“As people age, the fear of falling becomes paramount; a fall could mean never getting up again.” This sentiment resonates deeply with 70-year-old Ms. Li (a pseudonym) from Lishui Jinyun. Last spring, she suffered a fall at home due to osteoporosis and was diagnosed with a “geriatric femoral neck fracture” at a local hospital.
The doctors at the local hospital performed a hip joint replacement surgery, but unfortunately, the prosthesis became infected post-operation. Bacteria formed a “protective shield” biofilm on the surface of the prosthesis, rendering ordinary antibiotics ineffective. This caused Ms. Li immense suffering, as she experienced persistent pain in her joint and a continuous low-grade fever, leaving her feeling lethargic every day.
According to treatment protocols, a “spacer surgery” was necessary: removing the infected prosthesis and implanting an antibiotic-laden bone cement spacer, waiting for the infection to be controlled before a second “revision” surgery. However, Ms. Li had a renal stoma and chronic urinary tract inflammation, with inflammatory markers remaining elevated. This dragged on for a whole year, during which she went from being able to use a walker to being bedridden. Her family was distraught, fearing that “if this continues, her bones will deteriorate completely!”
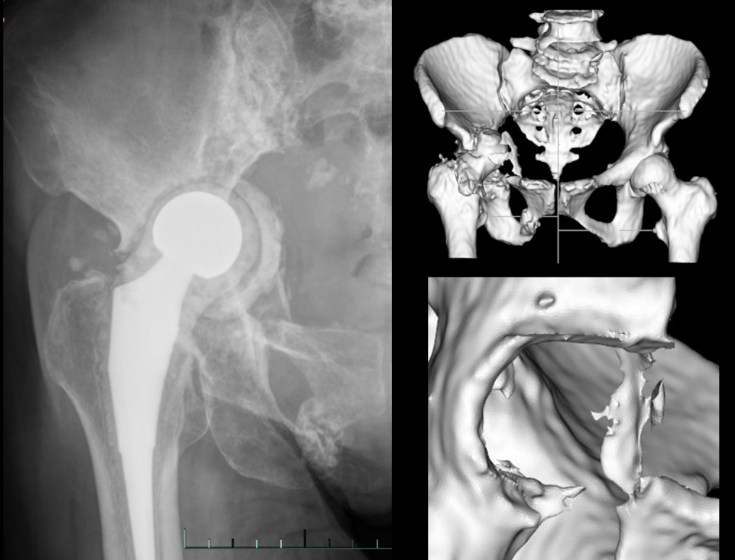
Imaging one year post-spacer surgery of the right hip joint
Double Challenges of Traditional Orthopedic Revision:
Why is it so difficult to repair fractures in the elderly?
Upon hearing that orthopedic experts from the First Affiliated Hospital of Zhejiang University School of Medicine frequently visit Jinyun County People’s Hospital, Ms. Li’s family decided to go there.
At the orthopedic outpatient clinic, Professor Xie Jie, the deputy director of orthopedics at Zhejiang University, carefully reviewed her medical history and patiently explained that traditional surgeries cannot overcome two major challenges during treatment:
1

Prosthesis and Bone Compatibility Issues
Traditional custom prostheses are designed based on the “fit” principle, similar to buying shoes in a specific size. However, Ms. Li’s acetabulum had over 50% bone loss, and the hardened bone was like “unyielding stone.” During manual grinding, if the prosthesis was too light, it wouldn’t adhere properly; if too heavy, the bone could “collapse.” The fit could only reach a maximum of 80%, posing a high risk of loosening in the long term.
2

Obscured Surgical Field
To minimize infection, revisions require minimal soft tissue dissection. Surgeons must manually install the prosthesis in a “narrow alley” surgical field, relying solely on experience to control angles. A deviation of more than 5° in the anteversion angle could lead to postoperative dislocation. Ms. Li’s muscle atrophy increased the stability requirements, significantly raising the risk of dislocation in traditional surgeries.
“For the elderly, delaying surgery by even one hour increases blood loss and the risks of postoperative anemia, infection, and cardiovascular events during the perioperative period. If they cannot get off the operating table, it could be disastrous,” Professor Xie pointed out. Traditional revisions take 3-4 hours, with blood loss exceeding 500ml, which patients like Ms. Li cannot endure in a “prolonged battle.”
So, would Ms. Li have to continue waiting in bed forever?
“Perhaps we can try a robotic navigation-assisted 3D printed custom acetabular prosthesis revision surgery,” Professor Xie’s words ignited hope in Ms. Li.
How Zhejiang University Hospital Revitalizes Fractured Joints
By Installing an “Intelligent Puzzle System”
Professor Xie introduced that the domestic robotic navigation-assisted 3D printed custom acetabular prosthesis revision surgery effectively addresses the two core challenges present in traditional hip joint revision surgeries. It not only improves the accuracy of prosthesis installation but also significantly shortens the surgical time, providing better outcomes and lower complication risks for patients.
To ensure a smooth treatment, the orthopedic team at Zhejiang University Hospital meticulously customized a surgical plan for Ms. Li.
Preoperatively, they created a “precise map” for the bone: using CT scans to generate a 3D model of the hip, the robotic system simulated the optimal grinding path. It clearly marked which hardened bone should be ground and which healthy bone should be preserved, just like planning a “navigation route” in advance.
1
2
During the operation, they performed sub-millimeter level “bone sculpting”: A “robotic arm” navigation device tracked the grinding head in real-time, with an error of only 0.1 millimeters. When facing hardened bone, the grinding head no longer “brutally smashed” but instead “carved” layer by layer, removing the “stubborn layer” while preserving as much bone mass as possible—this was crucial for Ms. Li, who had osteoporosis.
Personalized adaptation: Traditional prostheses are produced “according to the design,” but Ms. Li’s prosthesis was like a “bone twin.” The 3D printed prosthesis perfectly adapted to the bone defect based on preoperative CT data, with a fit rate soaring from the traditional 70%-80% to 95%.
3

Fine bone grinding under robotic navigation
The surgery was highly successful; on the first day post-operation, Ms. Li was already able to walk with the aid of a walker. This was also the world’s first hip joint prosthesis revision surgery utilizing both robotic navigation and 3D printing technology, providing new insights for the treatment of complex hip joint diseases in the future.

On the first day post-operation, Ms. Li walked with the aid of a walker
The shortened surgical time and precise operation spared Ms. Li much suffering, significantly reducing the risk of prosthesis loosening. Now, Ms. Li can walk independently without a walker, fully managing her daily life and often going out to buy groceries. She always says, “My dislocated joint was pieced back together by Zhejiang University Hospital using robots and 3D printing!”

Post-operative imaging
 Ms. Li presenting a banner to Professor Xie (first from the left) and the team
Ms. Li presenting a banner to Professor Xie (first from the left) and the team
Using technology and warmth
To safeguard the elderly’s “stable happiness”
love
Behind this surgery is the strong support of the outstanding orthopedic discipline at Zhejiang University Hospital and the relentless efforts of the expert team focused on patient needs. The successful treatment not only signifies a rebirth for a family but also reflects the progress of Chinese orthopedics towards precision and internationalization.
Professor Hu Yihe, the director of orthopedics at Zhejiang University Hospital, stated, “We aim to transform complex revisions into ‘standardized operations’ to benefit more elderly patients. When medical technology is human-centered, making complex surgeries simple and safe, it helps them embrace a happy life!”

Professor Hu Yihe reminds us: fractures themselves are not terrifying, but the complications arising from prolonged bed rest due to fractures in the elderly can be very dangerous. It is recommended that women over 50 and men over 60 check their bone density annually to prevent “fragility fractures” early. If an elderly person falls and experiences hip pain and cannot stand, they should promptly call 120 to visit a reputable hospital for timely and standardized treatment. Fracture patients often worry about the risks of infection or loosening after joint replacement. In fact, with breakthroughs in 3D printing technology, doctors can customize prostheses based on CT data modeling, accurately filling defect areas and even reconstructing multiple bone structures. Scientific plans and advanced equipment make treatment more efficient and safe. Facing it positively and trusting medicine is the key to recovery.
 This article is an original piece from Zhejiang University HospitalFor reprints, please contact usThis article’s correspondents: Zhou Jie, Wu Rong from the Orthopedics Department of Zhejiang University Hospital
This article is an original piece from Zhejiang University HospitalFor reprints, please contact usThis article’s correspondents: Zhou Jie, Wu Rong from the Orthopedics Department of Zhejiang University Hospital
Experts in this article

 This issue’s cover
This issue’s cover

Remember to like, share, and follow!