1. Management of SWD
SWD can present as superficial to deep wounds, with exposure of internal organs or implants. The goal of managing SWD is wound healing. Management should be tailored to the specific needs of the patient and requires the involvement and collaboration of the patient, family, nursing staff, and a broader multidisciplinary team. Before formulating a management plan, clinicians must clearly understand the conditions beneath the dehisced wound (such as implants, vital organs, or bone) to ensure proper management and avoid deterioration of the condition or more serious complications.
Principles of SWD Management Include
Soothing the Patient, Managing Expectations, and Education
Pain Management
Elimination or Improvement of Risk Factors that May CauseSWD or Affect Healing
Management of Systemic Infections
Local Treatment of Wound Dehiscence, Including Management of Local Infections
The treatment goals and management plans should be thoroughly documented and discussed with the patient, nursing staff, and family.
1. Soothing the Patient, Managing Expectations, and Education
Even small wounds can be frightening for patients. Physicians need to address concerns based on the patient’s needs, explaining the condition to alleviate their worries, such as the causes of SWD, the measures to be taken, and the expected recovery. Encourage patients to express their concerns and facilitate conversations between SWD patients and those with similar experiences, as this measure is effective.
Education forSWD Patients Should Include Signs and Symptoms of Infection (If Not Yet Present), How to Avoid Applying Extra Pressure on the Wound, Recommendations on Activity Levels, Guidance on How to Handle Worsening Wounds or Conditions, and Whom to Contact.
2. Pain Management
Pain management should include the causes of pain, as well as pain related to dressing changes and debridement. Both pharmacological and non-pharmacological measures should be considered, including education and dressing selection, frequency of dressing changes, and techniques to minimize pain and trauma. The World Health Organization’s three-step analgesic ladder for adult cancer pain may be applied to pain management in other situations and can appropriately guide pharmacological treatment.
3. Management of Comorbidities and Pathogenic Factors
Any factors that may lead to SWD or hinder healing, such as chest infections, poor blood sugar control in diabetic patients, smoking, and malnutrition, should be addressed.
4. Management of Systemic Infections
In the presence of symptoms and signs of SSI, or if erythema extends more than 5 cm from the incision accompanied by induration or necrosis, systemic antibiotic therapy should be initiated. The choice of antibiotics should be based on the location of the incision, local antibiotic policies, bacterial resistance, and microbiological analysis results.
For SWD Patients with Only Local Signs and Symptoms of Infection, Systemic Antibiotics Are Generally Not Recommended. However, If Infection Occurs Within the Incision, and This Incision is Critical for Preventing the Spread of Infection, Systemic Antibiotics May Be Necessary Due to Potential Severe Consequences (e.g., sternotomy).
5. Management of Local Infections
According to SSI management guidelines, residual sutures and clips in partially dehisced wounds should be removed from areas with signs and symptoms of infection (including abscess). Care should be taken when removing sutures and clips, as this may exacerbate the dehiscence or create new SWD. Removal of sutures should be performed by qualified clinicians in a medical environment to manage any potential expansion of the dehisced wound.
Local Antimicrobials
Local antimicrobials play two primary roles in the management of SWD:
■ Management of Local Infections
■ Prevention of Infection in SWD Patients at High Risk.
Many antimicrobials are available for wounds, including iodine, silver, and polyhexamethylene biguanide (PHMB). Antimicrobials come in various forms, including antimicrobial-impregnated dressings (e.g., flat, ribbon, or strips), ointments, gels, powders, and washes. The ideal characteristics of antimicrobial dressings include rapid and sustained release of antimicrobials into the wound environment for quick onset and sustained bactericidal activity.
Two-Week Challenge
Local antimicrobials should not be used indefinitely. If monitoring shows no specific issues, the use of antimicrobials should be reassessed after two weeks. If the condition of SWD improves after two weeks, the use of antimicrobials should be discontinued. If there is no improvement in SWD, the patient and wound should be re-evaluated, and consideration should be given to changing medications to address challenges in the next two weeks.
Define Management Goals
-
Involve Patients and Other Healthcare Professionals
-
Comprehensive Management
Soothing the Patient; Managing Expectations and Educating Patients, Families, and Nursing Staff; Pain Management; Management of Pathogenic Factors and Comorbidities
Local Management
1. Wound Closure — Convenient, Most Appropriate Mode;
2. Drainage of Abscess, Seroma, or Hematoma;
3. Use Appropriate Methods to Remove Non-viable or Necrotic Tissue Within the Clinician’s Skill Set;
4. Perform Appropriate Cleaning According to Local Policies;
5. During Cleaning, Select Dressings and Materials Based on Wound Exudate Volume and Depth to Promote Moist Wound Healing and Ensure Dead Space is Eliminated to Reduce Infection Risk;
6. Manage Local/Systemic Infections;
7. Control Lower Limb Incision Edema
Monitoring and Reevaluation
-
Monitor for Infection at All Times
-
Monitor Conditions During Each Dressing/Device Change
-
Conduct Regular Comprehensive Reevaluations Based on Wound Condition, Type of Surgery, Location of Incision, and Monitoring Conditions. Infected SWD may require early reevaluation. Non-infected SWD should receive comprehensive reevaluation every four weeks.
-
If Healing Does Not Progress as Expected or if the Wound is Worsening, Reevaluation Should Be Conducted, and Referrals Made as Needed, Such as to Surgical Departments.
Local Management of SWD
Local management of SWD depends on the following factors:
-
The Severity of Dehiscence, such as Depth and SWD Grading, and Exposure of Internal Organs, Bones, or Implants
-
Presence of Infection
-
Time Since Surgical-Related Incision Dehiscence
-
Occurrence of Complications that May Increase the Risk of Surgical Site Complications or Affect Healing
The results of the overall assessment will indicate appropriate treatment goals and guide management planning; the TIME principles can guide local management of wound dehiscence while considering the removal of devitalized tissue (debridement), controlling infection, controlling exudate, and promoting moist wound healing.
2. Management of SWD by Grade
|
Assessment, Management Goals, Systemic Management, Local Management |
||||
|
Outpatient/Social Environment |
||||
|
Hospital Environment |
||||
|
No Clinical Signs or Symptoms of Infection |
||||
|
Grade |
1 |
2 |
3 |
4 |
|
Closure Method |
Usually Secondary Closure |
Usually Secondary Closure |
Usually Secondary Closure; If Contaminated/Healing Issues, Consider Delayed Primary Closure; or with Flaps, Skin Grafts/Dermal Matrix Replacements |
Usually Secondary Closure; If Contaminated/Healing Issues, Consider Delayed Primary Closure; or with Flaps, Skin Grafts/Dermal Matrix Replacements |
|
Debridement |
If Needed, Often Choose Autolytic Debridement |
Often Autolytic Debridement; +/- If There is a Large Amount of Devitalized Tissue, Other Debridement Methods May Be Used
|
Sharp Debridement/Surgical Debridement to Remove Necrotic Tissue
|
Surgical Debridement to Remove Necrotic/Non-viable Tissue +/- Irrigation |
|
Local Management |
■Use Dressings to Manage Exudate Levels, Wound Surrounding Skin Condition, While Meeting the Purpose of Autolytic Debridement ■If the Patient is at Risk for Delayed Healing, Consider Using NPWT |
■Use Dressings to Manage Exudate Levels, Wound Surrounding Skin Condition, While Meeting the Purpose of Autolytic Debridement ■ If the Patient has High Exudate or is at Risk for Delayed Healing, Consider Using NPWT, Selecting Devices and Fillers for Wound Contact Layers Based on Wound Exudate Levels and Depth |
■Use Dressings to Manage Exudate Levels, Wound Surrounding Skin Condition, While Meeting the Purpose of Autolytic Debridement ■ If the Patient has High Exudate or is at Risk for Delayed Healing, Consider Using NPWT, Selecting Devices and Fillers for Wound Contact Layers Based on Wound Exudate Levels and Depth
|
■ +/- Surgical Management of Internal Organs, Bones, or Implants ■ Consider NPWT Wound Fillers +/- Prophylactic Antimicrobial Interfaces +/- Irrigation |
|
Clinical Symptoms or Signs of Infection |
||||
|
Grade 1a ■ Include All Measures for Grade 1 Wounds Above Control Local Infection: Use Antimicrobial Dressings According to Best Practice Guidelines and Local Regulations ■ Promptly Address Systemic Infections if Present |
Grade 2a Include All Measures for Grade 2 Wounds Above ■ Manage Local Infection: Use Antimicrobial Agents According to Best Practice Guidelines and Local Regulations ■ If Using NPWT, Consider Antimicrobial Interfaces According to Local Requirements ■ Promptly Address Systemic Infections if Present |
Grade 3a Include All Measures for Grade 3 Wounds Above ■ If Using NPWT, Consider Antimicrobial Interfaces According to Local Requirements ■ Promptly Address Systemic Infections if Present |
Grade 4a Include All Measures for Grade 4 Wounds Above ■ +/- If There is Persistent Infection Source, Surgical Management of Internal Organs, Bones, or Implants, ■ If Using NPWT, Consider Antimicrobial Interfaces +/- Infusion/Irrigation ■ Promptly Address Systemic Infections if Present |
If SWD Occurs Within 48 Hours Post-Surgery Due to Surgical Technique, Primary Closure Should Be Performed if There Are No Other Contraindications;
Dermal Matrix/Substitutes Should Not Be Used in the Presence of Wound Infection;
Manage Systemic Infections According to Best Practice Guidelines, Considering Local Policies, Microbiological Culture Results, and Sensitivity Reports;
3. Closure Methods
Selecting the Most Appropriate Method for Wound Closure is an Important Initial Decision in Managing SWD. This Depends Largely on How Soon SWD Occurs Post-Surgery, the Depth of Dehiscence (i.e., WUSWH SWD Grade), the Location of the Incision, and Whether Infection is Present.
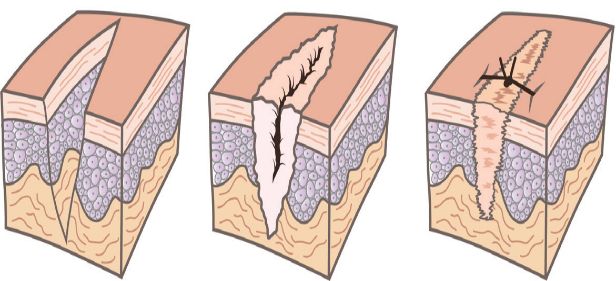
Primary Closure
Primary Closure After SWD Can Be Reflected in the Following Aspects:
-
SWD Occurs Within 48 Hours Post-Surgery, Clearly Due to Surgical Technique, Such as Suture Breakage, Clips Not Properly Placed
-
No Other Issues Leading to the Wound, i.e., No Excessive Tension on the Incision, and No Signs of Infection
-
The Patient is Not at Increased Risk of Complications at the Surgical Site
Secondary Closure
Secondary Closure is Commonly Used for Superficial SWD, with or without Infection. For Example, WUWHS Grades 1, 1a, 2, and 2a. Secondary Closure May Also Be Used for Deeper Dehiscence, Such as Grades 3 and 3a, Occasionally for Grade 4 and 4a with High SSI Risk or Infection, or for Wounds That Cannot Be Closed Primarily Due to Tissue Loss.
Delayed Primary Closure
Delayed Primary Closure (Figure 12), Sometimes Referred to as Tertiary Intention Healing, is Primarily Used for Deeper SWD, Such as WUWHS Grades 3, 3a, 4, and 4a, Where Contamination or Infection is Present, or Where Complications or Subcutaneous/Organ Swelling May Place Tension on the Closure, Increasing the Risk of Recurrence. When Primary Closure is Appropriate, If Tissue Deficiency Still Exists, Flaps or Grafts May Be Used.
Primary Closure
The Edges of the Incision Are Closely Apposed, For Example, by Sutures, Staples, or Adhesives to Achieve Primary Healing
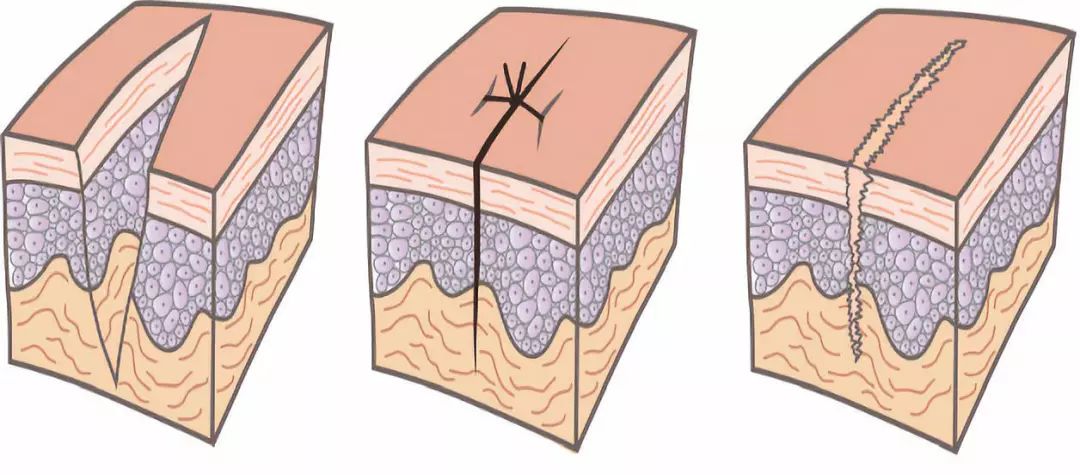
Secondary Closure
The Incision is Open, Healing Through New Tissue Filling from the Bottom and Sides of the Wound
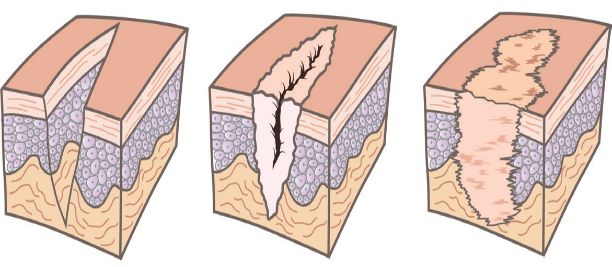
Delayed Primary Closure
To Treat Infection or Remove Contamination (If Necessary in Sequence) Remove Non-viable Tissue or Eliminate Swelling, the Incision Should Remain Open for Several Days or Weeks Before Primary Closure or Flap Use.
Management of Abscesses, Seromas, and Hematomas
Accumulation of Fluid Under Closed Incisions, Whether Pus, Serous Fluid, or Blood, May Increase Tension on the Incision, Increasing the Risk of SWD. Abscesses Should Be Drained to Remove Pus and Eliminate Potential Infection Risks. Seromas and Hematomas May Resolve Spontaneously; However, Depending on Their Size, Location, and Impact on the Incision, They May Require Aspiration or Drainage Tube Insertion.
4. Debridement
Necrotic, Non-viable Tissue and Foreign Bodies in Dehisced Incisions Serve as a Culture Medium for Bacterial Growth and Biofilm Formation, Increasing the Risk of Infection and Healing Impairment. The Presence of Biofilm in the Incision May Be Associated with 80% of SSIs.
Debridement Removes Non-viable Tissue and Foreign Bodies, Reducing Bio-burden, Biofilm, and Inflammatory Stimuli. Especially in Sharp or Surgical Debridement, Debridement Also Stimulates the Release of Growth Factors to Promote Healing.
There Are Several Methods of Debridement. Clinicians Should Work Within Their Skill Set When Performing Debridement, Referring Patients to Surgeons for Methods Beyond Their Skill Set.
Autolytic Debridement is Usually Sufficient for Grade 1/1a and 2/2a Dehisced Wounds. For Grades 3/3a and 4/4a Incisions, Sharp or Surgical Debridement May Be Most Appropriate.
|
Several Main Debridement Techniques for Dehisced Wounds |
|
|
Technique |
Description and Explanation |
|
Autolytic Debridement |
■ Softens and Liquefies Devitalized Tissue Through Enzymes Naturally Produced in the Wound ■ Creates a Moist Healing Environment Through Dressings ■ Selective, Non-invasive Procedure ■ Can Be Used Before or Between Other Debridement Methods |
|
Mechanical Debridement |
■ Wet to Dry Dressing: Apply Wet Gauze Pads to the Wound. When It Dries, Devitalized Tissue Adheres to the Gauze, Removed with the Gauze ■ Monofilament Pad or Debridement Cloth: Use Force to Clean the Wound, Separating and Removing Devitalized Tissue; Can Be Used in Combination with Autolytic Debridement |
|
Sharp Debridement |
■ Removal of Necrotic Tissue with Surgical Scissors, Scalpels, or Forceps ■ Quick, Selective ■ Requires Specialized Training; May Require Local Anesthesia |
|
Surgical Debridement |
■ Surgical Removal of Non-viable Tissue from the Wound Edges to Restore Health ■ Selective ■ Requires Specialized Training; May Require General Anesthesia and an Operating Room |
|
Maggot Debridement |
■ Placement of Cultured Green Bottle Fly Larvae (Lucilia sericata) in the Wound to Ingest Devitalized Tissue and Bacteria ■ Selective |
|
Ultrasound Debridement |
■ Ultrasonic Energy is Used to Disrupt Devitalized Tissue; Debris is Flushed Away by an Integrated Irrigation System ■ Quick, Selective ■ Requires Specialized Training |
|
Water Jet Debridement |
■ High-Pressure Saline Jet is Used to Remove Necrotic Tissue ■ Quick, Relatively Selective ■ Requires Specialized Training |
Factors Influencing the Selection of Local Antimicrobials
■ Allergies/Sensitivities
■ Antimicrobials Used for Current Wound Management
■ Length, Width, and Depth of the Wound
■ Used in Conjunction with Other Devices, Such as Negative Pressure Wound Therapy (NPWT)
■ Exudate Levels
■ Condition of Surrounding Skin
■ Expected Frequency of Dressing Changes
■ Availability
■ Cost
5. Cleaning
The Purpose of Wound Cleaning is to Remove Loose Debris, Dirt, Microorganisms, and Residues from Previous Dressings from the Wound and Surrounding Skin. The Choice of Cleaners Should Be Guided by Local Policies. Cleaners Include Drinking Water (e.g., Water Safe for Drinking) or Sterile Saline.
If the Wound is Infected, Consider Using Antimicrobial Irrigation Solutions for Cleaning. However, the Role of Antimicrobial Irrigation Solutions in the Management of Infected Wounds Has Not Been Fully Elucidated.
6. Moist Wound Healing and Exudate Management
Dressings for SWD Need to
■ Maintain a Moist Environment for Wound Healing While Absorbing Excess Exudate, which Can Serve as a Medium for Bacterial Growth or Cause Periwound Maceration
■ Protect the Dehisced Wound from External Contamination and Further Microbial Invasion
As Mentioned Above, Dressings Can Also Serve as Carriers for Local Antimicrobials or as Means to Promote Autolytic Debridement. The Selected Dressings Should Have Sufficient Absorbency to Maintain a Moist Environment for the Wound, Not Leak or Cause Damage to the Surrounding Skin, and Allow for Appropriate Intervals Between Dressing Changes. Ideally, the Frequency of Dressing Changes Should Align with the Need for Wound Monitoring: Infected Wounds Require More Frequent Monitoring Than Non-infected Wounds, Thus May Require More Frequent Dressing Changes. The Performance of Individual Dressings is Influenced by the Materials and Quantity of the Dressings Used. Therefore, It Is Difficult to Generalize the Absorbency and Capacity to Handle Exudate of Different Dressings. To Address This Issue, Dressings Are Often Combined with Different Types of Materials. Generally, Dressings Containing Foam, Alginate, or Carboxymethylcellulose Are Suitable for Moderate to High Exudate Wound Management.
The Performance of Individual Dressings is Highly Dependent on Their Structure and Composition Materials
It is Important to Remove Exudate from Dehisced Wounds’ Dead Space, as Exudate in Dead Space Can Increase the Risk of Infection. WUWHS Grades 2 and 3 Wounds Use Dressings, Which Need to Be Selected Based on Exudate Levels (e.g., Linear, Ribbon, Strip, or Paste) for Filling. Two-layer Dressings are Necessary to Keep the Dressings in Place. For Grade 4 Dehisced Wounds, Simply Using Dressings May Not Be Enough, at Least in the Early Treatment Phase.
Selecting Dressings Should Align with the Amount of Exudate at the Dehisced Wound, the Depth of the Wound, and the Expected Frequency of Dressing Changes.
7. Negative Pressure Wound Therapy
Negative Pressure Wound Therapy (NPWT) is Particularly Suitable for High Exudate, Deep, or Complex Dehisced Wounds. NPWT Can Promote Moist Wound Healing, Manage Exudate/Secretions, Remove Dead Space, and Prevent External Contamination to Facilitate Secondary or Tertiary Healing of Dehisced Wounds.
For Over 20 Years, NPWT Has Been Widely Used to Manage Various Acute and Chronic Wounds. Based on Extensive Evidence and Clinical Experience, NPWT is Recommended as the “Gold Standard” for Treating Open Abdominal Wounds and Dehisced Sternotomy Wounds.
A Large Number of Studies Have Investigated the Use of NPWT on Infected Surgical Wounds (Including Patients with and without SWD), Focusing Primarily on the Role of NPWT in SWD, Including:
■ Abdominal Incisional Dehiscence
■ Dehiscence After Sternotomy
■ Dehiscence After Cesarean Section
■ Perineal Dehiscence
■ Dehiscence After Amputation
■ Dehiscence After Vascular Surgery
■ Dehiscence After Spinal Surgery
References
1.Tarzia V, Carrozzini M,Bortolussi G, et al. Impact of vacuum-assisted closure on
outcomes of sternal wound dehiscence. InteractiveCardiothor Thorac Surg 2014;
19: 70–75.
2.International Wound InfectionInstitute (IWII). Wound infection in clinical practice.
Wound International, 2016. Available at:www.woundsinternational.com
3.Limongelli P, Casalino G,Tolone S, et al. Quality of life and scar evolution after
negative pressure or conventional therapy for wounddehiscence following post-
bariatric abdominoplasty. Int Wound J 2017; doi:10.1111/iwj.12739.
4.World Union of Wound HealingSocieties (WUWHS). Principles of best practice:
wound infection in clinical practice. An internationalconsensus. London: MEP Ltd,
5.Available at: www.woundsinternational.com
6.Schultz GS, Brillo DJ, MozingoDW, et al. Wound bed preparation and a brief
history of TIME. Int Wound J 2004; 1(1): 19–32.
7.World Union of Wound HealingSocieties (WUWHS). Principles of best practice: Wound exudate and the role ofdressings. A consensus document. London: MEP Ltd,
8.Stevens DL, Bisno AL, ChambersHF, et al. Practice guidelines for the diagnosis
and management of skin and soft tissue infections: 2014update by the Infectious
Disease Society of America. Clin Infect Dis 2014; 59; e10.
9.WUWHS. Principles of bestpractice: minimising pain at wound dressing-related
procedures. A consensus document. London: MEP Ltd, 2004.
10.Richardson C. An introductionto the biopsychosocial complexities of managing
wound pain. J Wound Care 2012; 21(6): 267–73.
11.Edmiston CE, McBain AJ, KiernanM, Leaper DJ. A narrative review of microbial
biofilm in postoperative surgical site infections: clinicalpresentation and
treatment. J Wound Care 2016; 25(12): 693–702.
12.Effective debridement in achanging NHS: a UK consensus. London: Wounds UK,
13.Available at: www.wounds-uk.com
14.Atkin L. Understanding methodsof wound debridement. Br J Nurs 2014; 23(12):
S10–15.
15.Wolcott R, Fletcher J. The roleof wound cleansing in the management of wounds.
Wounds Int 2014; 1(1): 25–31.
16.Fernandez R, Griffiths R. Waterfor wound cleansing. Cochrane Database Syst Rev
2012; 15(2): CD003861.
17.Weiss EA, Oldham G, Lin M, etal. Water is a safe and effective alternative to
sterile normal saline for wound irrigation prior tosuturing: a prospective, double-
blind, randomised, controlled clinical trial. BMJ Open2013; 3: e001504.
18.National Institute for Healthand Care Excellence (NICE). Surgical site infections:
prevention and treatment. NICE, 2008; updated February2017.
19.Wounds UK Best practicestatement. The use of topical antimicrobial agents in
wound management. London: Wounds UK, 2013. Available at:www.wounds-uk.
com
20.Lipsky BA, Hoey C. Topicalantimicrobial therapy for treating chronic wounds. Clin
Infect Dis 2009; 49: 1541–49.
21.Bovill E, Banwell PE, Teot L,et al. Topical negative pressure wound therapy: a review of its role andguidelines for its use in the management of acute wounds.