The incidence of SOM in children varies across different age groups and regions, with detection rates ranging from 1.16% to 30.7%, predominantly affecting preschool children. Risk factors for SOM in children include Down syndrome, cleft palate, and autism.
Eustachian Tube Dysfunction
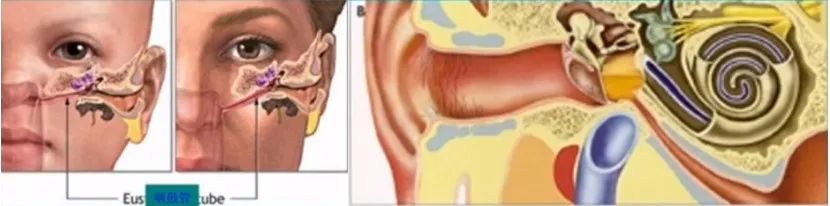
Eustachian tube anatomical diagram
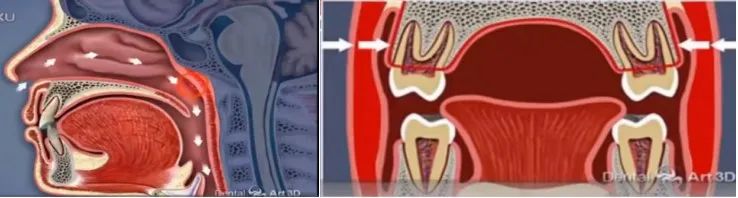
Adenoid hypertrophy and other obstructive diseases leading to mouth breathing
(3) Mucosal Changes in the Eustachian Tube: The “mucociliary transport system” in the Eustachian tube continuously expels pathogens and secretions to the nasopharynx. Conditions like congenital ciliary dyskinesia, bacterial exotoxins, inflammatory secretions from the middle ear and Eustachian tube, and acute or chronic sinusitis or bronchitis can cause abnormal mucus secretion and ciliary movement disorders, leading to blockage of the Eustachian tube.
(4) Local Developmental Abnormalities: Children with cleft palate may have abnormal development of the levator veli palatini muscle, preventing effective contraction, or the fibers of the tensor veli palatini muscle may be underdeveloped, reducing the Eustachian tube’s drainage and pressure-equalizing functions, leading to prolonged negative pressure in the middle ear and fluid accumulation.
Infectious Factors
SOM was once thought to be a sterile inflammation of the middle ear, but recent findings indicate that it is related to infections, with the most common bacteria being Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, as well as viruses like respiratory syncytial virus, adenovirus, rhinovirus, and coronaviruses. Patients may have varying degrees of bacterial biofilms on the nasopharyngeal and middle ear mucosal surfaces, leading to recurrent SOM and chronic suppurative otitis media.
(1) Allergic Reactions: The proteins and enzymes in the effusion of the tympanic cavity are secretions rather than exudates, possibly belonging to immune complex (III) diseases; patients with allergic rhinitis have a higher incidence of SOM due to mucosal edema at the Eustachian tube orifice caused by rhinitis, which may be due to an immediate hypersensitivity (I) reaction or a delayed hypersensitivity (IV) reaction mediated by T cells.
(2) Immunoglobulin Deficiency: Secretory IgA produced by the upper respiratory mucosa can prevent pathogen adhesion and clear resident flora in the nasopharynx. In children, the immune system is not fully developed, and the lack of secretory IgA may lead to a higher incidence and recurrence of SOM.
Other Factors: Passive smoking, obesity, endocrine diseases, improper breastfeeding positions, excessive use of pacifiers, and gastroesophageal reflux in infants can trigger SOM.
1. Hearing Abnormalities:
(1) Some children may complain of hearing loss, often manifesting as ignoring calls or being inattentive in class, which is noticed by parents or teachers; they may also experience noises in the ear, enhanced self-hearing, and/or changes in hearing with position changes;
(2) It is also possible for one ear to be affected while the other remains normal, going unnoticed for a long time until a comprehensive examination during a check-up reveals it;
(3) Infants may show delayed responses to speech and environmental sounds, and prolonged hearing loss can lead to speech development disorders in preschool children.
2. Ear Fullness:: Children may feel a sense of fullness or blockage in the ear, which can be temporarily relieved by repeatedly pressing on the ear.
3. Ear Pain:: Usually transient and mild, this characteristic increases the subtlety of SOM.
4. Tinnitus:: Often low-pitched and intermittent, such as “crackling” sounds, “buzzing” sounds, and “water flow” sounds, with sounds of air passing through water when moving the head or yawning.
5. Dizziness and Unsteadiness: A few children may exhibit vestibular symptoms and balance abnormalities.

Acute phase tympanic membrane congestion in SOM, light reflex shallow or absent

Tympanic membrane with effusion and air bubble signs
(3) Pneumatic Otoscopy: Dynamic changes in the tympanic membrane can be observed.

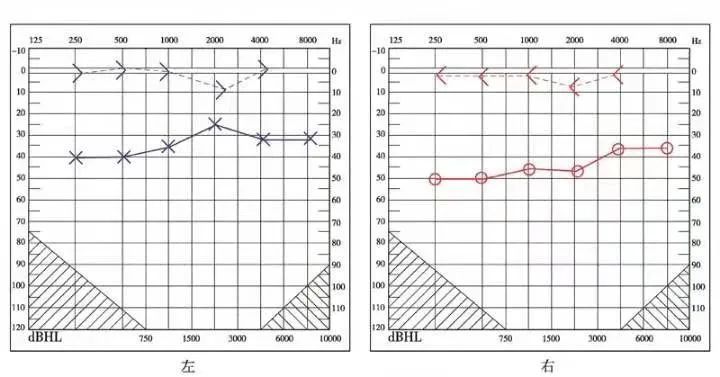
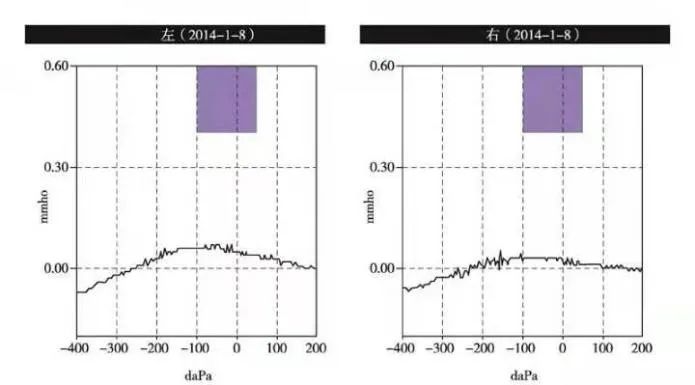
Typical “B” type image of acoustic impedance testing for SOM

WBA images indicating middle ear effusion and negative pressure
4. Objective Audiometry
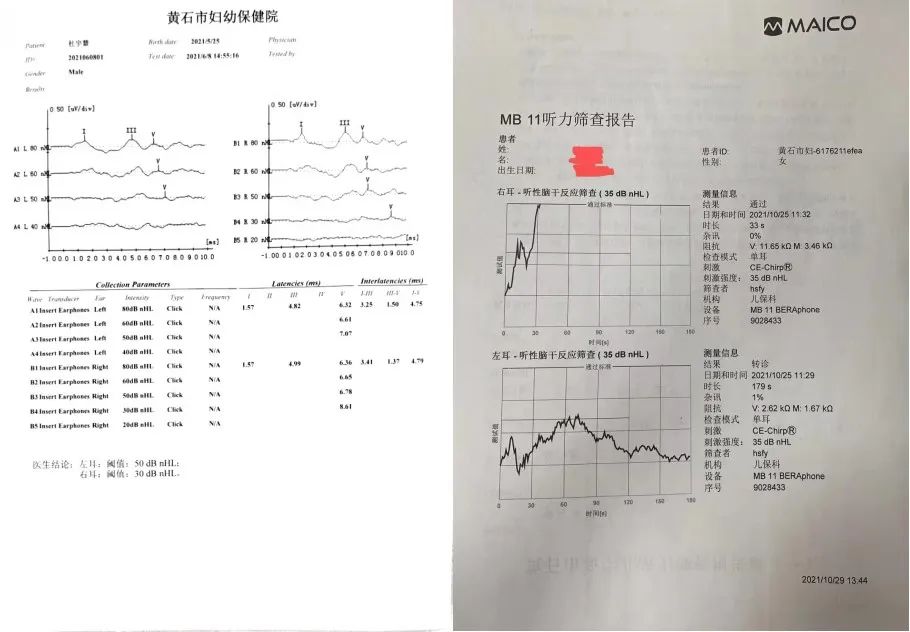
ABR and AABR test result reports
5. Nasopharyngeal Examination: The ear, nose, and throat cavities are interconnected, and inflammation can affect one another; thus, clinical practice often requires examination of the nasal and pharyngeal areas and simultaneous treatment of related diseases.

6. Imaging Examination: Not routinely recommended, but CT scans of the temporal bone may be performed if necessary.
Based on the medical history and clinical presentation, combined with otoscopy and audiometric examinations, diagnosing SOM is not difficult. Clinically, it is often necessary to differentiate it from acute suppurative otitis media, nasopharyngeal masses, cholesterol granulomas, cerebrospinal fluid otorrhea, acute middle ear barotrauma, and jugular bulb tumors.
SOM is a self-limiting disease with a high spontaneous recovery rate; children with a history of less than 3 months and without high-risk factors should avoid unnecessary medical interventions and have regular follow-ups.
(5) Decongestants: Can reduce nasal mucosal swelling but have no definitive effect on improving SOM symptoms and may have adverse effects; routine use is not recommended.
-
Indications: Unilateral or bilateral SOM lasting more than 3 months, tympanometry showing type B or C, meeting one of the following conditions: ① Hearing loss in the affected ear ≥25 dB HL, with an air-bone gap, or affecting speech communication and learning; ② Significant retraction, adhesion, and/or effusion of the tympanic membrane; ③ ≥3 episodes within 6 months or ≥4 episodes within 1 year.
-
Ventilation tubes: When choosing, consider the possibility of SOM recurrence and the patient’s compliance with follow-up; they are usually placed in the anterior or posterior inferior part of the tympanic membrane, away from the annulus. Recommendations: ① For children ≤6 years, choose T-tubes; for >6 years, choose button tubes; ② For those unable to follow up on time, button tubes are recommended; ③ For those with allergic rhinitis, T-tubes may be used initially; ④ For retracted tympanic membranes, button tubes are preferred; ⑤ For completely retracted tympanic membranes or narrow tympanic cavities, T-tubes may be selected.

Different types of middle ear ventilation tubes
-
Complications include ear discharge, tympanic membrane perforation, retraction, and cholesteatoma formation, and tympanic sclerosis. The management principles are: ① Keep the ear canal clean and dry postoperatively; ② If ear discharge occurs, local infection control with antibiotic or corticosteroid + antibiotic ear drops is recommended; routine systemic antibiotics are not recommended, and removal of the ventilation tube is not advised during discharge; ③ For persistent tympanic membrane perforations, tympanoplasty may be scheduled; ④ For retraction pockets and cholesteatoma formation, surgery should be scheduled; ⑤ Tympanic sclerosis is generally not treated.
-
Postoperative matters: Follow-up every 3 months after tube placement to observe tube patency, displacement, or dislodgement. The retention time is 12-18 months, with longer retention times considered for younger children or those with multiple recurrences; some tubes may fall out naturally, while those that do not must be removed after the due date. If SOM has not resolved despite tube blockage or premature dislodgement, re-tubing is necessary.
Indications:
Children ≥4 years who meet one of the following conditions are recommended to undergo adenoidectomy concurrently with tympanostomy or tympanic membrane incision:
① Associated with recurrent sinusitis or nasopharyngitis; ② Recurrent SOM; ③ Re-tubing; ④ Other indications for adenoidectomy.
Children under 4 years have poor clinical benefits from adenoidectomy unless they meet operative indications (such as adenoid hypertrophy, obstructive sleep apnea, or sinusitis); surgery is generally not recommended.
Myringotomy can quickly drain tympanic cavity effusion, but it is difficult to perform without pain, and the puncture opening has a short retention time; hence, it is not recommended. Simple myringotomy typically heals in 7-10 days and is not routinely recommended for children with SOM; laser myringotomy can coagulate the edges of the incision, making healing less likely in the short term and can be used selectively.
Should be avoided in conjunction with acute upper respiratory infections, chronic sinusitis, and acute otitis media. Children over 2 years can use a balloon or automatic Eustachian tube balloon dilator with parental assistance for dilation, with follow-up after 2-4 weeks.
Hearing aids may be considered for children with other related diseases whose hearing cannot be improved despite standard treatment, posing a potential risk for speech development; however, they are not recommended for children with isolated SOM.
High-risk children with SOM should be followed up every 1-2 months, while non-high-risk children should be assessed every 3 months.
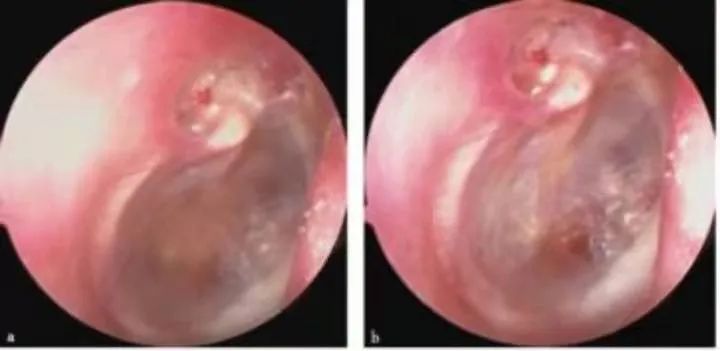
Retracted pocket in the upper tympanic cavity associated with SOM
2. Auditory and Speech Development
SOM primarily leads to conductive hearing loss, but can also involve sensorineural hearing loss, with an average hearing threshold of about 28 dB HL, which can result in unclear speech or age-inappropriate speech errors in children; good family care can mitigate this impact.
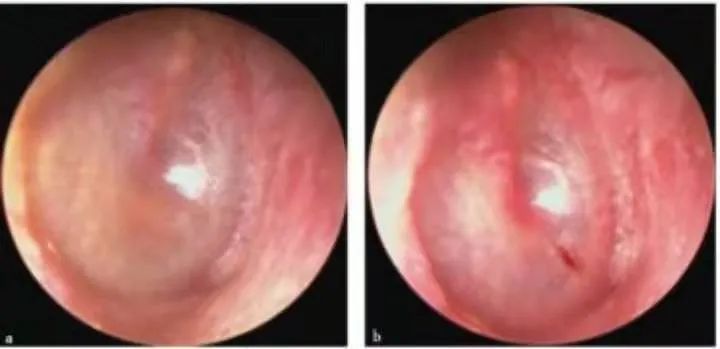
Recurrent SOM after tympanostomy, with healed puncture site and remaining effusion in the tympanic cavity; thin and retracted tympanic membrane with visible tympanic calcification.
3. Vestibular Function
Prolonged SOM may lead to decreased balance ability in children, but balance and motor skills can often return to normal after the middle ear effusion resolves.
4. Behavioral and Learning Abilities
Persistent SOM can lead to sluggish responses, lack of concentration, decreased reading and communication skills, and even an inability to complete tasks and homework independently.
5. Quality of Life
Hearing loss, ear discharge post-tubing, sleep disturbances, behavioral issues, and balance disorders can affect children’s health-related quality of life (HRQL), with the degree of impact related to the severity and frequency of SOM.
The high incidence of SOM in children, diverse causes, insidious onset, prolonged course, and significant harm necessitate active diagnosis and treatment, along with knowledge dissemination to ensure early detection, diagnosis, and rehabilitation.
Inform parents that the occurrence of SOM is related to various factors such as allergic rhinitis, adenoid hypertrophy, upper respiratory infections, air pollution, passive smoking, and pharyngeal reflux; primary diseases should be actively treated to reduce recurrence.
2. Compliance with Follow-Up
Most children can relieve or heal themselves after 3 months of observation, while some require follow-up. Those who have undergone tympanostomy should be informed to avoid getting water in the ear and to have regular follow-ups.
Inform parents that hearing loss can lead to delayed speech development, difficulties in learning and communication, and behavioral abnormalities. During follow-ups, inquire about the treatment process and any changes in hearing, speech, and quality of life, and provide appropriate counseling.
Submission Email:[email protected]
For business cooperation, joining the ENT group, submission communication, etc., please add the WeChat of the ENT assistant: erbihoushikong (note your name and hospital)
Phone: 16655049062