Skip to content
Pediatric epilepsy specialist Dr. Dave Clarke aims to better diagnose and manage childhood epilepsy through telemedicine, which led to the development of the Project Epidet initiative. In collaboration with Silicon Labs (also known as “芯科科技”), they are using the EFR32BG22(BG22) series of low-power Bluetooth SoCs to create a portable medical device that is energy-efficient, wirelessly connected, compact, and equipped with accurate and reliable detection algorithms. Click the Read Original button at the end of the article or visit the link below for the full article: https://cn.silabs.com/applications/home-and-life/connected-health/rethinking-epilepsy-management-with-a-portable-medical-device
Rethinking Epilepsy Treatment
Science fiction often predicts technological advancements that may one day become part of our daily reality. From smartphones to smartwatches, from virtual reality headsets to autonomous vehicles, what once seemed purely fantastical is rapidly becoming an interconnected part of our lives.
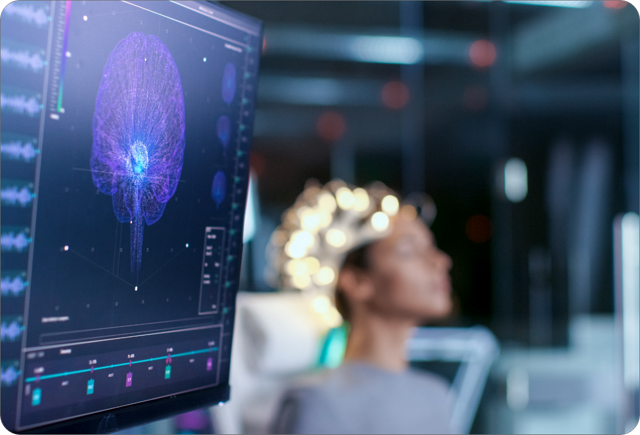
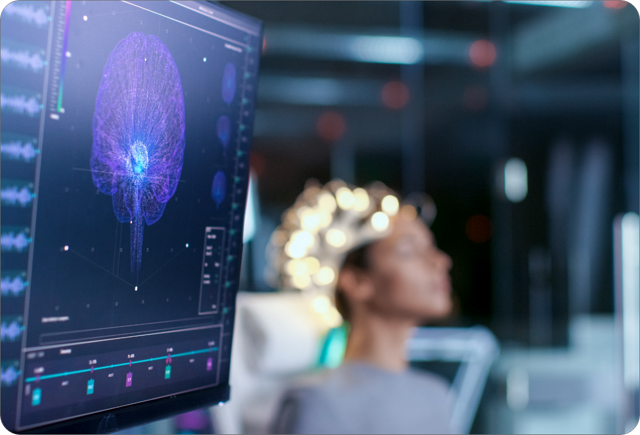
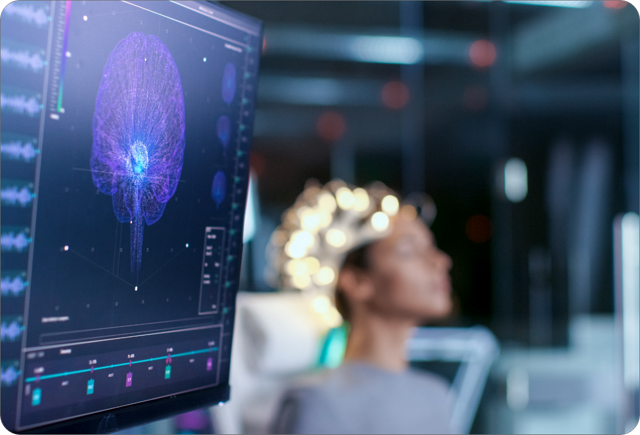
Today’s portable medical devices provide continuous monitoring, real-time alerts, machine learning (ML) analytics, and virtual or remote cloud-connected consultations with doctors for immediate assistance. With ongoing advancements in many medical fields providing instant feedback, there is one global disease that particularly warrants attention, where technological innovations present exciting breakthrough opportunities that could change many lives. According to the World Health Organization, over 50 million people worldwide suffer from epilepsy; nearly 80% of whom live in low- and middle-income countries. Furthermore, if properly diagnosed and treated, it is estimated that 70% of epilepsy patients could be seizure-free. Considering the latest advancements in embedded IoT devices, what can we do to address this issue??

Wireless Monitoring Applications for Epilepsy Patients
Dr. Clarke has witnessed the damaging consequences of uncontrolled or poorly monitored epilepsy. He states: “Some conditions, like infantile spasms, should be treated as medical emergencies, but often go undetected for months.“ They require immediate treatment, or severe consequences may occur. If you can better define epilepsy or other types of symptoms safely and effectively, it will benefit everyone in medical management.
To this end, Dr. Clarke initiated the Project Epidet development plan, focusing on creating a device that provides an early warning system for caregivers of epilepsy patients. Despite the lofty goals, Dr. Clarke is acutely aware of the complexities of immediate detection and prediction of seizures related to epilepsy.
According to Dr. Clarke, part of the challenge lies in the various types of seizures, including focal seizures that begin in one area of the brain but can spread. There are also tonic-clonic seizures, which involve loss of consciousness and generalized muscle contractions. Absence seizures can cause patients to stare blankly into space for a few seconds. Myoclonic seizures result in brief spasms of muscles or muscle groups. Tonic seizures are characterized by sudden stiffness or tension in the muscles of the arms, legs, or trunk, leading to a sudden loss of muscle strength. Devices monitoring generalized tonic-clonic seizures, which involve whole-body movements, may miss subtle movements associated with different types of seizures.FDA has some sufficiently sensitive technologies to monitor movements, but they have not yet been approved, and research is exploring other methods.
Another challenge is that when a product transitions from the realm of “entertainment only” health wearables to medical monitoring, the FDA requires evidence of efficacy and safety. The complexity of achieving this goal increases by an order of magnitude, which is one of the reasons so few companies pursue portable medical devices. However, Dr. Clarke believes that epilepsy should also be manageable. For about 70% of epilepsy patients, antiepileptic drugs provide a pathway to freedom from seizures. For the other 30% who cannot be treated with medication, seizure prediction is crucial, creating opportunities to improve their lives.
Capturing All Physiological Features with Portable Medical Devices

Despite the many types of seizures, all seizures share some common physiological features. For example, when a seizure begins, the patient’s brain activity increases, and other reactions may occur, including sweating, temperature fluctuations, and heart rate changes. Seizures can be life-threatening due to cardiac or respiratory complications, and sometimes tragically lead to sudden unexpected death in epilepsy (SUDEP). This risk is particularly high for those who frequently experience undetected seizures.
Dr. Clarke and his team are dedicated to creating a user-friendly wireless device that is comfortable to wear and suitable for non-medical personnel. It can also detect many types of seizures, typically alerting caregivers immediately when the patient is unaware or does not remember the event. Through continuous monitoring and data collection, Project Epidet will be able to log data and establish a history of captured events. This data can be used to predict future events and alert patients to take preventive measures.
Dr. Clarke points out: “Seizures can affect bodily systems outside the brain.““In collaboration with Silicon Labs (also known as “芯科科技”), we are researching autonomous features—skin conductance measurement (skin conductivity), temperature, and acceleration measurements (movement measurement) that influence sleep and other parameters, to better utilize data to predict when seizures will occur. Other exciting advancements include how we use heart rate and other parameters to define different types of epilepsy. Such devices could fundamentally change how we view patients and improve epilepsy management. We will find answers faster, which benefits everyone.“
How to Achieve Portable Medical Devices
Advancements in semiconductor technology have miniaturized devices, ultimately making them fully disposable. We can now offer small devices with tiny electronic packages, including an application microcontroller unit (MCU), wireless connectivity, analog peripherals, general I/O, integrated power supplies, and the ability to interface various sensors based on the desired data collection.
In the context of the pandemic, sensors monitoring ECG and electrodermal activity (EDA), temperature, movement (decline or rest conditions), and heart rate and variability (HRV) can easily connect to a system on chip (SoC) with sufficient memory to run advanced algorithms, handle secure connections with mobile phones or gateways, provide state-of-the-art security protections for devices and users from intrusive activities, and operate for weeks before needing a recharge or replacement.
These small, low-power devices open up new design avenues for innovators like Dr. Clarke and his team.
Dr. Clarke states: The first thing to think about when manufacturing a device is—how user-friendly is it for patients? Another very important consideration is cultural sensitivity. The device is being carefully modeled so that it can be promoted globally and serve as an effective epilepsy management tool across all cultures. Addressing these issues for only a portion of our population would be a disservice, as improving global outcomes is our true goal.“
Cultural diversity is another significant challenge faced by medical device manufacturers (especially when looking to enter international markets). Social environments, family preferences, and expectations can influence the use of wireless medical devices, not to mention anthropometric characteristics and language barriers. Personalized care and privacy are particularly sensitive topics when caring for children.Globally, 80% of epilepsy patients live in low- to middle-income countries, thus a device that is easy to wear, cost-effective, and improves access to care has the potential to significantly alleviate the global burden of epilepsy.
Like continuous glucose monitors (CGM) and dynamic ECG patches, Project Epidet needs to be small and flexible enough not to restrict patients’ daily activities while collecting the required data. It also needs the necessary components and battery capacity to accomplish this. In some cases, patches can even be disposable, considering environmental and cost factors, to be used for a week or two before recycling or reusing.
Flexible patches can be more easily secured to the body with adhesives and provide better signal acquisition during physical activity and exercise. Conversely, stiffer patches can accommodate larger, replaceable batteries and can be strapped to the arm or chest with elastic bands. They are also more likely to displace during activity, possibly requiring readjustment or recalibration of measurements during exercise.Thus, smaller and more flexible form factors are ideal, such as the Silicon Labs‘s EFR32BG22 which offers application MCU, Bluetooth 5.2 connectivity, ultra-low power consumption, compact size, and a range of peripherals for sensor integration, all integrated in a single SoC.
Accurate and Reliable Detection Algorithms

The next challenge is to implement accurate and reliable detection algorithms. Sensors will collect ECG and EDA readings, monitor temperature and device acceleration, and locally process all this information on the device.
The chosen BG22 includes an ARM Cortex-M33 core running at frequencies up to 76.8 MHz, featuring 352kB Flash (512k variant available) and 32kB RAM. The device has a dedicated Cortex-M0+ core driving the Bluetooth wireless electronic system, which allows the M33 core and sufficient memory to handle application and data processing algorithms. This enables Project Epidet to obtain the frequency and resolution required to detect various types of seizures, process all data locally on the device, and utilize the Bluetooth radio to send case results, providing necessary updates to caregivers and recording and further analyzing via the cloud.
This means that all relevant parties will benefit from the device: patients, their families and/or caregivers, and healthcare providers. For patients, it provides protection; for families/caregivers, it offers reassurance that they will be able to intervene when necessary. For providers, it will determine the true frequency of seizures and allow for accelerated decision-making and care management.
Device Power Consumption Design
Another major design decision weighs factors such as size, power consumption, battery choice, whether the device is disposable, rechargeable, or potentially has a replaceable battery, battery type and shape, etc. Design standards are partly driven by BG22‘s low power consumption, as it runs applications and processes periodic transmissions through optimized low-power Bluetooth connectivity, combined with the power consumption of various sensors, components on the signal chain, and external EEPROM needed to store data samples. Data acquisition is a significant component of the power consumption budget. Clever techniques and optimizations are needed to avoid continuously monitoring all sensors by default, thus reducing the average power consumption of the device. It is also necessary to provide a convenient way to recharge the battery within the device.
The key to maximizing the battery life of Project Epidet is that the BG22 consumes only 27uA per MHz when active and operates at 1.2uA in the lowest sleep state. This power-optimized device offers 5 energy modes: EM0 (fully running), EM1 (sleep), EM2 (deep sleep), EM3 (stop), and EM4 (off). Depending on the mode, various architecture components can be enabled or disabled, allowing the system to optimize the overall power budget of the device.
Additionally, utilizing sensor interrupts and Bluetooth functionality minimizes TX/RX time, saving overall power. RFSense is another unique feature of the EFR32 wireless MCU series, allowing the MCU to be “woken up” from EM2 or even EM4 power modes, further saving power for the device.
For More Information, VisitSilicon Labs‘s Official Website: https://cn.silabs.com/applications/home-and-life/connected-health/rethinking-epilepsy-management-with-a-portable-medical-device
ExploreBG22 Low-Power BluetoothSoC and Module Information: https://cn.silabs.com/wireless/bluetooth/efr32bg22-series-2-socs
You can also scan the QR code below to follow Silicon Labs on social media platforms.