Author: Zhang Jing | Reviewer: Niu Zheng | Editor: Li Dongge
Introduction
Reducing the use of opioids during surgery has been a hot topic in clinical research. Currently, there is no clear tool to monitor the truly appropriate dosage of opioids during general anesthesia. Clinically, hemodynamic parameters such as heart rate and blood pressure changes are often used, but their reliability needs improvement.
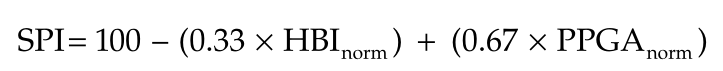
The Surgical Volume Index (SPI) is a parameter calculated based on heart rate and pulse volume waveform, which can serve as a tool to monitor the pain-analgesia balance under general anesthesia.
The basic principle is that stress stimuli trigger peripheral sympathetic system activation, inducing distal vasoconstriction. By measuring the light absorption at the fingertip, the amplitude of the photoplethysmographic pulse wave (PPGA), which reflects the degree of vasoconstriction, can be calculated, thus assessing peripheral sympathetic nerve activity.
Changes in PPGA provide information on peripheral sympathetic contraction. HBI is the heart’s beat-to-beat interval, reflecting central sympathetic tone. By combining PPGA with HBI measurements, the following calculation formula can be obtained through standardization and regression analysis:
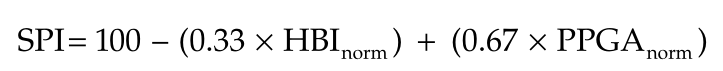
SPI ranges from 0 to 100, with higher values indicating higher stress levels and stronger pain stimuli.
Studies have shown that SPI values between 20 and 50 reflect sufficient analgesic effect. A change in SPI greater than 10 or a value above 50 indicates insufficient analgesia, while a value below 20 indicates excessive analgesia.
However, SPI values are influenced by various factors
-
Patient population: Its application in pediatric anesthesia is still controversial, and it has not been studied in elderly anesthesia.
-
Conscious state: SPI has almost no correlation with pain in awake patients and is only effective in patients under general anesthesia with loss of consciousness.
-
Vasoactive drugs: Won et al. found that the use of the calcium channel blocker nicardipine during surgery would lower SPI values and cannot reflect the surgical stress level.
-
Blood volume: Hans et al. found that patients with low blood volume have a higher likelihood of lower SPI values, and SPI values increase with blood volume.
-
Surgical position: Studies have shown that the lithotomy position significantly lowers SPI values.
Meanwhile, measuring pupil size during surgery has also shown good effects in monitoring pain-analgesia balance.
Pupil dilation reflex (PDR) refers to the increase in pupil diameter in response to pain stimuli. Surgical skin incision or other noxious stimuli can inhibit the oculomotor nerve nucleus, leading to pupil dilation, which can be observed in both awake and anesthetized patients. The degree of pupil dilation is proportional to the intensity of the pain stimulus and inversely proportional to the amount of opioids administered.
The benefits of pupil measurement in clinical practice have yet to be confirmed. Compared to SPI or traditional monitoring, will intraoperative pupil measurement effectively influence opioid consumption and postoperative pain control?
A study conducted by Korean scholars was a prospective, single-center, parallel, double-blind randomized controlled trial comparing the effects of pupil and SPI monitoring on 86 patients from January to May 2019 after obtaining written informed consent.
Methods
Inclusion criteria: ASA I–II, aged 20-65, scheduled for laparoscopic cholecystectomy.
Exclusion criteria: History of ocular diseases (e.g., Adie syndrome, Horner syndrome), neurological or metabolic disease history, history of ocular surgeries, medications interfering with the autonomic nervous system (e.g., β-blockers, anticholinergics), history of substance abuse or psychiatric disorders, chronic pain, or analgesic use within 2 weeks before surgery, and use of pacemakers or arrhythmias.
The patients received no preoperative medications and were monitored for heart rate, non-invasive blood pressure, blood oxygen saturation, neuromuscular blockade, and state entropy (SE) and SPI upon entering the operating room.
Anesthesia was induced with propofol and remifentanil target-controlled infusion pumps, with initial effect-site concentrations (Ce) set at 4µg/mL and 4 ng/mL, respectively. Once the patient lost consciousness, 0.6mg/kg of rocuronium was injected. When the train-of-four (TOF) count reached zero, tracheal intubation was performed for mechanical ventilation. The propofol concentration was adjusted to maintain the SE value between 40 and 60 throughout the surgery.
To facilitate awakening, after carbon dioxide release and beginning suturing, propofol was gradually reduced, allowing the SE target to reach 65. After reversing the muscle relaxant effect, extubation could be performed once the patient opened their eyes on verbal command, resumed spontaneous breathing, and TOF >0.9.
Research Plan
Remifentanil Ce (ng/mL) was managed by grouping from 0.5ng to 5ng, and after tracheal intubation, the remifentanil Ce was lowered to 1.5 ng/mL until the baseline pupil diameter (PD) was reached. In the control group, the remifentanil dosage was determined by the attending anesthesiologist. In the pupil measurement group, the remifentanil Ce was adjusted every 5 minutes based on changes in PD.
If the PD increased by more than 30% compared to the baseline, the remifentanil Ce was increased by 0.5 ng/mL. If the increase remained below 30% or the decrease was within 5% of baseline, the remifentanil Ce remained unchanged. If the PD decreased by more than 5% compared to baseline, the remifentanil Ce was decreased by 0.5 ng/mL.
In the SPI group, the target SPI was set between 20 and 50. If the SPI value exceeded 50, the remifentanil Ce was increased by 0.5 ng/mL. If the value was below 20, it was decreased by 0.5 ng/mL. Once the SPI value increased by more than 10 within one minute, the remifentanil Ce was increased by 0.5 ng/mL. In all groups, the remifentanil infusion rate was gradually reduced after beginning skin suturing and stopped at the end of the surgery.
Pupil measurement was performed using a portable video pupillometer. It non-invasively identifies and tracks the pupil with an infrared camera at 30 frames per second and with an accuracy within 0.03mm. During anesthesia, the average PD measured over 5 seconds guided the remifentanil Ce.
The average PD was measured as baseline about 10 minutes after anesthesia induction (i.e., before skin incision). Subsequently, average PDs were collected during surgical skin incision, laparoscopic insufflation, cannula insertion, and every 5 minutes until the end of surgery.
Measurement
Primary outcome measure was the peak postoperative numerical rating scale (NRS) upon entering the PACU.
Secondary outcome measures included: intraoperative remifentanil consumption rate (μg/kg/min, calculated by dividing the total consumption by patient weight and total infusion time), opioid responsiveness percentage (pain reduction after opioid administration), number of doses administered in PACU according to the predetermined regimen, and the number of patients requiring pethidine administration post-PACU in addition to routine analgesics.
Other outcomes included postoperative complications related to opioid consumption.
After entering PACU, the Riker Sedation-Agitation Scale (RSAS) was assessed every 10 minutes. This study defined “residual sedation” as RSAS <4. When patients became alert, they were asked to rate their pain based on NRS (0=no pain to 10=extreme pain) every 10 minutes after entering PACU. If NRS >4 or the patient required analgesics, 50µg fentanyl (FTN) was administered, and if pain persisted, it was repeated.
If pain control was poor after two consecutive FTN administrations, 30 mg ketorolac was given. For persistent pain resistant to ketorolac, 25 mg pethidine was administered. In the primary study, we assessed FTN responsiveness when NRS decreased by ≥1 within 10 minutes after two remedial FTN administrations.
Postoperative adverse events during PACU were recorded, such as postoperative nausea/vomiting, dizziness, low oxygen saturation (pulse oxygen saturation <90%), itching, bradycardia (heart rate <50 beats/min), and total analgesic consumption. Patients could leave PACU when pain relief was achieved and modified Aldrete score >9, and PACU stay time was recorded.
24 hours postoperatively, we evaluated NRS and adverse events after leaving PACU. Additionally, the number of patients requiring pethidine (25 mg intravenous) in addition to routine analgesics (30 mg ketorolac every 8 hours in the first 24 hours postoperatively) was recorded. Patients were also asked about any intraoperative awareness or recall. All measurements were completed during hospitalization.
Results
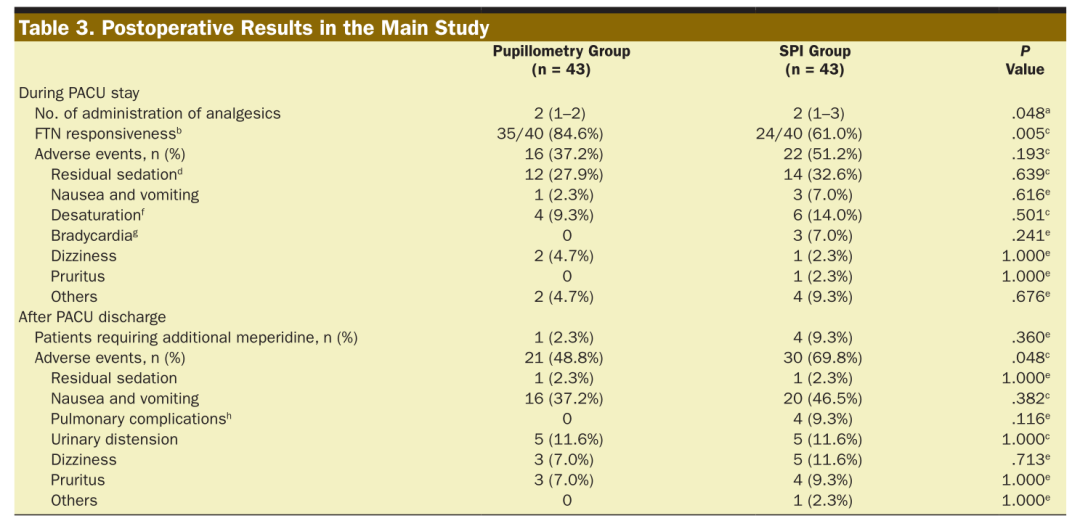
-
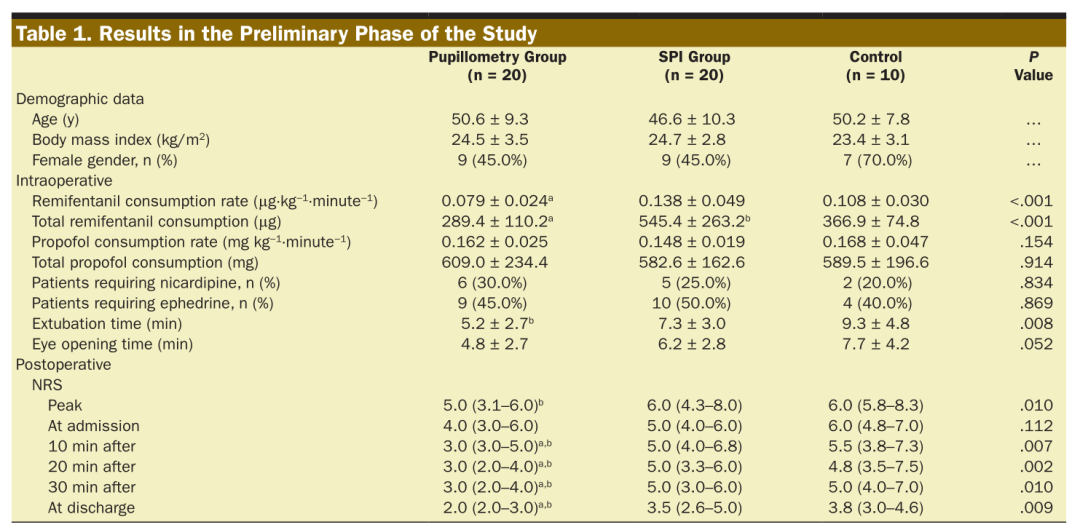
Compared to SPI monitoring, pupil measurement monitoring reduced intraoperative remifentanil consumption, with no observed differences between the pupil measurement group and the control group.
-
The extubation time in the pupil measurement group was earlier than that in the conventional monitoring group, but not earlier than in the SPI monitoring group.
-
The peak NRS score in the pupil measurement group was lower than that in the conventional monitoring group, but there was no difference between the pupil measurement group and the SPI group. (Table 1).
Table 1 Results from the preliminary phase of the study
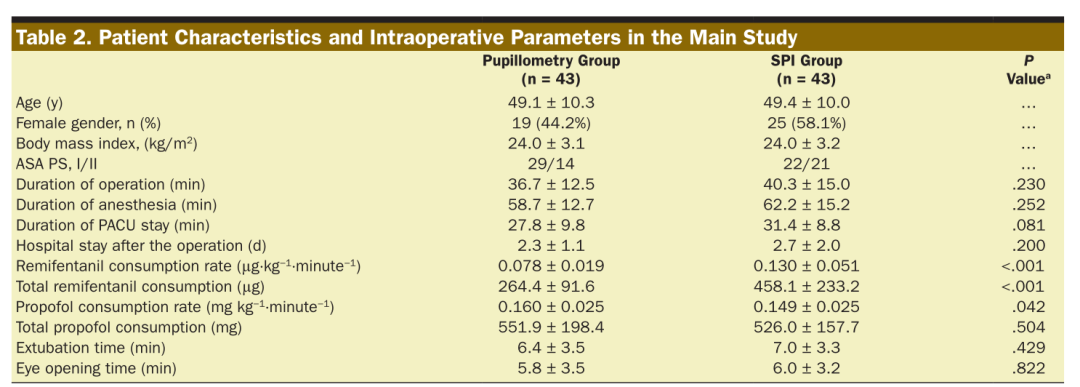
Main study: Among 276 eligible patients assessed, 86 were randomly assigned to each group.
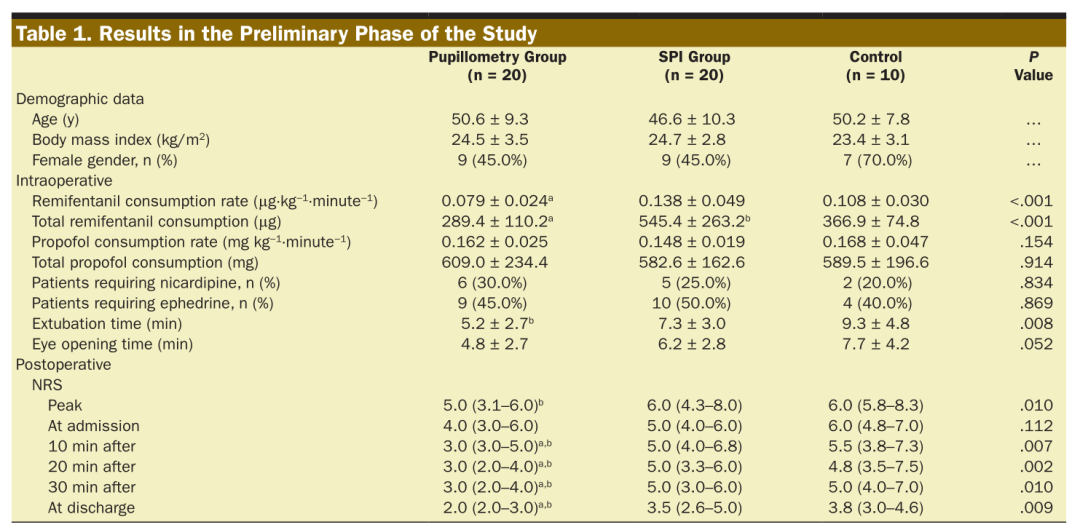
The demographic data of the main study were comparable between the two groups. (Table 2)
Table 2 Patient characteristics and intraoperative parameters in the main study
-
The remifentanil consumption rate in the pupil measurement group was lower than that in the SPI group.
-
During PACU, the NRS scores reported in the pupil measurement group were lower than those in the SPI group.
-
The peak NRS score in the pupil measurement group was lower than that in the SPI group.
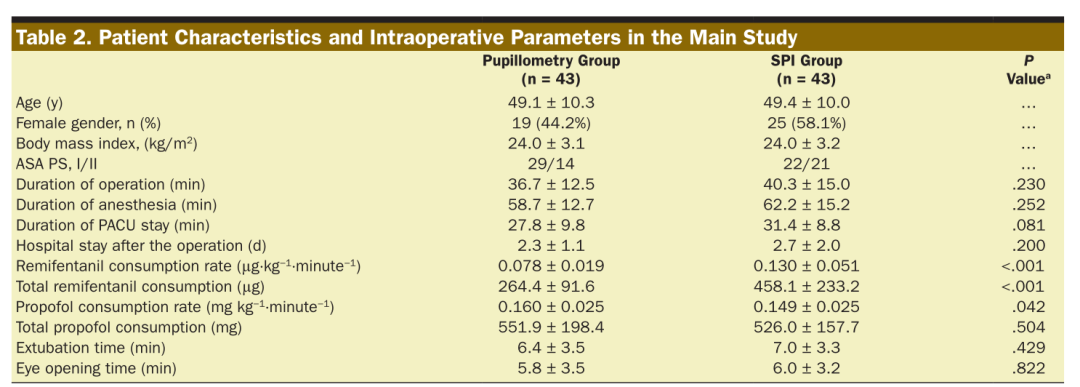
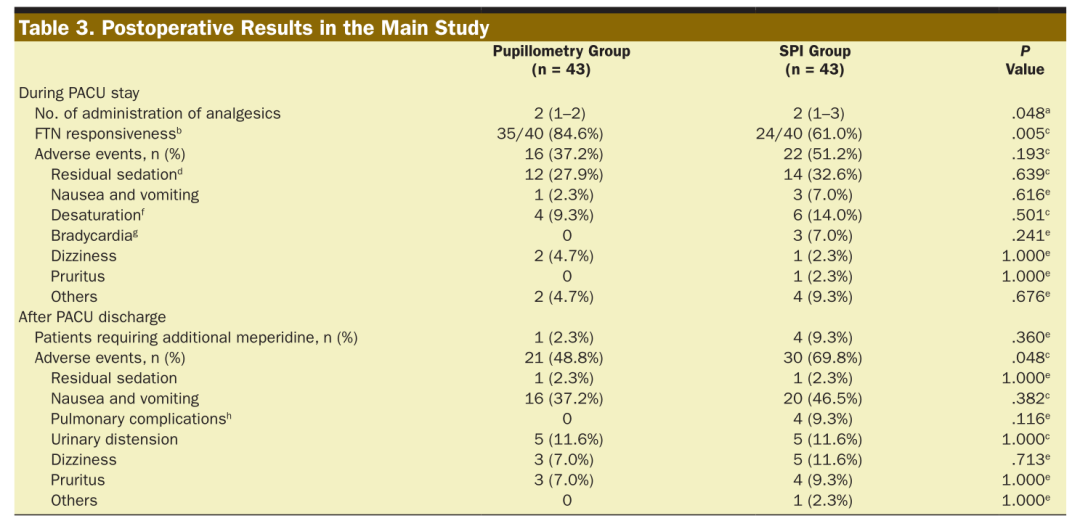
Table 3 Postoperative outcomes of the main study
-
The pupil measurement group required significantly less analgesics compared to the SPI group.
-
FTN responsiveness was higher in the pupil measurement group compared to the SPI group.
Discussion
This study indicates that pupil measurement can reduce intraoperative opioid consumption, postoperative pain, and the number of postoperative analgesic administrations in adults undergoing laparoscopic cholecystectomy compared to SPI monitoring.
Most studies using pupil measurement to assess PDR for pain perception have been conducted under calibrated noxious stimuli. Recently, a study conducted under real surgical stimulation showed that, compared to traditional methods, pupil measurement-guided remifentanil administration performed better; however, their study was limited to gynecological surgeries and did not compare with other monitoring devices.
In this study, the intraoperative remifentanil consumption guided by SPI was higher than that guided by pupil measurement. Possible reasons include:
(1) SPI rapidly increases sympathetic tone with increasing noxious stimuli. However, it decreases slowly with the elimination of the stimulus. Therefore, due to the delayed response of SPI values to the disappearance of noxious stimuli, we may inadvertently overlook reducing the remifentanil infusion rate.
(2) To maintain hemodynamic stability, significant use of vasoactive drugs that affect SPI values was inevitably employed. Although we minimized their use by excluding patients with diabetes, hypertension, and arrhythmias.
(3) Since hypercapnia dilates peripheral vessels, coronary vessels, and cerebral vessels, we speculate that hypercapnia caused by carbon dioxide pneumoperitoneum may affect SPI values. In contrast, PDR during general anesthesia was not influenced by typical doses of vasodilators and vasopressors or circulating catecholamines.
Pupil measurement not only reduced postoperative pain but also improved FTN responsiveness by reducing analgesic use. These results may imply that monitoring via pupil measurement to reduce remifentanil dosage can decrease the occurrence of opioid-induced hyperalgesia.
In conclusion, traditional intraoperative analgesia protocols titrate analgesics based on clinical experience and changes in vital signs. In contrast, pupil measurement is a good alternative.
Compared to SPI, pupil measurement can also reduce intraoperative opioid analgesics, PACU opioid requirements, and pain scores. However, further research in different settings is still needed to confirm and promote the effectiveness of pupil measurement under general anesthesia.