In the ongoing exploration of alternatives to organ transplantation in the medical field, on June 23, 2025, a research team led by Professor Alison Marsden at Stanford University announced findings that mark a new stage in3D bioprinting technology. This groundbreaking technology, through a dual approach of algorithmic revolution and material innovation, successfully constructs artificial vascular networks with complete physiological functions, increasing the survival rate of lab-cultured kidney cells to400 times that of the control group, clearing the most critical technical barrier for the eventual realization of transplantable artificial organs.
The biggest bottleneck faced by traditional3D printed organs is the inability to replicate the intricate vascular system of the human body. Research shows that cells cultured in vitro will die from hypoxia if they are more than200 micrometers away from a nutrient source, meaning that any practical artificial organ must establish a capillary-level delivery network.The topology optimization algorithm developed by Marsden’s team simulates Murray’s law, which describes the mathematical relationship between vascular diameter and branching angles, compressing a manual design process that would normally take weeks into just a few minutes. This biologically inspired computational model can automatically generate the most efficient vascular branching schemes in fluid mechanics, accurately arranging25 different levels of blood vessels within a kidney unit’s annular structure with a diameter of1 centimeter.
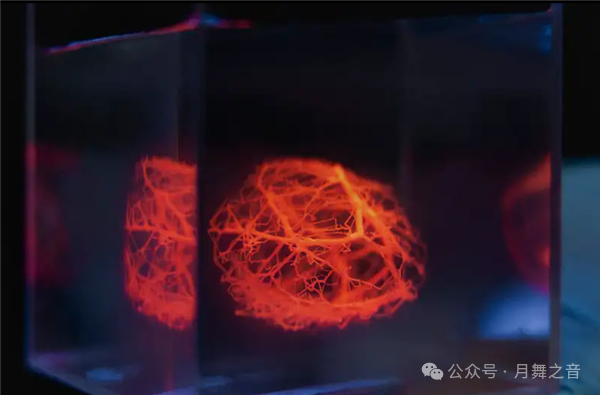
To achieve precise construction of sub-millimeter blood vessels, the research team innovatively used temperature-responsive gelatin microspheres as printing materials. This biocompatible material remains liquid at4°C and instantly solidifies upon contact with a37°C culture medium through micro-nozzle extrusion, forming hollow tubular structures with a diameter of only1 millimeter. Compared to traditional UV-cured hydrogels, this technology avoids UV damage to cells and enables continuous printing of complex vascular networks. Experimental data shows that this biomimetic vascular structure achieves82% oxygen transport efficiency under simulated physiological blood flow conditions, with nutrient permeability meeting the metabolic needs of over90% of cells.
The maturity of this technology is attributed to deep interdisciplinary integration. Computational biologists established a vascular growth model containing4000 parameters, materials scientists developed a new type of bioink with shape memory characteristics, and mechanical engineers designed a six-degree-of-freedom precision printing platform. Notably, the team introduced a“vascular-first” printing strategy: first constructing a complete vascular network framework, then injecting bioink containing stem cells. This reverse engineering approach successfully resolves the contradiction between cell encapsulation rates and vascular patency that traditional printing faces, achieving a live cell density of1.2 billion cells per cubic centimeter, close to the density of natural kidney cortical cells.
The research team disclosed a clear path to industrialization: by 2026, complete animal experiments on centimeter-scale functional organ modules (such as kidney units and liver lobules) will be completed; by 2028, multi-module organ assembly technology will be realized; and by 2030, full-size pig organ printing tests will commence. Currently, three multinational medical technology companies are involved in industrialization cooperation, focusing on vascular endothelialization technology and immune rejection control solutions. An independent evaluation report from Saclay University in Paris indicates that if this technology is successfully transformed, it could reduce the global organ transplant waiting list by60%, potentially saving the lives of about2 million end-stage organ failure patients each year.
This breakthrough also raises a series of social issues. Bioethicists are discussing the legal status of“printed organs”— when organs can be industrially produced, the existing legal framework surrounding human organ transplantation needs a comprehensive overhaul. The FDA in the United States has initiated a special approval channel for“biomanufactured organs,” but experts estimate that full process certification will still take5-7 years. Additionally, the cost of this technology is approximately$500 per cubic centimeter, making it a high-end medical solution in the short term, and how to achieve technological accessibility will be an important issue for the next decade.
This research not only opens a new avenue for organ regeneration medicine, but its core algorithm can also be extended to applications in drug screening models, trauma repair scaffolds, and other fields. As noted in a review by Nature Biotechnology, when scientists successfully translate mathematical laws into life support systems, humanity will have truly mastered the engineering code for“creating life.” With the advancement of the pig body experiment plan, the medical dream of printing replacement organs using patients’ own cells is accelerating towards reality.
Please open in the WeChat client