Abstract
Objective To explore the significance of detecting the thickness of the ganglion cell complex (GCC) in the macular region for diagnosing patients with preperimetric glaucoma (PPG). A self-controlled study and case-control study design were employed. The study subjects included 20 patients with primary open-angle glaucoma (POAG) (20 eyes without visual field defects in the PPG group and 20 eyes with visual field defects in the POAG group) and 30 normal controls (30 eyes).
Methods The RTvue SD-OCT was used to measure the GCC thickness in the macular region and the retinal nerve fiber layer (RNFL) thickness around the optic disc. The ability of each parameter to distinguish between PPG and normal eyes was evaluated using the area under the receiver operating characteristic curve (AUC). The main indicators were the thickness of GCC and RNFL, as well as their AUC values.
Results The average GCC thickness (AvgGCC), superior GCC thickness (SupGCC), inferior GCC thickness (InfGCC), average RNFL thickness (AvgRNFL), superior RNFL thickness (SupRNFL), and inferior RNFL thickness (InfRNFL) in the PPG group were all thinner compared to the normal control group, with statistically significant differences (t=5.508, 5.402, 5.576, 6.517, 5.849, 5.392, P<0.001). However, all were thicker than those in the POAG group, with statistically significant differences (t=4.778, 3.698, 4.593, 5.209, 3.757, 5.450, P≤0.002). The overall loss volume of GCC (GCC-GLV) and the focal loss volume (GCC-FLV) in the PPG group were larger than those in the normal control group, with statistically significant differences (t=6.539, 2.515, P<0.001, P=0.021), but smaller than those in the POAG group, with statistically significant differences (t=6.013, 7.669, P<0.001). The AUC values for AvgGCC, SupGCC, InfGCC, GCC-GLV, GCC-FLV, AvgRNFL, SupRNFL, and InfRNFL for diagnosing PPG were 0.910, 0.898, 0.908, 0.983, 0.724, 0.930, 0.918, and 0.863, respectively. Among the GCC parameters, the diagnostic efficacy of GCC-GLV was the highest, and there was no statistically significant difference when compared with the AUC value of AvgRNFL from the RNFL parameters (P>0.05).
Conclusion GCC thickness can serve as an effective indicator for screening PPG.
Keywords: Glaucoma; Visual Field; Ganglion Cell Complex; Retinal Nerve Fiber Layer; Optical Coherence Tomography
When characteristic structural damage of glaucoma appears in the fundus, such as disc rim narrowing, notching, hemorrhages, cup enlargement, and deepening, or when the retinal nerve fiber layer (RNFL) has thinned but the visual field examination is normal, it is referred to as preperimetric glaucoma (PPG).
Sommer et al. and Wu et al. suggest that damage to retinal ganglion cells (RGCs) and loss of their axons occur before visual field defects manifest in glaucoma patients.
Research by Quigley et al. found that a 20% loss of RGCs corresponds to a 5 dB decrease in retinal light sensitivity during visual field testing, while a 40% loss corresponds to a 10 dB decrease; in late-stage glaucoma patients, only 10% or less of RGCs remain. Due to the irreversibility of visual function damage in glaucoma, how to detect and diagnose glaucoma before visual field damage occurs and provide proactive and effective treatment is crucial for reducing the blindness rate caused by glaucoma.
The instruments currently used for quantitatively detecting structural damage in PPG include optical coherence tomography (OCT) and confocal scanning laser ophthalmoscopy (CSLO).
Studies indicate that OCT measurement of RNFL thickness around the optic disc is more effective for diagnosing PPG than the third-generation Heidelberg Retina Tomograph (HRT-III) CSLO. However, some PPG patients do not exhibit thinning of RNFL thickness, and factors such as oblique optic disc entry, large optic discs, and high myopia with peripapillary choroidal atrophy can reduce the accuracy of RNFL thickness measurement.
The ganglion cell complex (GCC) includes the RNFL, RGC layer, and inner plexiform layer (IPL), representing the axons, cell bodies, and dendrites of RGCs, respectively. As glaucoma progresses, the decrease in RGCs leads to thinning of GCC.
Frequency-domain OCT (SD-OCT) has an axial resolution of 3-6 μm and a scanning speed of 26,000-27,000 A-scans per second. Compared to time-domain OCT, SD-OCT significantly improves detection accuracy, allowing for more precise and reliable measurement of GCC thickness in the macular region.
Bhagat et al. found that the efficacy of GCC thickness in diagnosing PPG is greater than that of RNFL thickness, while Lisboa et al. believe that RNFL thickness is more meaningful for diagnosing PPG than GCC thickness.
To further investigate the diagnostic value of GCC thickness for PPG, we used RTVue SD-OCT to study 20 patients with primary open-angle glaucoma (POAG) (one eye with visual field defects and the contralateral eye with no visual field abnormalities) to analyze the clinical characteristics of GCC thickness in the macular region and RNFL thickness around the optic disc, as well as their diagnostic efficacy for PPG.
Data and Methods
Clinical Data
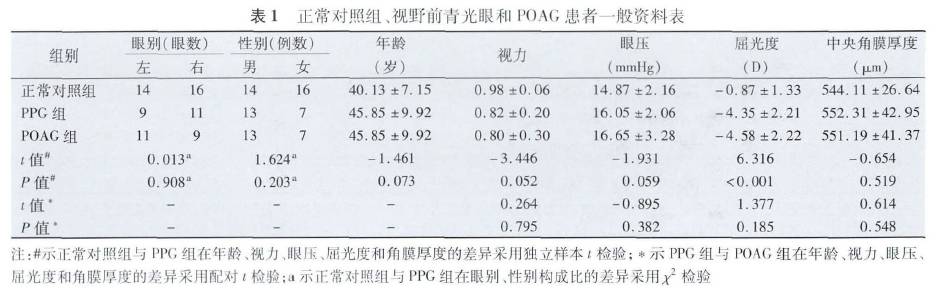
We collected data from POAG patients who visited Beijing Tongren Hospital Eye Center from November 2015 to April 2016. Using Humphrey visual field as the standard, we screened 20 patients (40 eyes) with one eye having visual field defects and the contralateral eye having normal visual field but with glaucoma-related optic disc and RNFL changes (13 males and 7 females, average age (45.85±9.92) years). The eyes with visual field defects were included in the POAG group, while the eyes without visual field defects were included in the PPG group. Thirty healthy volunteers (30 eyes) served as the normal control group (14 males and 16 females, average age (40.13±7.15) years), with data analysis conducted using the right eye. There were no statistically significant differences between the normal control group and the POAG patients regarding gender, eye side, visual acuity, age, intraocular pressure, and central corneal thickness, except for refractive error (Table 1).
Inclusion criteria for POAG (eyes with visual field defects):
-
Best corrected visual acuity ≥0.2, able to complete visual field examination, and one eye with glaucoma-related visual field defects while the contralateral eye has normal visual field.
-
Pre-treatment intraocular pressure >21 mmHg.
-
Optic disc showing glaucoma-specific damage: such as disc rim narrowing, notching, hemorrhages, and RNFL defects.
-
Open angles.
-
Spherical refractive error: -7.00D to +2.00D, cylindrical refractive error: -1.50D to +1.50D.
Exclusion criteria:
-
Secondary glaucoma.
-
Unreliable results with fixation loss rate >20%, false positive rate >15%, false negative rate >15%.
-
Anterior segment abnormalities, uveitis, retinal, choroidal diseases, other optic nerve diseases besides glaucoma, and history of intraocular surgery.
Visual acuity was measured using the international standard visual acuity chart, intraocular pressure was measured with the Canon TX-20 non-contact tonometer (Canon Inc., Japan), and fundus examination was performed using the Kowa nonmyd WX 3D stereo camera (Kowa Company, Japan). The gonioscope used was the Goldmann double-sided gonioscope (Ocular Instruments, USA).
Inclusion criteria for the normal control group:
-
Best corrected visual acuity ≥0.9;
-
Intraocular pressure <21 mmHg, with a difference of <5 mmHg between both eyes, and no history of elevated intraocular pressure;
-
Cup-to-disc ratio (C/D) <0.5, with a difference of ≤0.2 between both eyes, and no signs of disc rim narrowing, notching, hemorrhages, or RNFL defects;
-
Open angles;
-
Reliable and normal visual field examination results;
-
Spherical refractive error: -6.00D to +2.00D, cylindrical refractive error: -1.50D to +1.50D.
Exclusion criteria: History of ocular diseases other than refractive errors.
2
Examination Methods
GCC thickness detection in the macular region: The RTvue SD-OCT (Optovue Inc., USA, version 4.0) was used to detect GCC thickness, selecting the “GCC” program. It consists of one horizontal scanning line (passing through the fovea) and 15 vertical scanning lines (spaced 0.5 mm apart).
RNFL thickness detection around the optic disc: The RTvue SD-OCT was used to measure RNFL thickness, selecting the “ONH” program. Thirteen circular scans and twelve radial scans were performed centered on the optic disc, with circular scan diameters ranging from 1.3 to 4.9 mm and each ring spaced 0.3 mm apart. The machine’s software analyzed the RNFL thickness within a 3.45 mm diameter area centered on the optic disc.
Humphrey visual field examination: The Humphrey 750i visual field analyzer (Carl Zeiss AG, Germany) was used for visual field testing. The central 30-2 threshold program and SITA-FAST testing strategy were selected, with both the background light and the cursor being white, using size III targets, and corrections made for refractive errors before testing. Only those who completed Humphrey visual field and RTVue SD-OCT within one month were included in the statistical analysis.
3
Statistical Methods
Statistical analysis was performed using SPSS 19.0 software, with count data expressed as x±s. The differences in count data between the PPG group and the normal control group were compared using independent sample t-tests, while the gender composition ratio was compared using the χ2 test. The differences in count data between the PPG group and the POAG group were compared using paired sample t-tests.
The diagnostic efficiency of GCC thickness and RNFL thickness for POAG was evaluated by plotting the ROC curve and calculating the AUC, with comparisons of AUCs between groups using z-tests. A P value <0.05 was considered statistically significant.
Results
GCC Thickness in the Macular Region
The average GCC thickness (AvgGCC), superior GCC thickness (SupGCC), and inferior GCC thickness (InfGCC) in the PPG group were lower than those in the normal control group, and the GCC focal loss volume (GCC-FLV) and global loss volume (GCC-GLV) were larger than those in the normal control group, with all differences being statistically significant (t=5.508, 5.402, 5.576, 2.515, 6.539, P values for FLV=0.021, others P<0.001), as detailed in Table 2.
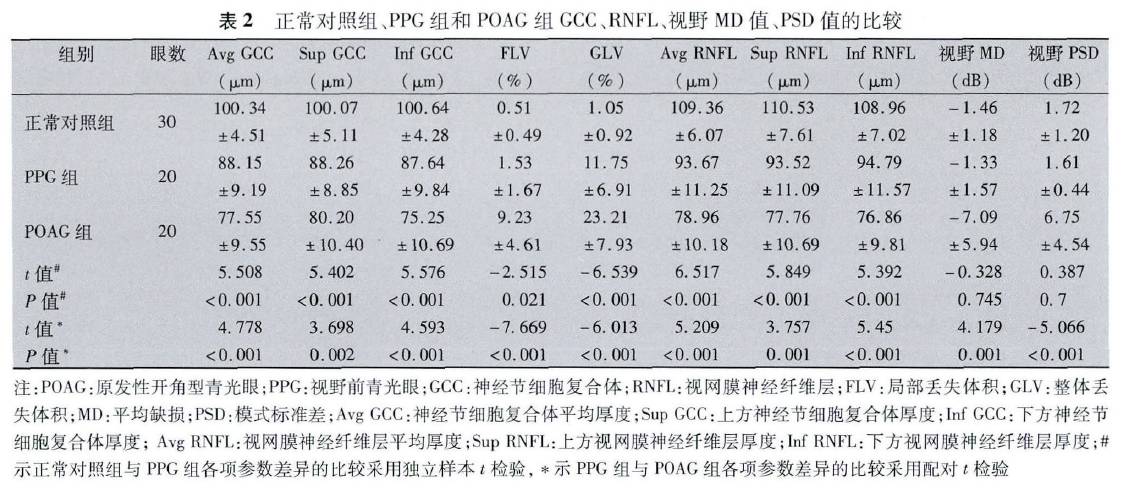
The AvgGCC thickness, SupGCC thickness, and InfGCC thickness in the PPG group were higher than those in the POAG group, while GCC-FLV and GCC-GLV were smaller than those in the POAG group, with all differences being statistically significant (t=4.778, 3.698, 4.593, 7.669, 6.013, P≤0.002) (Table 2).
2
RNFL Thickness Around the Optic Disc
The average RNFL thickness (AvgRNFL), superior RNFL thickness (SupRNFL), and inferior RNFL thickness (InfRNFL) in the PPG group were lower than those in the normal control group, with statistically significant differences (t=6.517, 5.849, 5.392, P<0.001), as detailed in Table 2. The AvgRNFL thickness, SupRNFL thickness, and InfRNFL thickness in the PPG group were all greater than those in the POAG group, with statistically significant differences (t=5.209, 3.757, 5.450, P≤0.001) (Table 2).
3
Visual Field Examination Results
The average mean defect (MD) value and pattern standard deviation (PSD) in the PPG group were not statistically significant compared to the normal control group (t=0.328, 0.387, P=0.745, 0.700); however, there were statistically significant differences when compared to the POAG group (t=4.179, 5.066, P≤0.001), as detailed in Table 2.
4
Diagnostic Efficiency of GCC Thickness and RNFL Thickness for PPG
The AvgGCC thickness, SupGCC thickness, InfGCC thickness, GCC-FLV, GCC-GLV, AvgRNFL thickness, SupRNFL thickness, and InfRNFL thickness were plotted on ROC curves, all located above the reference line (Figure 1).
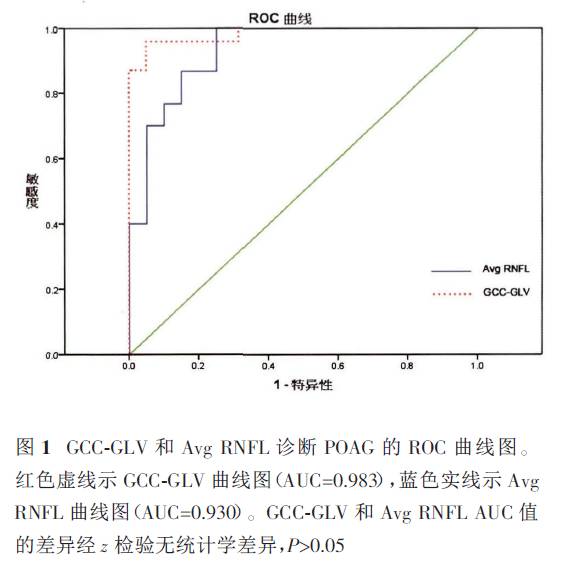
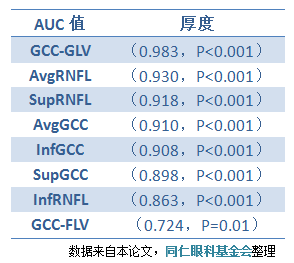
Except for GCC-FLV, all other parameters showed high diagnostic efficacy, with GCC-GLV (0.985) showing the highest diagnostic efficacy among GCC parameters, and there was no statistically significant difference when compared to the highest efficacy parameter AvgRNFL (0.930) among RNFL parameters (P>0.05).
Conclusion
How to early diagnose POAG and provide proactive and effective treatment to prevent visual function damage has always been a challenging issue in ophthalmology. RGCs are primarily located in the macular region, distributed in about 2-7 layers, making it the only area in the retina where RGCs exceed a single layer of cell arrangement. The thinning of retinal thickness in glaucoma patients is mainly due to the thinning of RGCs and RNFL in the macular region.
Tan et al. found that OCT could detect thinning of the inner retinal thickness in the macular region before visual field defects occur in glaucoma patients. Due to the high density of RGCs in the macular region, the macular region may become an ideal area for detecting early RGC loss in glaucoma and monitoring RGC changes with disease progression.
Mwanza et al. studied the thickness of the ganglion cell-inner plexiform layer (GCIPL) and RNFL thickness around the optic disc in 58 early glaucoma patients and 99 healthy controls, suggesting that the thickness of GCIPL in the macular region has similar or even stronger diagnostic efficacy than the RNFL thickness around the optic disc.
Seol et al. studied 104 eyes with high myopic PPG, 67 eyes with non-high myopic PPG, and 182 eyes with simple high myopia, finding that the thickness of GCIPL in the macular region was superior to RNFL thickness around the optic disc for diagnosing high myopic PPG, with the inferior temporal GCIPL thickness being the best parameter for diagnosing high myopic PPG.
Bhagat et al. studied 70 eyes with PPG, 62 eyes with POAG, and 68 healthy controls, concluding that the thickness of GCC in the macular region was superior to RNFL thickness around the optic disc for diagnosing PPG.
Thus, whether measuring the thickness of GCIPL composed of RGC cell bodies and dendrites, or the GCC thickness that integrates axons, cell bodies, and dendrites, both are significant for diagnosing early glaucoma and even PPG.
Our study found that although there was no statistically significant difference in MD and PSD values between the PPG group and the normal control group, both the GCC thickness and RNFL thickness in the macular region were thinner in the PPG group compared to the normal control group, but thicker than those in the POAG group, with all differences being statistically significant, consistent with the findings of Takagi et al. and Na et al.
The maximum AUC value for diagnosing PPG among GCC parameters was GCC-GLV (0.983), while the maximum AUC value for diagnosing PPG among RNFL parameters was AvgRNFL thickness (0.930), with no statistically significant difference (P>0.05). Therefore, we believe that the thickness of GCC in the macular region has similar or even stronger diagnostic efficacy than RNFL thickness around the optic disc, consistent with the findings of Bhagat et al. and Mwanza et al.
GCC-GLV represents the reduction of the entire GCC thickness in the macular region of the subject compared to the normal database, reflecting diffuse damage. In contrast, GCC-FLV represents the degree of variation in GCC thickness compared to the normal database, indicating focal damage.
For PPG patients without visual field defects, GCC-GLV is more meaningful, which aligns with our findings. We observed that among all GCC parameters, GCC-GLV (0.983) had the highest diagnostic efficacy for PPG, followed by AvgGCC thickness (0.910), InfGCC thickness (0.908), and SupGCC thickness (0.898), while the diagnostic efficacy of GCC-FLV (0.724) was the weakest.
Distante et al. analyzed the relationship between Humphrey visual field, RNFL thickness, and GCC thickness parameters in 50 glaucoma patients, using Medeiros’ empirical formula to estimate RGC counts in glaucoma patients, finding that GCC-GLV correlated most with RGC counts, suggesting that GCC-GLV could replace RGC counts in clinical practice. This indicates that the parameters of GCC in the macular region may have certain clinical value for detecting early RGC loss in glaucoma.
Studies on the repeatability of SD-OCT results for detecting structural damage in glaucoma have found that the coefficient of variation for RNFL thickness is 1.5%-4%, while for GCC thickness, it is 0.4%-2.8%. This shows that the reliability of measuring GCC thickness using SD-OCT is higher than that of RNFL thickness, indicating that GCC thickness has advantages over RNFL thickness.
Hirasawa et al. analyzed two main reasons: first, the thickness of GCC in the macular region is minimally affected by the large blood vessels in the retina; second, it is easier to locate the center of the macular region than the center of the optic disc during instrument measurements, meaning that the overlap of areas measured for GCC thickness during multiple follow-up assessments is higher than that for RNFL thickness.
In conclusion, the thickness of GCC in the macular region has similar or even stronger diagnostic efficacy for PPG compared to RNFL thickness around the optic disc. For PPG patients without visual field defects, GCC-GLV, which reflects diffuse damage, is more clinically significant than GCC-FLV, which reflects focal damage.
Wang Huaizhou
Doctor of Ophthalmology, Associate Chief Physician at the Eye Center of Beijing Tongren Hospital, Deputy Director of the Office of the Eye Center.
Member of the Visual Physiology Group of the Ophthalmology Branch of the Chinese Medical Association, Secretary of the Glaucoma Professional Committee of the Chinese Medical Doctor Association, Member of the Ophthalmology Professional Committee of the Chinese Medical Equipment Association, and Youth Member of the Ophthalmology Branch of the Beijing Medical Association.
He has long followed Professor Wang Ningli in clinical and research work. He has rich clinical experience and skilled surgical techniques in the diagnosis and treatment of glaucoma, cataracts, and high myopia, and has pioneered procedures such as vacuum trabeculoplasty (PNT), trabectome, express glaucoma drainage device implantation, canaloplasty, and 360-degree trabeculotomy guided by catheters.
Source: “Ophthalmology” 2017 Vol. 26, Issue 1 Wang Weiwei, Wang Huaizhou, Liu Jianrong, Huo Yanjiao, Li Meng, Yang Xinguang
Editor: Xu Qingzi