Research Background and Objectives
The DANAMI-3-PRIMULTI trial has confirmed that in patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease (MVD), fractional flow reserve (FFR)-guided complete revascularization (FFR-CRV) can significantly reduce the need for subsequent ischemia-driven revascularization (ID-RV), but it has no significant impact on mortality or reinfarction.
The core questions of this substudy:
– Which lesions led to ID-RV in the IRA only group versus the FFR-CRV group?
– What are the anatomical characteristics (location, degree of stenosis) and functional significance (FFR values) of these lesions?
Research Methods
– Design: A retrospective analysis of the DANAMI-3-PRIMULTI trial, including 627 patients with STEMI and MVD.
– IRA only group (313 patients): Only the culprit lesion (IRA) was treated.
– FFR-CRV group (314 patients): FFR-guided revascularization was performed on non-IRA lesions within a median of 2 days after the initial PCI (FFR ≤ 0.80 or visually assessed stenosis ≥ 90% requiring intervention).
– Endpoints: ID-RV (revascularization driven by angina or positive ischemic tests), lesion characteristics (location, degree of stenosis, FFR values).
– Statistical methods: Descriptive analysis, chi-square test to compare differences between groups.
Key Results
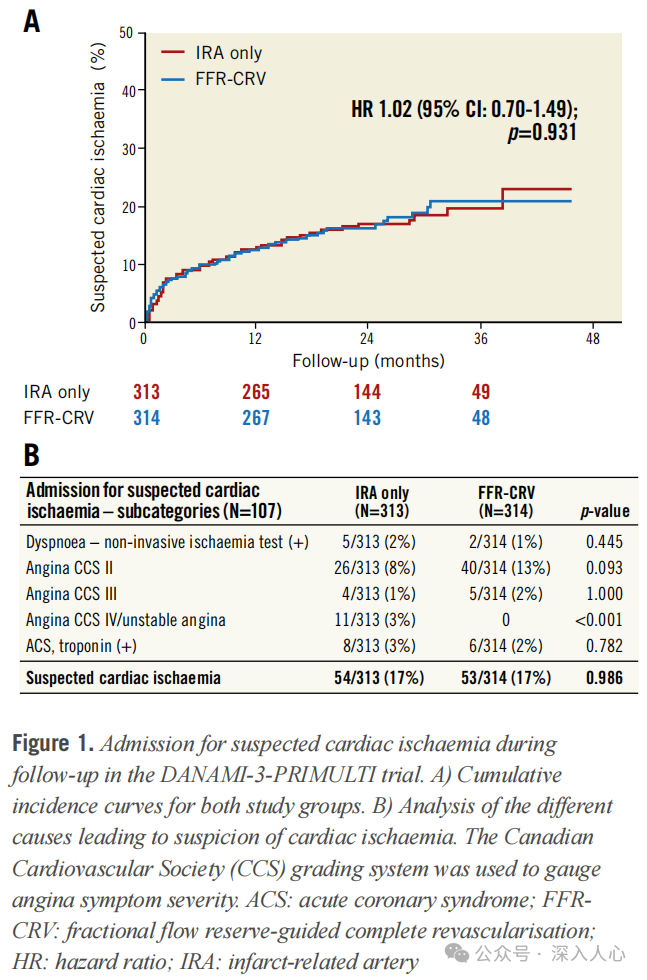
1. ID-RV incidence:
– IRA only group: 52 cases (17%) required ID-RV.
– FFR-CRV group: 17 cases (5%) required ID-RV (HR=0.32, p<0.001).
– Source of difference: 71 untreated non-culprit lesions in the IRA only group required ID-RV, while only 13 cases in the FFR-CRV group (p<0.001).
2. Lesion characteristics analysis:
– IRA only group:
– ID-RV mainly concentrated in untreated non-culprit lesions (71/82 cases, 87%).
– High stenosis (≥80%) + proximal lesions (LAD/RCA) are more likely to trigger ID-RV, often leading to class IV angina/unstable angina (11 cases, accounting for 21% of ID-RV in the IRA only group).
– FFR-CRV group:
– Only 13 untreated non-culprit lesions required ID-RV, of which 2 cases were not intervened due to procedural complexity despite FFR ≤ 0.80, and 1 case developed symptoms due to FFR borderline values (0.81-0.82).
3. Other findings:
– New lesions (de novo): The incidence was low in both groups (8 cases in the IRA only group, 7 cases in the FFR-CRV group).
– Repeat interventions on treated lesions: Rare (only 0.8% in the FFR-CRV group).
– CABG requirement: 7 cases (2.2%) in the IRA only group vs. 2 cases (0.6%) in the FFR-CRV group, not reaching statistical significance (p=0.107).
Discussion Highlights and Clinical Implications
1. Clinical value of FFR-CRV:
– Reduction of ID-RV: By screening lesions with FFR ≤ 0.80, it avoids excessive intervention on non-ischemic stenosis, reducing the need for subsequent readmissions.
– Safety: The rate of repeat interventions on treated lesions is extremely low (<1%), supporting the long-term efficacy of FFR-CRV.
2. Caution in handling certain lesion types:
– High stenosis proximal lesions (e.g., LAD proximal ≥80% stenosis): Even without FFR measurement, such lesions in the IRA only group are prone to progress to acute events (e.g., class IV angina).
– FFR borderline values (0.81-0.82) or complex lesions (bifurcation/calcification): Clinical judgment is needed to weigh the risks and benefits of revascularization.
3. Rationality of staged strategy:
– Performing FFR assessment 2 days after initial PCI can avoid interference from microvascular dysfunction during the acute phase, improving decision-making accuracy.
4. Gap between guidelines and practice:
– Although guidelines recommend complete revascularization, 78% of STEMI patients in the real world still receive incomplete revascularization, indicating a need to strengthen the clinical promotion of FFR-guided strategies.
Study Limitations
1. Missing FFR data: Non-culprit lesions in the IRA only group were not measured for FFR, making direct comparison of functional significance between the two groups impossible.
2. Sample size limitations: Subgroup analyses (e.g., CABG requirement) lacked statistical power.
3. Follow-up duration: Median follow-up of 27 months; long-term (e.g., 5 years) hard endpoints (mortality, reinfarction) effects still need verification.
Clinical Practice Recommendations
– Recommended strategy: For STEMI patients with MVD, perform FFR-guided complete revascularization during hospitalization after initial PCI (staged) to reduce ID-RV.
– Individualized decision-making:
– High stenosis proximal lesions: Even if FFR is borderline, intervention may be considered if the anatomy is complex or the blood supply area is large.
– Complex lesions with FFR ≤ 0.80: Need to consider procedural feasibility and the overall condition of the patient (e.g., renal function, bleeding risk).
Conclusion
The DANAMI-3-PRIMULTI substudy further reveals the mechanism by which complete revascularization reduces ID-RV: by screening non-culprit lesions that require intervention through FFR, it avoids leaving behind lesions with high ischemic risk. For proximal high stenosis or borderline FFR lesions, a personalized strategy should be developed based on anatomical and functional assessments. Future research is needed to explore the impact of complete revascularization on long-term hard endpoints and the optimal timing for intervention.
References:Characterisation of lesions undergoing ischaemia-driven revascularisation after complete revascularisation versus culprit lesion only in patients with STEMI and multivessel disease: a DANAMI-3-PRIMULTI substudy. EuroIntervention 2019;15:172-179
Reply086 available in PDF format.Original text.
This public account is a compilation of my study materials; conclusions and opinions are for reference only. Please be cautious when forwarding, and corrections and comments are welcome.