SWD can occur at any time post-surgery, from 1 day to over 20 days after the operation, but generally occurs between the 4th and 14th postoperative days.
Possible Signs of SWD
SWD can occur without any signs. Incisions at risk of dehiscence may show signs of inflammation that exceed the normal healing time and range, such as increased redness, swelling, heat, and pain at the incision site after 5 days postoperative. Palpation of the incision and surrounding area may reveal increased skin temperature and a fluctuating sensation (subcutaneous fluid collection, hematoma, or abscess). A sudden increase in pain or fluid drainage from the incision may indicate SWD.
Signs of inflammation at the incision site, such as fever, erythema, edema, and pain, are normal in the first few days post-surgery and do not necessarily indicate infection.
|
Characteristics of Good vs. Impaired Wound Healing |
|||
|
Indicators |
Link to TIME Principles |
Signs of Good Healing |
Signs of Impaired Healing |
|
Incision Color |
Tissue |
Days 1-4: Red; Days 5-14: Pinkish-white; Days 15-30: Light pink, white or silvery in darker-skinned patients; |
Days 1-4: May be red, with tension at the incision line; Days 5-9: Edges may be well-approximated, with persistent tension; Days 10-14: If no SWD occurs, remains red or progresses to pink, ultimately forming hypertrophic scars; |
|
Healing Ridge |
Days 5-9: A thickened tissue healing ridge may be felt, indicating newly formed collagen, extending about 1 cm along the length of the incision until the remodeling phase |
No healing ridge |
|
|
Surrounding Area of the Incision |
Infection/Inflammation |
Signs of inflammation: – Day 5: Mild edema, erythema, fever, or skin discoloration; – Pain; |
No signs of inflammation in the first few days post-surgery; Signs of prolonged inflammation and persistent pain; |
|
Exudate |
Moisture |
Days 1-4: Exudate volume decreases from moderate to minimal, changing from sanguineous (blood-stained) to serosanguineous (mix of blood and serum) to serous (clear amber serum) – Appears on day 5 |
Exudate persists beyond days 1-4 post-surgery; Exudate may be serosanguineous, serous, or purulent (e.g., cloudy, green, yellow, or brown) |
|
Wound Edges |
Edges |
By day 4, long skin closure is visible along the entire incision |
Epithelium may be only partially present or completely absent; SWD may occur within 14 days post-surgery; |
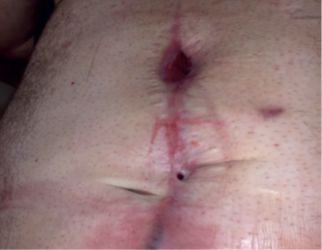
Signs of SWD
Separation of the wound edges may present as small pinprick-like to larger gaps, potentially involving the entire length and depth of the incision. If the incision communicates with a body cavity, SWD may lead to exposure of internal organs. Suture materials may be visible in the separated area and may also break.
In patients with abdominal or sternotomy incisions, wound dehiscence may occur after nausea, vomiting, or coughing. Patients may describe a pulling or tearing sensation in the wound area.
A patient with a surgical incision at increased risk for SWD or who has experienced dehiscence may exhibit local and systemic signs and symptoms of infection.
|
Local Clinical Symptoms and Signs of Closed Surgical Wound Infection |
|
–Local erythema or spreading(cellulitis) –Purulent or serous exudate –Abscess –Swelling/induration –Increased skin temperature –Foul odor –Crepitus –Dehiscence –Sudden pain or tenderness |
|
Systemic Signs and Symptoms Possibly Related to Closed or Dehisced Surgical Wound |
|
–Discomfort –Anorexia –Hypothermia –Tachycardia –Tachypnea – cElevated reactive protein –Elevated or decreased white blood cell count –Sepsis –Septic shock |
Incision/Wound Assessment
Before assessing SWD, it is essential to identify the event that led to the dehiscence, such as coughing, vomiting, trauma, or removal of sutures/staples, and determine the timing of the dehiscence; those occurring shortly after surgery and recent SWD may be suitable for re-suturing.
The entire length of the incision with SWD should be thoroughly assessed, as factors leading to SWD may affect other closed incisions.
The core expert working group recommends using a structured framework, such as the TIME principles, to assist in SWD assessment. Sequential photographs can aid in monitoring healing. Photography should be conducted with patient consent and in accordance with local policies.
If there is more than one dehisced wound, each should be assessed individually.
Multiple Dehisced Wounds
A shorter dehisced area may not only be superficial but may also affect deeper tissues.
While determining the depth of the dehisced area is important, any probing should be performed with caution by a qualified clinician to avoid inadvertently worsening the dehiscence or causing other damage.
All systemic and local wound assessments, further investigations, interventions, and referrals should be documented.
|
Overall Assessment of SWD |
|
Risk Factors for SWD |
|
Medical and Surgical History, including: |
|
Previous wound healing issues, such as SWD, SSI -Radiation therapy -Chemotherapy -Allergies and sensitivities to medications and skin/wound products |
|
Procedural Factors Leading to Incision Dehiscence, including: |
|
–Surgical reasons and dates –Emergency surgery/elective surgery –Intraoperative and postoperative complications – such as bleeding, hypothermia, prolonged surgery, SSI –Method of incision closure –Timing of suture removal |
|
Current Health Status, including: |
|
–Need for hemodynamic or respiratory support –Active comorbidities – such as diabetes, obesity, COPD, coagulation factor deficiencies, anemia/transfusion, cough/chest infections, constipation, skin diseases |
|
Lifestyle Factors, including smoking, drinking, diet, exercise, etc. |
|
Current Medications and Reasons for Use, including: |
|
–Anticoagulant, antiplatelet therapy –Long-term corticosteroids –Immunosuppressants –Antibiotics –Analgesics |
|
Pain, including severity of pain at the site; whether related to the wound; use of numerical or visual analog scales can objectively assess and monitor pain severity; current pain management strategies |
|
Mental State, including: |
|
Care environment Family/caregiver support –Occupational and financial status –Patient’s understanding and attitude towards their condition and the incision and surgery –Ability and willingness to engage in self-care –Impact of the wound on quality of life (physical, social, and emotional) |
|
Using TIME Principles to Assess SWD |
||
|
Indicators |
Assessment |
Characteristics |
|
Tissue |
Location and extent of dehiscence |
Location of incision Extent of affected incision Number of dehisced incisions Condition of sutures, etc. (intact or broken) |
|
Depth of Dehiscence |
Partial thickness or full thickness Affected tissues Exposure of organs/bones/implants Sinus or tract Exposure of viscera in abdominal SWD |
|
|
Tissue Vitality |
Condition of exposed tissues Type and proportion of wound bed tissue – e.g., necrotic tissue, slough, and granulation tissue |
|
|
Size |
Dimensions of dehiscence: maximum length, width, depth |
|
|
Infection or Inflammation |
Local infection or inflammation |
Clinical symptoms and signs Signs of acute and chronic infection In immunocompromised patients, signs and symptoms of infection may be less pronounced |
|
Moisture Level |
Color, viscosity, type, and odor of exudate |
Purulent (creamy, yellow, or green) or sanguineous (red, brown) may indicate infection Yellow or brown exudate may suggest a fistula or sinus Odor may suggest infection or sinus tract |
|
Level of Exudate |
Exudate level can be determined from the dressing condition and the appearance of the wound bed (i.e., dry dressing indicates low secretion; saturated or leaking dressing indicates high exudate volume) |
|
|
Edges |
Edges of dehisced wounds |
Long-standing dehisced wounds may have undermining underneath the edges |
|
Color and condition of skin surrounding the dehisced wound |
Skin conditions that may affect healing, such as radiation dermatitis Signs of infection spread, such as spreading erythema, fever, and edema Moisture around the wound may indicate high exudate/drainage levels and/or low absorption of exudate by the dressing |
The diagnosis of infection in a surgical incision or dehisced wound is primarily based on local and systemic signs and symptoms. Fever within 48 hours post-surgery is unlikely to be caused by SSI.
The role of sampling and microbial culture in diagnosing SSI remains controversial. Reasons include that surface sampling may only reflect the presence of bacteria on the surface rather than deep tissue, which is highly relevant to deep surgical incisions.
Advancements in technology, such as the use of point-of-care fluorescence imaging to detect bacterial levels in thickened tissue areas and guide sampling, can help improve the effectiveness of microbial sampling.
Clinicians should be aware of the limitations of microbiological analysis of wound samples and interpret results in conjunction with clinical signs and symptoms, noting that a “negative” swab does not necessarily indicate no infection.
Most patients with SWD do not require further imaging diagnostic tests. However, if there is uncertainty about the diagnosis, depth of dehiscence, or if the extent of dehiscence worsens or does not improve despite treatment, imaging studies may be considered.
In many cases, ultrasound will be the most appropriate imaging modality, while more expensive options, such as MRI, may be reserved for further research. Imaging can be used not only to assess tissue but also to detect and evaluate seromas, hematomas, and purulent fluid, and to assess the proximity of dehisced wounds to implants, such as prosthetic joints.
Classification of SWD
Classification of SWD is often related to specific types of surgical procedures, such as thoracic or abdominal surgeries. Some classifications are adapted from adverse event reporting systems, such as the Ottawa Thoracic Morbidity and Mortality system.
A classification system that is applicable to all types of surgery, easy to use, suitable for all care settings (including community), capable of representing severity, and guiding appropriate management strategies is needed.
The WUWHS SWD scoring system was proposed by the core expert working group during consensus meetings, referencing the Sandy SWD scoring system. This system considers wound depth and the presence of infection as primary factors in assessing the severity of SWD. The purpose of distinguishing between symptomatic and asymptomatic SWD is to emphasize different treatment approaches. The WUWHS SWD scoring system should only be applied after a comprehensive assessment of the patient and surgical incision, and sometimes requires probing by a qualified clinician to explore the dehisced area. Although most SWD occurs between 4-14 days post-surgery, the scoring system includes a 30-day period. This is to encourage monitoring of SWD after discharge, as with SSI, SWD may be underreported due to patient discharge. The 30-day timeframe roughly aligns with SSI reporting requirements and has been applied to all SWD classifications to ensure consistency. As awareness of SWD increases, the timeframe may need to be adjusted.
Since SWD generally occurs between 4 to 14 days post-surgery, most patients may experience SWD after discharge. Regardless of how long the incision has been dehisced, SWD involving deeper layers of the incision is more severe than those involving multiple superficial layers.
|
WUWHS Classification |
Description |
|
|
Severity
Increase
|
1 |
Involves only the dermis; no visible subcutaneous fat; no signs and symptoms of infection |
|
1a |
Grade 1 with clinical signs and symptoms of infection |
|
|
2 |
Subcutaneous tissue exposed; fascia not visible; no signs and symptoms of infection |
|
|
2a |
Grade 2 with clinical signs and symptoms of infection |
|
|
3 |
Subcutaneous layer and fascia exposed; no signs and symptoms of infection |
|
|
3a |
Grade 3 with clinical signs and symptoms of infection |
|
|
4 |
Fascia dehisced incision with exposure of organs, viscera, implants, or bone; no signs and symptoms of infection |
|
|
4a |
Grade 4 with clinical signs and symptoms of infection |
|
|
Scoring should be conducted after thorough assessment, including probing of the affected area at the discretion of a qualified clinician; If more than one separation occurs, grading should be based on the deepest separation; Grade 4 or 4a dehisced abdominal incisions are also referred to as “burst abdomen”. |
Source: Ostomy Wound Management Microcommunity


 Join the WeChat group of nurses classified by department, please click on the “Read the original text” below.
Join the WeChat group of nurses classified by department, please click on the “Read the original text” below.