tools, but to avoid the impact of high-frequency high-voltage electricity on motor motion control, electromagnetic protection must be applied next to the motor, resulting in bulky surgical arms and high costs.
To replace wire-driven systems, Waseda University and the Daegu Gyeongbuk Institute of Science and Technology (DGIST) in South Korea have developed link-driven systems, but these systems lack sufficient operational flexibility. Continuum mechanism systems are based on dual continuum mechanisms, achieving surgical execution arm movements through overall deformation of the mechanism, resulting in flexible motion. Continuum mechanisms simultaneously serve structural and deformation transmission purposes, allowing for more compact designs. In 2014, Professor Xu Kai’s team at Shanghai Jiao Tong University developed a 12mm diameter laparoscope SURS system, achieving the world’s smallest skin incision.
Laparoscopic surgical robots have a vast and rapidly growing market. The da Vinci surgical system from Intuitive Surgical holds an absolute monopoly in the industry, while products such as Senhance from TransEnterix, Revo-i from Meere, and Hugo system from Medtronic have all been approved for market entry. In the single-port laparoscopic surgical robot sector, the world’s first single-port laparoscopic surgical robot IREP system was initiated in the US in 2007, with the da Vinci SP single-port system from Intuitive Surgical completing its development and finalization in 2015.
Among domestic companies, Beijing Shurui Technology Co., Ltd. has developed a single-port laparoscopic surgical robot based on continuum snake-arm technology, achieving precise cutting and suturing. In 2021, it completed the first pure single-port robot radical prostatectomy in Asia, resulting in fewer and smaller incisions compared to the da Vinci multi-port system while achieving similar surgical outcomes. Currently, Shurui Company is conducting clinical trials for single-port robot surgeries in general surgery, gynecology, and other fields with several clinical centers, holding significant implications for independent R&D and import substitution.
Natural Orifice Transluminal Endoscopic Surgery Robots
Natural Orifice Transluminal Endoscopic Surgery (NOTES) involves using natural orifices in the human body to enter the abdominal cavity, mediastinum, or thoracic cavity for exploration, biopsy, and various surgical operations, offering advantages such as less pain, no external scars, minimal trauma, and rapid recovery. However, NOTES robots face issues such as limited visibility and lack of tactile perception.
NOTES robots typically consist of one camera and two robotic arms, with key technologies including the diameter of the operational arms, end flexibility, and gripping force of the forceps.
In 1994, Wilk first proposed the idea of performing surgical treatments through natural orifices in the human body.
In 2007, Abbott and others from Purdue University developed the ViaCath system, which allows the endoscope and operational arms to reach inside the body through the gastrointestinal tract.
In 2015, the Flex robot developed by Medrobotics entered the oropharynx and hypopharynx through the mouth, becoming the first robot approved by the FDA for natural orifice surgery, though its application was limited due to restricted access.
Johnson & Johnson’s Monarch robot combines nCLE imaging for examining small abdominal nodules, using a 3.5mm ultra-thin catheter to reach small bronchi. The Anovo robot can perform benign surgical operations via the vagina under laparoscopic guidance through the umbilicus and received FDA approval in February 2021.
The Future and Outlook of Surgical Robots
“Eyes” Brighter With the development of surface reconstruction, fluorescence and multispectral imaging, confocal microscopy, and augmented reality technologies, surgical robots can provide clearer and more intuitive surgical views to assist doctors in performing surgeries better.
“Hands” More Precise By incorporating gripping force perception systems, operational force perception systems, and multi-perception human-machine interaction control technologies, surgeons can achieve more precise control when using surgical robots.
“Brains” Smarter Leveraging artificial intelligence technology to achieve surgical automation is the future development trend of surgical robots. In January 2022, robots independently completed laparoscopic small bowel anastomosis on soft tissues in pigs for the first time, pushing forward the further development of surgical automation. Surgical automation can be classified from “no automation” to “full automation” in levels 0-5, with most surgical robots still in the assistant stage, presenting significant challenges and vast development prospects.
“Bodies” Smaller Miniaturization is another trend in the development of surgical robots, with the advancement of capsule robots and micro-nano robots further promoting non-invasive surgeries.
The innovation of surgical methods, minimally invasive tools, and technologies has never ceased. In the future, smarter, more efficient, and precise surgical robots will greatly reduce patient suffering, further enhance surgical output, lower surgical risks, and contribute significantly to the pursuit of a better life for the people, providing stronger guarantees.
This article is based on the author’s report at the “Shanghai Science Popularization Forum” organized by the Shanghai Association for Science and Technology Volunteers.
Click to order “World Science” at a discount
