The burden of atherosclerotic cardiovascular disease (ASCVD) in our country continues to increase, and the prevention and control situation is severe. Low-density lipoprotein cholesterol (LDL-C) is a pathogenic risk factor for ASCVD. In recent decades, the prevalence of dyslipidemia among individuals aged 18 and older in our country has significantly increased, but the awareness, treatment, and control rates remain low.
01What Indicators Are Measured in Lipid Testing?
Four Basic Indicators: Clinical lipid testing is recommended to include total cholesterol (TC), triglycerides (TG),LDL-C, and high-density lipoprotein cholesterol (HDL-C).
Three Optional Indicators: Conditional medical institutions can conduct tests for apolipoprotein A1 (ApoA1),ApoB, and lipoprotein (a) [Lp(a)].
02Why Are These Indicators Tested?
TC refers to the total cholesterol contained in various lipoproteins in the blood.
LDL-C is a pathogenic risk factor for ASCVD and is the primary therapeutic target for lipid-lowering treatment.
HDL-C: Generally, HDL-C levels are negatively correlated with ASCVD risk.
Non-HDL-C=TC-(HDL-C), is the secondary intervention target for lipid-lowering treatment, representing the total amount of cholesterol in all lipoproteins containing apolipoprotein B (ApoB).
TG is a risk factor for ASCVD and is also considered a risk factor for increased ASCVD risk during risk stratification. For patients whose LDL-C levels are at target but still have high TG, treatment to lower TG should be considered to further reduce ASCVD risk.
03Who Needs Lipid Testing?General Population
It is recommended that adults under 40 years old undergo lipid testing every 2 to 5 years (including TC, LDL-C, HDL-C, and TG).
Adults aged 40 and older should have at least one lipid test each year.
Key Populations
(1) Individuals with a history of ASCVD;
(2) Individuals with multiple ASCVD risk factors (such as hypertension, diabetes, obesity, smoking);
(3) Individuals with a family history of early-onset ASCVD (first-degree relatives <55 years for males or <65 years for females) or familial hyperlipidemia;
(4) Individuals with xanthomas or thickening of the Achilles tendon.
Collect venous blood, maintaining daily dietary habits and stable weight for at least 2 weeks prior to blood collection, avoiding vigorous physical activity within 24 hours, fasting for 8 to 12 hours, and resting in a seated position for at least 5 minutes.
04How to Interpret Lipid Test Results to Determine if They Are Within Target Levels?
Step 1: Overall ASCVD Risk Assessment.
With ASCVD → Secondary Prevention
-
Very High-Risk Population: Among individuals diagnosed with ASCVD, those who have experienced ≥2 serious ASCVD events or have had 1 serious ASCVD event with ≥2 high-risk factors are classified as very high-risk.
-
High-Risk Population: Other ASCVD patients.
No ASCVD → Primary Prevention
-
High-Risk Population: Individuals meeting any of the following three conditions do not need further ASCVD 10-year incidence risk assessment: (1) LDL-C ≥4.9mmol/L or TC ≥7.2mmol/L; (2) Diabetic patients aged ≥40; (3) CKD stages 3-4.
-
Low, Moderate, and High-Risk Populations: Individuals who do not meet the above three conditions (including diabetic patients <40 years old): When considering whether lipid-lowering treatment is needed, an assessment of the overall 10-year ASCVD incidence risk should be conducted, with average risks of <5%, 5%-9%, and ≥10% defined as low, moderate, and high risk, respectively.
Step 2: Based on ASCVD risk stratification, assess whether lipid levels are within target and develop corresponding lipid-lowering strategies.
The main lipid indicators reference standards for low-risk populations (non-diabetic patients) in ASCVD primary prevention are shown in the table below.
Appropriate Levels for Lipid Indicators are TC <200 mg/dl; LDL-C <131 mg/dl; TG <150 mg/dl; non-HDL-C <158 mg/dl.
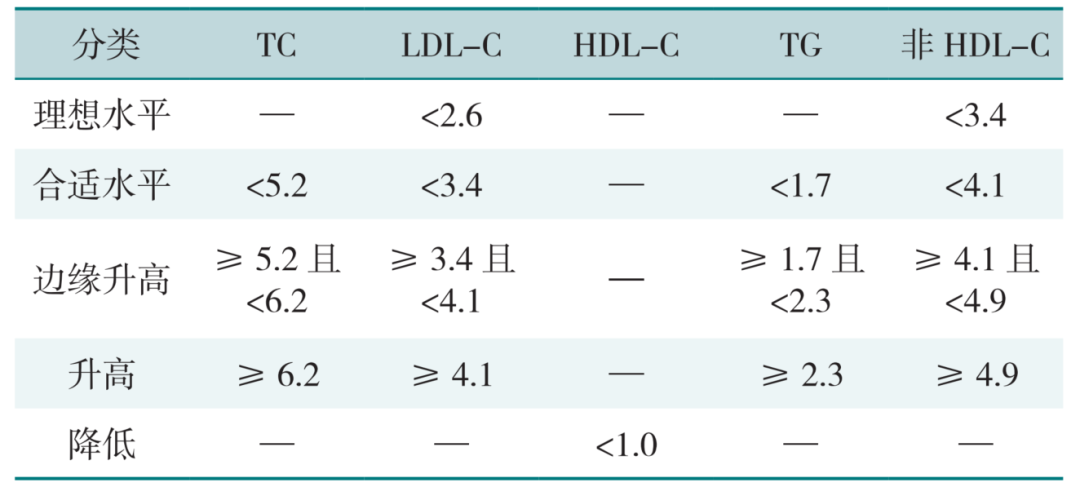
Unit: mmol/L
The expression units for the measured values of each lipid item are according to national standards in mmol/L (or g/L), while some countries internationally use mg/dl, with the conversion factors as follows:
[TC, HDL-C, LDL-C] 1.0 mmol/L = 38.6 mg/dl;
[TG] 1.0 mmol/L = 88.5 mg/dl;
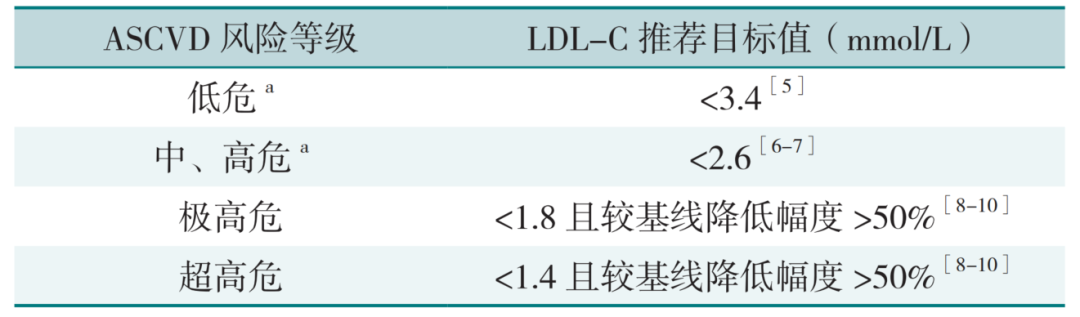
Different ASCVD risk levels correspond to different LDL-C control levels. The target values for LDL-C are shown in the table below.
05Prioritize Healthy Living Before Considering Medication for Lipid Lowering
Lipid-lowering treatment includes lifestyle interventions and pharmacotherapy.
Healthy lifestyle changes are recommended first, including a balanced diet, moderate physical activity, weight control, smoking cessation, and limiting alcohol consumption. Among these, a balanced diet has a significant impact on lipid levels, primarily by limiting the intake of saturated and trans fatty acids and increasing the intake of vegetables, fruits, whole grains, dietary fiber, and fish.
Lipid-lowering medications are categorized based on their primary effects into those that primarily lower cholesterol and those that primarily lower TG.
-
Lipid-lowering medications that reduce cholesterol include statins, cholesterol absorption inhibitors, PCSK9 inhibitors, probucol, bile acid sequestrants, and other lipid-lowering drugs (e.g., ezetimibe, polyunsaturated fatty acids).
-
Medications that lower TG primarily include fibrates, ω-3 polyunsaturated fatty acids (high-purity medical prescription grade), and niacin.
In populations without ASCVD, if lipid targets are not achieved after 3 months of lifestyle intervention, consideration should be given to adding lipid-lowering medications. Statins are the cornerstone of lipid-lowering therapy for dyslipidemia. Moderate-intensity statins are the first-line strategy for lipid-lowering treatment in the Chinese population. Combination therapy with lipid-lowering medications is a fundamental trend in the treatment strategy for dyslipidemia. Hot Topics
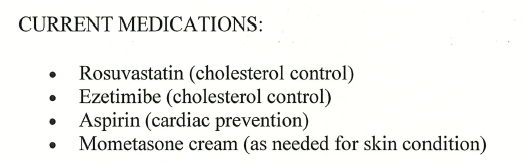
Recently, the White House published the results of the current President Donald Trump’s health examination conducted last Friday. The report shows that the 78-year-old Trump, under the combined use of rosuvastatin (a statin) and ezetimibe (a cholesterol absorption inhibitor), has reduced TC to 3.6 mmol/L (optimal value <5.2 mmol/L), TG to 0.63 mmol/L (normal value <1.7 mmol/L). HDL-C (good cholesterol) is 2.0 mmol/L (ideal value >1.0 mmol/L), and LDL-C (bad cholesterol) is 1.3 mmol/L (optimal value <2.6 mmol/L).
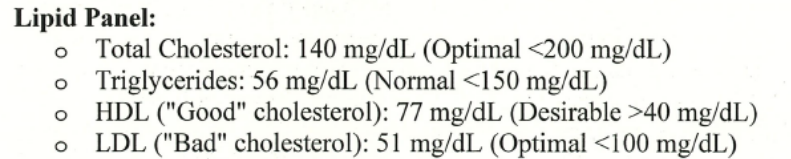
It is worth mentioning that the LDL-C level reported this time is not only below the recommended target value for low-risk ASCVD in our country (<2.6 mmol/L) but also lower than the recommended target value for very high-risk ASCVD in our country (<1.4 mmol/L).
References:1. Chinese Lipid Management Guidelines (Primary Care Version 2024)2. Chinese Lipid Management Guidelines (2023 Edition)3. White House Website
Previous Recommendations
Summary Article | 9 Mechanisms of Atrial Fibrillation and ECG Manifestations
Evolut Low Risk Trial Interpretation: The 5-Year Outcomes of TAVR in Low-Risk Aortic Stenosis Patients Are Not Inferior to SAVR! | ACC.25
Oral Semaglutide Can Reduce Cardiovascular Event Risk by 14%! Professor Xue Yajun’s Team Interprets the Semaglutide Cardiovascular Outcomes (SOUL) Trial
Summary by Xiao Xun
More Selected Content