
 Jing Yuming Professor
Jing Yuming Professor
Deputy Chief Physician of Urology at Xijing Hospital.
Academic Positions: Member of the Minimally Invasive and Robotic Surgery Group of the Urology Branch of the Chinese Medical Doctor Association, Member of the Urology and Male Reproductive Association of the China Medical Healthcare International Exchange Promotion Association, Vice Chairman of the Minimally Invasive Urology Branch of the Shaanxi Medical Promotion Association, Executive Member of the Multidisciplinary Cooperation Committee for Urological Diseases of the Shaanxi Association of Traditional Chinese and Western Medicine, Member of the Urology Branch of the Shaanxi Medical Promotion Association, Member of the Urological Tumor Committee of the Shaanxi Anti-Cancer Association, Member of the Minimally Invasive Urology Branch of the Shaanxi Medical Doctor Association, Member of the Andrology Branch of the Shaanxi Medical Doctor Association, Member of the Sexual Medicine Committee of the Shaanxi Health Association, Member of the Urology Branch of the Xi’an Cancer Rehabilitation Association.
Expertise: Laparoscopic and robotic minimally invasive surgery in urology, especially radical cystectomy and orthotopic neobladder surgery for bladder cancer, radical prostatectomy, and comprehensive treatment of malignant tumors in the urinary system. Published over twenty articles in domestic and international journals, chief editor of one monograph, and co-editor of three monographs, Editorial Board Member of the Journal of Modern Urological and Reproductive Tumors.
 Zhao Hongfan Professor
Zhao Hongfan Professor
Resident Physician in Urology at Xijing Hospital, Doctor of Medicine.
Published six papers in journals such as Ebiomedicine and Advances in Therapy, obtained two new practical patents, and participated in several national and provincial research projects.
Patient Basic Information:
General Information: 74 years old, female.Main Complaint: A mass in the right renal pelvis discovered during a physical examination for over two weeks. Past Medical History: Healthy.
Physical Examination: Symmetrical bilateral costovertebral angles, no tenderness or percussion pain in both renal areas, and both kidneys not palpable below the ribs. No tenderness in the area of both ureters, no masses or tenderness palpated. No fullness or tenderness in the suprapubic bladder area.
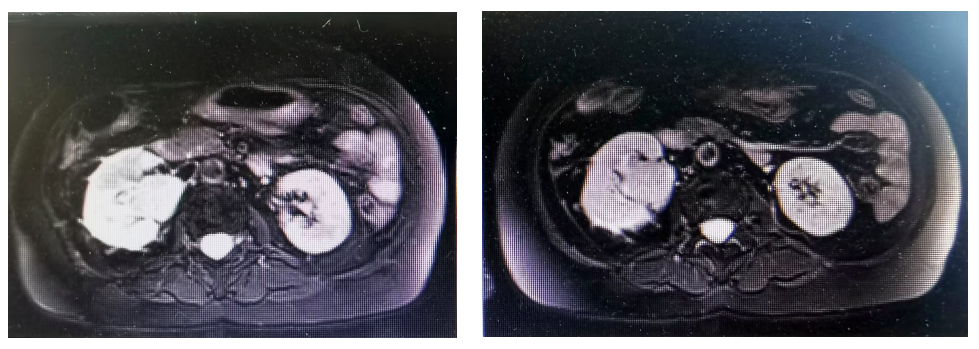
Key Imaging Examination: Enlarged right kidney, with a mass-like soft tissue signal in the right renal pelvis, showing mild progressive enhancement, approximately 3.2X4.4cm in size. An irregular patchy T2 signal is seen in the adjacent right upper back, with uneven mild progressive enhancement in the adjacent cortex, and irregular large areas of reduced enhancement inside. Fine vascular shadows are seen at the lower pole of the right kidney, with an irregular margin, and no obvious dilation of the right renal calyx. The left kidney shows no significant abnormalities in shape or signal, with no obvious dilation of the left renal pelvis or calyx, and no significant enlarged lymph nodes in the abdominal cavity or retroperitoneum, with no abdominal effusion.
Laboratory Tests: No significant abnormalities in blood routine or liver and kidney function.
Treatment Process
STEP 1:Cystoscopy: No new growths seen in the bladder.
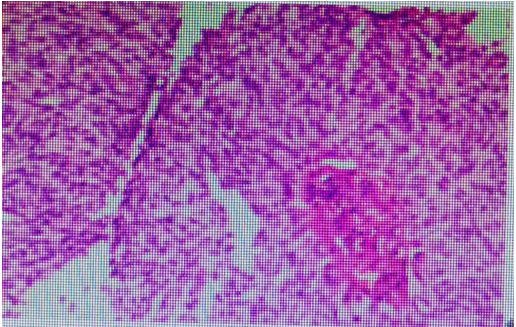
STEP 2:Laparoscopic right kidney ureter bladder partial resection; postoperative pathology indicated: (right renal pelvis) consistent with low-grade papillary urothelial carcinoma, invading the renal parenchyma, with no cancer tissue found at the ureter stump, part of the bladder, renal vascular, or perirenal fat.
Sent for examination (right renal hilar lymph nodes) showed no metastatic cancer. Pathological staging: pT3N0.
Immunohistochemistry: p63(+), CK7(+), P40 (focal +), CK20(-), P53 (scattered +), GATA3 (weak +), HER-2 (2+), Ki-67 (+, about 30%).
Risk Stratification: High risk.
According to the 2024 version of the CSCO Guidelines for Diagnosis and Treatment of Urothelial Carcinoma in China, high-risk patients include those with one of the following characteristics: multifocal disease; tumor size >2cm; hydronephrosis; high-grade urine cytology or ureteroscopic biopsy; CT or MRI showing local invasion; biopsy pathology with other tissue components.
STEP 3:Postoperative adjuvant therapy started one month after surgery: regimen: Gemcitabine (1000mg/m2, on days 1 and 8) + Cisplatin (70mg/m2, on day 1) + PD-1 inhibitor (once every three weeks) for a total of 4 cycles, with no severe adverse reactions observed.
STEP 4:After August, follow-up ultrasound (2024-04-02) revealed: examination of the mass described by the patient in the right flank: imaging of the fat layer, cannot rule out metastatic lesions, recommended to combine with puncture biopsy; pathological examination indicated: (post right renal pelvis cancer, right abdominal) infiltrative cancer found in fibrous tissue, supported by medical history and immunohistochemistry results for infiltrative urothelial carcinoma.
Immunohistochemistry: HER2 (2+).
Main examination: Enhanced CT of the chest and abdomen indicated: solid lesions in the left lower lobe and right upper lobe increased compared to before, likely metastatic.
Started treatment with Vadimezan 120mg + Toripalimab 240mg, every two weeks, with follow-up after six cycles.
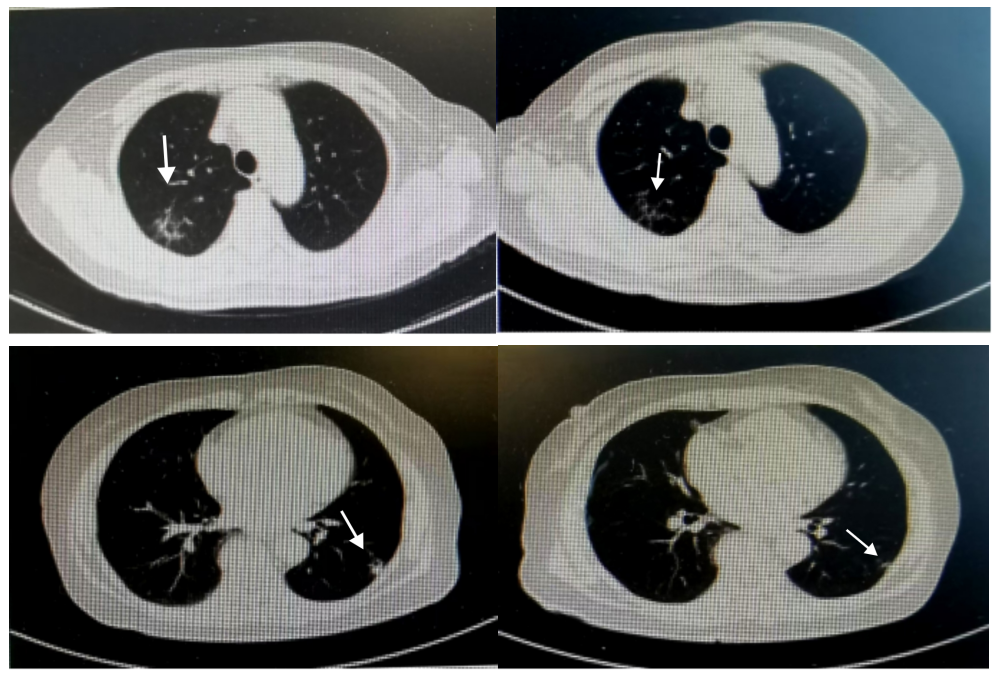
Significant reduction in lung metastatic lesions. Follow-up ultrasound: outpatient examination of superficial color Doppler ultrasound indicated: examination of the mass in the right flank: a low echo of 1.7×1.0x1.2cm visible in the fat layer, with clear boundaries and regular shape. Considered as metastatic lesions.
Considering tumor invasion into the subcutaneous fat layer, traditional surgery would inevitably cause defects in the skin, subcutaneous tissue, and muscle layers, affecting postoperative functional recovery and possibly facing recurrence risks. In contrast, “intraoperative radiotherapy” can concentrate the radiation dose in the 1 cm thick risk area, effectively eliminating hidden cancer cells while protecting surrounding healthy tissue. Therefore, performed subcutaneous tumor resection in the right flank + intraoperative radiotherapy.
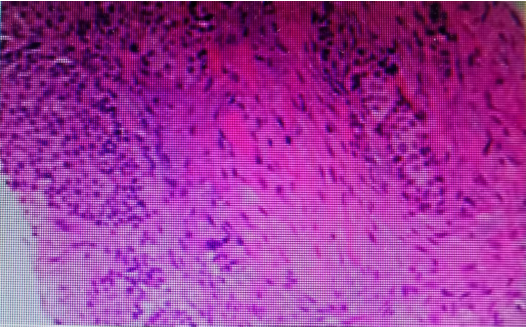
Postoperative pathology indicated: infiltrative cancer found in fibrous tissue, supported by medical history and immunohistochemistry results for infiltrative urothelial carcinoma.
Immunohistochemistry results: CK20(-), CK5/6(+), CK7(+), GATA3(+), p16(-), p53 (wild-type expression), p63(+), Pax-8 (focal +), TTF-1(-), Uroplakin III(-), Ki-67 proliferation index approximately 25%, HER2(1+).
Intraoperative Radiotherapy



Subsequent Maintenance Treatment
Considering the patient is an elderly female, weighing 46kg, the medication regimen was adjusted: Vadimezan 120mg + Toripalimab 240mg, once every four weeks, with follow-up after three months. Currently, treatment has been ongoing for 14 months with good disease control and no significant adverse reactions observed.
Summary
First point: In metastatic lesions of renal pelvis urothelial carcinoma, the combination of Vadimezan and immunotherapy plays an important role in controlling disease progression and tumor shrinkage. Although there is a strong correlation with HER2 expression in metastatic lesions, in this case, the treatment effect was also observed in HER2 weakly positive (1+) tumors.
Second point: The overall safety of Vadimezan treatment is good, with no significant adverse reactions during the treatment process, and no significant abnormalities in laboratory tests.
Third point: For the subcutaneous tumor in the right flank, the combination of Vadimezan and immunotherapy also has a tumor-shrinking effect. We first applied the technique of subcutaneous tumor resection in the flank along with intraoperative radiotherapy, providing important safety assurance for this patient’s life.
In recent years, urology has continuously innovated in disease diagnosis and treatment concepts, therapeutic methods, and surgical models, integrating various treatment modalities such as surgery, radiotherapy, chemotherapy, immunotherapy, and antibody-drug conjugates (ADC) into a “combination punch” strategy, which has become a key strategy for improving efficacy.
This treatment approach, combining intraoperative radiotherapy, showcases its potential application in important scenarios such as bladder-preserving treatment and advanced comprehensive treatment, leveraging its advantages of precise targeting and efficient control. With the continuous accumulation of clinical cases, the “dual sword combined” therapy, which integrates precise surgical operations with the thorough elimination advantages of radiotherapy, is expected to open doors of hope for more complex cases.
Disclaimer:This content is intended for reading by medical and pharmaceutical professionals only and does not constitute actual treatment advice. Please contact for authorization for reprints; infringement will be pursued!
Editor: Wu Mengxia
Reviewed by:Huang Pengcheng