In just 10 weeks, you can go from a basic understanding of TensorFlow to building models such as CNNs, autoencoders, RNNs, GANs, and ultimately mastering practical development skills. Online courses will start in April, and www.mooc.ai is now open for reservations.
According to Lei Feng Network “New Intelligent Manufacturing”: Boston Consulting Group estimates that the current annual revenue of medical robots is $4 billion, and it will reach $11.4 billion by 2020, becoming the second largest robot market. This article is the first in a series on medical robots launched by New Intelligent Manufacturing, outlining the historical development trajectory of medical robots to glimpse the infinite possibilities of the future market. New Intelligent Manufacturing, as a column under Lei Feng Network, focuses on innovation and creation in the intelligent era, aiming to find opportunities worth starting a business and investing in. We will also bring more reports on industry players, capital, and startups related to medical robots, so stay tuned.
The term medical robot may be somewhat misleading, as it may lead one to think of machines that operate independently on pre-programmed tasks without supervision. Such applications are popular in industry, but human skills are also very important when dealing with human tasks.

It is generally believed that medical robots should be classified as medical devices, but they differ from traditional medical devices. They can assist doctors, enhance their capabilities, and their intelligence level will continue to grow, while also meeting the following three aspects: medical applicability, clinical adaptability, and good interactivity.
Medical robots have only started to be used in recent decades, but their presence is rapidly increasing.
Lei Feng Network has reported that according to Boston Consulting Group, the current annual revenue of medical robots is $4 billion, and it will reach $11.4 billion by 2020. Among them, the most well-known medical robot company, Intuitive Surgical, had a revenue of $2.1 billion in 2014. Thanks to the rapid growth of medical robots, commercial robots are expected to replace military robots, becoming the second largest robot market with a market value of $17 billion.
There are many reasons why the medical industry is interested in robots, which can be compared to the reasons for adopting automated machinery in manufacturing. This does not mean that the problems solved by medical robots are the same, but the benefits they bring are undoubtedly similar. The advantages that robots bring to the industry may exceed those of the most specialized and diligent medical workers, mainly including speed, accuracy, repeatability, reliability, and cost-effectiveness. A robot, no matter how long it is used, will not get tired, and its accuracy during the hundredth use is the same as during the first use.
Currently, medical robots can be mainly divided into the following categories:
-
Surgical robots: Used for surgical imaging guidance and minimally invasive surgery, mostly controlled by surgeons, who operate the robot on the patient according to input devices.
-
Rehabilitation robots: Used to assist and treat elderly, permanently or temporarily disabled patients, and those with mobility impairments. Users control the robot through visual feedback and various input devices to perform simple tasks, such as bringing food to their mouth, turning pages, or standing and walking.
-
Medical service robots: Common forms include mobile robots for transportation in hospitals, used for fetching or distributing medications, as well as disinfection and sterilization robots, which can alleviate the shortage of hospital staff and share some heavy and tedious work.
-
Laboratory robots: Used for conducting drug tests or repetitive experiments, such as HIV testing, which can save time and free up human resources for other purposes. The main reason for their popularity is their ability to perform repetitive tasks at high speed, reliably, and without fatigue.
Of course, the above classification may not cover all medical robots; there are also emotional robots used for companionship, which can help treat dementia and cognitive disorders, and can also be used for rehabilitation-type home care.
Statistics show that surgical robots currently account for the highest proportion, over 60%. This is mainly due to their early development, practicality, and significant effectiveness. However, with the development of robots and artificial intelligence technologies, rehabilitation and service robots are also catching up. In the following sections, Lei Feng Network will focus on the history of surgical robots.
The origin of a technology is often rooted in the advantages and disadvantages of its predecessors, and for surgical robots, the predecessor is laparoscopic surgery.
Laparoscopic devices themselves cannot provide haptic feedback (force and touch) and do not allow for natural coordination and dexterous operation of hand-eye movements. Moving laparoscopic instruments while watching a two-dimensional video monitor can also be somewhat counterintuitive. Additionally, during operation, the instruments must move in the opposite direction of the target aimed at on the display. These factors make it difficult to realize the advantages of laparoscopy, and to overcome these limitations has driven the development of surgical robots.
The first use of a surgical robot was the PUMA 560 in 1985, which could precisely control neurosurgical biopsies. Three years later, in 1988, the PUMA 560 was used in prostate surgery. This system also led to the emergence of PROBOT, a system specifically designed for prostate surgery.
While PROBOT was being developed, Integrated Surgical Supplies was also developing another robot. In 1992, ROBODOC was born, a robot that assisted surgeons in performing total hip replacement surgery, and it was the first surgical robot to receive FDA approval.
Also in the mid-1980s, a group of members from NASA’s Ames Research Center became interested in using virtual reality technology to develop telepresence surgery. This concept of remote surgery became one of the main driving forces behind the development of surgical robots.
In the early 1990s, several scientists from the Ames team joined the Stanford Research Institute (SRI). Collaborating with other robotic and virtual reality experts at SRI, these researchers developed a dexterous teleoperated surgical manipulator. One of their main design goals was to provide surgeons with the sensation of performing surgery directly on the patient, rather than in another room.
During the development of these robots, some general surgeons and endoscopic physicians also joined the development team and realized that these systems had great potential in improving the limitations of conventional laparoscopic surgery.
On the other hand, the U.S. military also took notice of SRI’s work and was very interested in the possibility of using telepresence to “bring surgeons to injured soldiers” to reduce wartime mortality rates. With funding from the military, researchers designed a system in which injured soldiers would be placed in vehicles equipped with robotic surgical equipment, and then operated remotely by surgeons from nearby Mobile Army Surgical Hospitals (MASH).
This system was highly anticipated and could potentially prevent soldiers from excessive blood loss before reaching the hospital, thereby reducing wartime mortality rates. The system has been successful in animal models but has not yet been tested on actual battlefield casualties.
Later, several surgeons and engineers who developed surgical robot systems for the military founded a commercial company, Computer Motion, to introduce robotic technology into civilian surgery. Notably, this company received seed funding from the military and developed the Automated Endoscope Positioning System (AESOP), a robot arm controlled by surgeons to manipulate endoscopic cameras.
Shortly after AESOP was launched, Integrated Surgical Systems (now Intuitive Surgical) obtained the license for the SRI Green Telepresence Surgery system. They then extensively redesigned the system, which ultimately became the da Vinci Surgical System. In 2000, the da Vinci robot received FDA approval, becoming the first comprehensive laparoscopic surgical robot system.
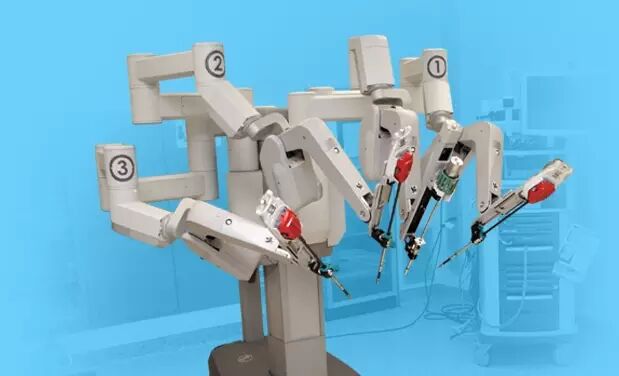
The da Vinci Surgical System mainly consists of three parts: a surgical control console, a control system, and robotic arms. The surgeon sits at the surgical control console and gives corresponding commands to the computer, while the camera provides information about the condition of the human organs, and the surgeon makes surgical decisions based on this feedback.
Within a year of the birth of da Vinci, Computer Motion’s Zeus system also went into production. The subsequent development of surgical robot systems was primarily dominated by these two companies. In 2003, Intuitive Surgical acquired Computer Motion, and the Zeus system was no longer actively marketed.

Just like the development of surgery, other types of robots, such as prosthetics and exoskeletons, have also made significant progress.
General Electric developed the first exoskeleton device in the 1960s. It was called Hardiman, a hydraulic and electric-powered wearable device. Due to its weight, it was not suitable for military use. Now, this field has seen the emergence of a series of companies like ReWalk.
With the help of robotic exoskeletons, stroke patients can recover arm mobility faster than traditional physical therapy. Sensors detect muscle strength, range of motion, and brain activity, and can inform therapists of the patient’s progress. These machines also help retrain the brain to compensate for damaged areas. Robotic systems also assist patients in relearning walking and other motor skills.
Microprocessor-equipped artificial knees entered the market in 1993. In 1998, Adaptive Prosthesis combined microprocessors with hydraulic and pneumatic controls, giving prosthetics a more natural walking ability and a more responsive adaptation to changes in walking speed. At the same time, the C-Leg, which debuted in 1997, further enhanced knee flexion control. It has developed to be very sophisticated, adapting to each user’s different conditions and enabling activities like ice skating and cycling.
Today, robotic prosthetics have sensors attached to muscles and nerves, allowing patients to feel touch and even control movement with their thoughts. Bionic hands also possess fine motor skills, capable of performing tasks such as writing, typing, or playing the piano.

The application range of medical robots has been booming in recent years. The da Vinci robot has already performed thousands of surgeries in hospitals, and it even has the precision to suture grape skins. According to Lei Feng Network, by 2015, the da Vinci surgical system had performed no less than 600,000 surgeries that year. It can be used for various surgeries, ranging from heart valve repair to tumor removal.
However, it should be noted that medical robots, especially autonomous surgical robots, are still in their infancy. For example, issues related to flexible control and the precision of tactile feedback have not yet been resolved; issues regarding multi-information integration, visualization, sensing, and how to achieve comprehensive human-machine interaction are still present. There are also many problems in regulation and access, as safety and efficacy are essential thresholds for medical device registration.
Future medical robots will certainly make trauma smaller, achieve simplicity, safety, integration, and be suitable for doctors’ operating habits. In the future, there may even be direct control, achieving a master-slave integration, making them smaller and more convenient.
It can be said that robotic surgery has achieved the goal of eliminating the limitations of laparoscopic surgery. Even the latest and most innovative technologies in modern medicine can be simply summarized as: robots.
Appendix: Small Details About the History of Medical Robots
-
The world’s first surgical robot was the Arthrobot, developed and used in Vancouver, Canada in 1983, a robot for hip replacement surgery.
-
The first use of a surgical robot was the PUMA 560 in 1985.
-
Intuitive Surgical was founded in 1995.
-
In December 2003, in Tampa, USA, a woman died after her husband accidentally severed a main blood vessel during surgery with a surgical robot, and the hospital was sued.
-
In May 2006, Italy performed the first unmanned robotic surgery.
-
In June 2008, the German Aerospace Center (DLR) developed the first minimally invasive surgical robot system with force feedback.
-
In September 2010, the University Medical Center in Ljubljana performed a robotic surgery on the femoral vascular system, which can be said to be a true robot, as it did not replicate human hand movements but operated autonomously after pressing a button.
|
Click on keywords to view related historical articles ● ● ● Recent Hot Topics 15 minutes to charge 5000mAh, is the “graphene battery” back again? Exclusive | A long interview with Alibaba’s Yan Zhijie, a 360-degree understanding of the mysterious iDST Dialogue with Li Zhifei: The biggest dilemma of Out of the Door in recent years Google engineer recounts why TPU is 30 times faster than CPU and GPU? Should Chinese companies buy Imagination after Apple’s treatment? Li Gang from Ofo: The despair brought by Didi has passed Uber’s chaos revealed: the autonomous driving team has fallen into a “small civil war” Peaceful breakup? You have no idea what happened to Andrew Ng at Baidu Heavyweight | Tear off the e-commerce label, restore Alibaba’s real intention of “NASA” From the perspective of the supply chain, can we really resist Korean goods? How does today’s headline engine work? Dark web credit card purchase record: personal experience of no-threshold fraud What are the advantages of 5G over 4G? After reading this article, you will understand. Latest Courses
|
