Research Background and Objectives
In patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease (MVD), the strategy of complete revascularization (CRV) can reduce ischemic events, but its impact on bleeding risk remains unclear.
Core Questions:
– Does staged complete revascularization (FFR-guided) during hospitalization increase the risk of severe bleeding?
– What is the impact of complete revascularization on minor bleeding events and patient prognosis?
Research Methods
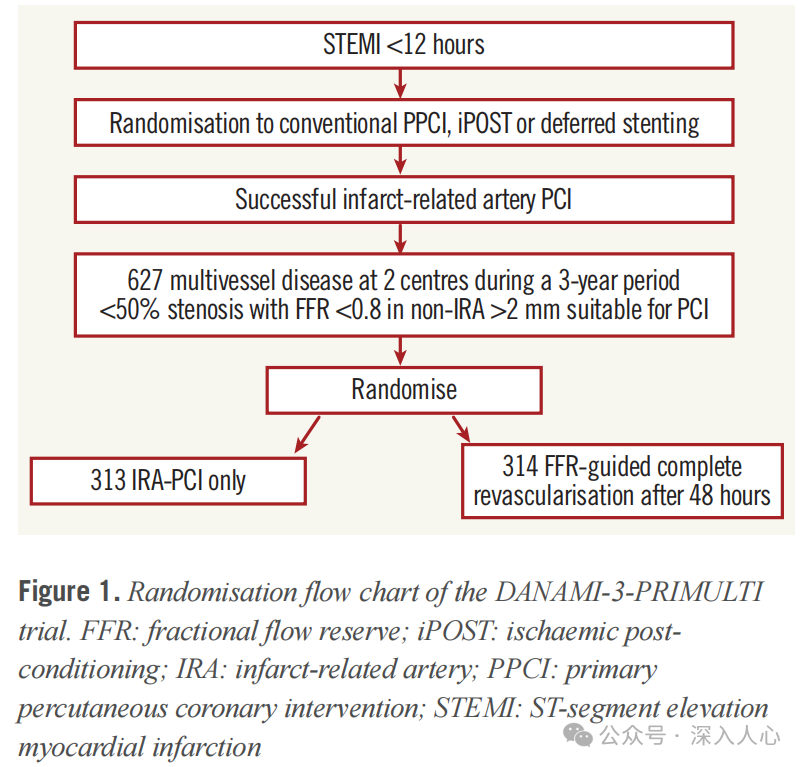
– Design: A retrospective analysis based on the DANAMI-3-PRIMULTI trial, including 627 patients with STEMI and MVD.
– Control group (IRA-PCI only group, 313 cases): Only the culprit lesion (IRA) was treated.
– Intervention group (FFR-CRV group, 314 cases): FFR-guided complete revascularization was performed within a median of 2 days (IQR 2-4 days) after initial PCI.
– Endpoints:
– Primary endpoint: Severe bleeding defined by TIMI and BARC criteria (major + minor bleeding).
– Secondary endpoints: Minor bleeding (e.g., puncture site oozing), length of hospital stay, one-year mortality.
– Statistical methods: Intention-to-treat (ITT) analysis and as-treated analysis, Cox proportional hazards model to assess risk factors.
Key Results
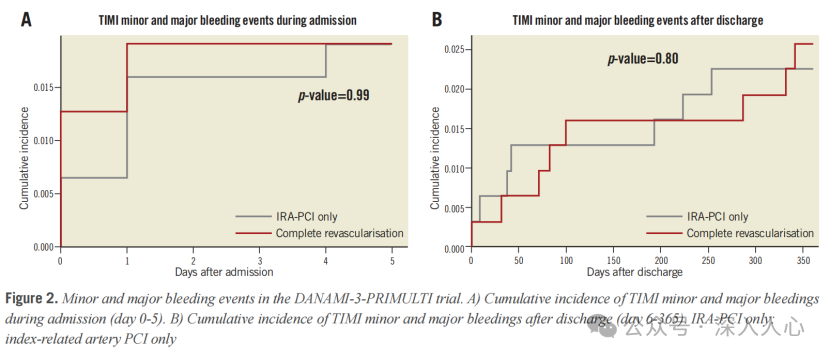
1. No difference in severe bleeding events:
– During initial PCI: The incidence of TIMI major + minor bleeding was approximately 1% in both groups (p=0.99).
– During the second procedure: No TIMI major or minor bleeding events occurred in the FFR-CRV group.
– Severe bleeding within one year: The incidence was 4.3% in both groups (p=0.85).
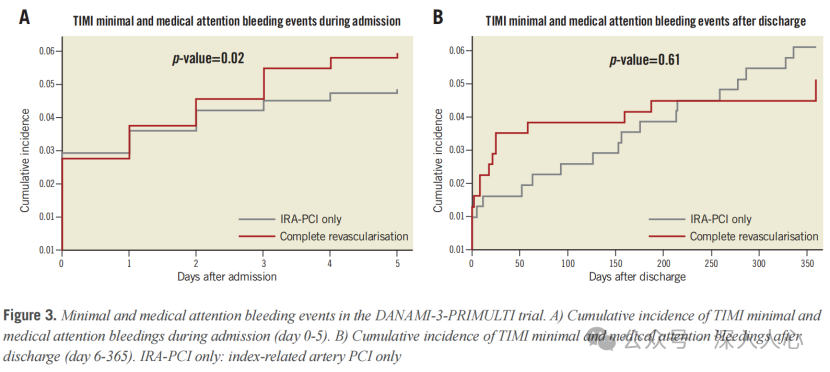
2. Increased minor bleeding events:
– Minor bleeding during hospitalization: The FFR-CRV group had a higher incidence (61.5% vs. 49.5%, p=0.003), mainly due to puncture site oozing (21% vs. 8%, p<0.001).
– Minor bleeding after discharge: No difference between the two groups (p=0.61).
3. Other findings:
– Length of hospital stay and mortality: The median length of stay was 5 days in both groups (p=0.4), with no difference in one-year mortality (2.2% vs. 2.6%, p=0.8).
– Multivariable analysis: Male gender was a protective factor for minor to moderate bleeding (HR=0.15), while high systolic blood pressure (>191mmHg) and the use of glycoprotein IIb/IIIa inhibitors were risk factors.
Discussion and Clinical Implications
1. Safety validation:
– Staged complete revascularization does not increase the risk of severe bleeding, supporting its safety in reducing ischemic events.
– Increased minor bleeding but no clinical significance: Puncture site oozing does not affect length of stay or mortality and can be considered operational “background noise.”
2. Impact of procedural details:
– Low radial artery access rate (only 6%): The study period was from 2011 to 2014, when radial access was not yet widespread; if a modern radial-first strategy were adopted, the bleeding risk might be further reduced.
– Antithrombotic regimen: 75% of patients used bivalirudin, which may reduce bleeding risk, but differences between antithrombotic regimens were not compared.
3. Limitations:
– Sample size limitation: The incidence of severe bleeding events was low (2.1%), which may be insufficient to detect small differences.
– Exclusion of high-risk patients: Patients with coagulopathy, severe renal dysfunction, and other high bleeding risk factors were excluded from the study, which may underestimate the true risk.
Clinical Practice Recommendations
– Recommended strategy: For patients with STEMI and MVD, staged FFR-guided complete revascularization during hospitalization is safe, with a preference for radial access to reduce puncture site bleeding.
– Individualized antithrombotic therapy: Adjust the antithrombotic regimen based on the patient’s bleeding risk (e.g., age, renal function) to avoid excessive use of glycoprotein IIb/IIIa inhibitors.
Conclusion
The DANAMI-3-PRIMULTI substudy indicates that while staged complete revascularization increases minor bleeding events, it does not elevate the risk of severe bleeding or mortality, providing critical safety evidence for the clinical promotion of this strategy. Future efforts should integrate modern interventional techniques (such as radial access) and new antithrombotic agents to further optimize treatment strategies.
References:Bleeding episodes in “complete, staged” versus “culprit only” revascularisation in patients with multivessel disease and ST-segment elevation myocardial infarction: a DANAMI-3-PRIMULTI substudy.
Reply083Available in PDF format.Original text.
This public account is a compilation of my study materials; conclusions and opinions are for reference only. Please be cautious when forwarding, and corrections and comments are welcome.