-
DR. RUDOLF SLAVICEK
Diagnosis is the key to treatment and the principle upon which medicine acts. Splints are therapeutic aids designed to execute specific treatment concepts correlated to the diagnosis, with the goal of balancing the dynamic triangle of TMJ, occlusion (on the splint), and musculature.
Treatment planning begins with the patient’s chief complaint and the subjective information derived from the occlusal index questionnaire. Extensive objective data from the clinical functional and instrumental analyses aid further in the formulation of a proper diagnosis.
The science behind my splint therapy is derived from this manual or computerized information, which is absolute, verifiable, and repeatable. The hypotheses are goal-oriented, and the treatment expectations easily quantified with subsequent data. The more data we have collected for our left-brain thinking, the freer our right brain is to formulate the diagnosis and treatment plan, and to control and monitor treatment.
Patient Management
My practice has a high percentage of dysfunctional patients with pain, but only 20-25% of these receive splints–and then only for four to six weeks. Fifteen years ago, I would perform splint therapy on 90-100% of these patients for eight to 18 months. Today, I feel I have better diagnostic means to formulate definitive treatment plans and execute them efficiently.
Regardless of its configuration, a splint invokes rapid, specific, irreversible changes. It is therefore imperative that you deal with the patient before you deal with the patient’s problems via splint therapy. The patient will project any psychological problems onto what he or she believes is a diseased gnathological system.
Let the patient first tell you the problem in subjective terms. Don’t solicit information by asking about headaches or pain. Give the patient time to disclose everything he or she feels is important before you proceed to a full instrumental analysis. You may find many problems, but if they are of no consequence to the patient you have no justification for initiating treatment. This is not to say that the patient should not be informed of any concerns that might develop into serious problems later.
Don’t evaluate a pain patient according to your concept of an ideal occlusion. No one has an ideal Class I occlusion, and most people function well with what they have. Modifying the situation through splint therapy might leave the patient in an occlusal situation for which he or she can no longer compensate.
Consider a young female with a CO-CR discrepancy and myofascial pain. Does her pain result from the occlusion or from psychological problems–stress or muscle tension from using her system as a stress release center? A splint to retrude the mandible might temporarily relieve her pain, but you may have violated one of nature’s biological compensating mechanisms and decompensated her by half a molar width or more. Perhaps she was protrusive because her teeth fit together better that way, or she thought she looked better with more of a chin. After several weeks of “successful” splint therapy, you might have a maxillofacial surgery case with two and one-half to three years of orthodontic treatment and the possibility of recurring pain.
Splint therapy lasting more than three months must be reevaluated. Long-term use is not therapy. You may intrude teeth, change the occlusal plane and occlusion, alter TMJ function, or interfere with muscle programming and proprioception. Three-dimensional computer analysis has demonstrated a widening in maxillary arch form as a result of long-term splint usage.
The clinical and instrumental functional analysis gives you the data necessary to formulate a comprehensive diagnosis with appropriate monitoring capability. But you must inform the patient of your treatment objectives and the possible ramifications of splint therapy–which can in some cases make further treatment even more complex.
Splint Construction
The splints I use are divided into five categories: myopathic, compression, distraction, verticalization, and anterior repositioning, or any combination thereof. The first four types are reference position (RP) splints; the last is a deranged reference position (DRP) splint.
Casts are mounted to the reference position split cast, verified by the wax interocclusal record. A facebow mounting is essential. All positional changes are made relative to the RP, even if it is a DRP. Therefore, you cannot use a leaf gauge, Lucia jig, power centric, power bite, protrusive check bite, or retrally positioned occlusal record. These kinds of bite records interfere with the balance between the muscle and the ligamentous position of the mandible.
Using the information from manual or computer axiography, the articulator is programmed for the horizontal condylar inclination (H.C.I.) of the protrusive-retrusive movement, and the lateral guidance is set to follow the mediotrusive pathways. For a compression splint, the condyles are set .3mm superiorly.
The splint construction procedure is as follows:
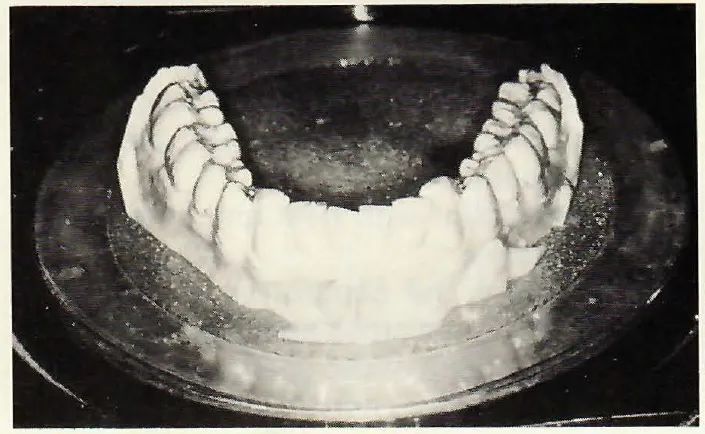
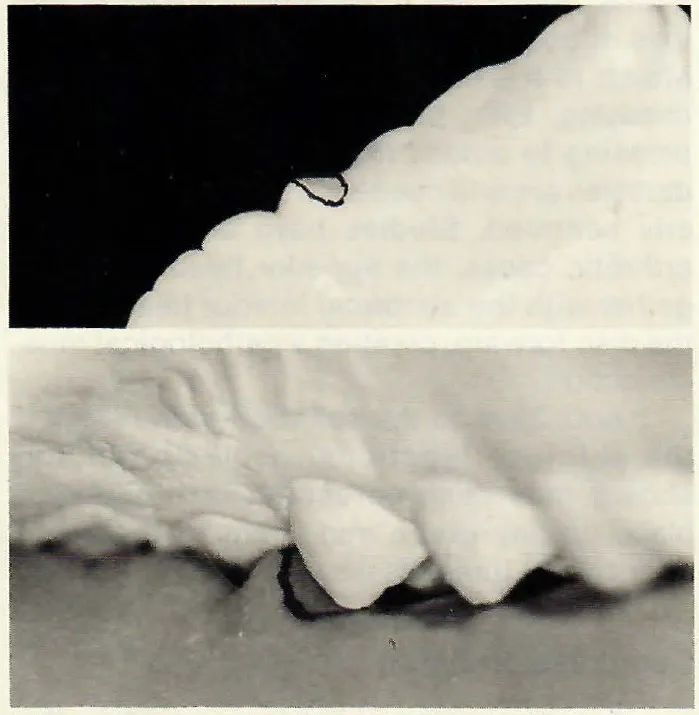
1. Make a duplicate of the mounted mandibular cast (Fig. 114).
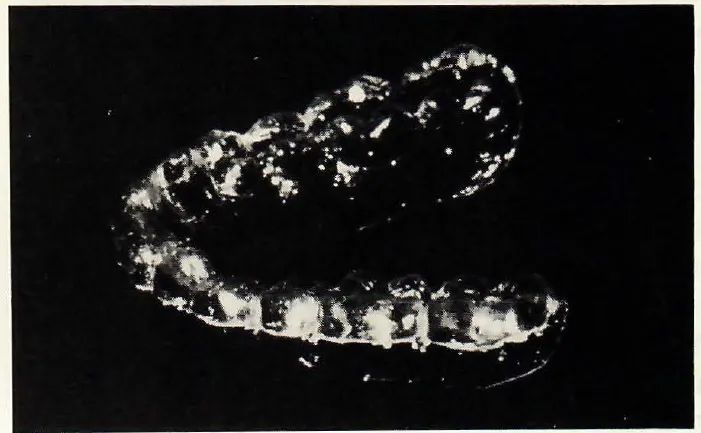
2. Make a .5mm matrix by vacuum or pressure molding, and trim it to 1mm below the height of the posterior teeth (Fig. 115).
3. Place the matrix on the articulated cast, close to the first point of contact, and fix the incisal pin.
4. Open the incisal pin 1mm, except for a verticalization splint. In that case, open the pin to the desired lower facial height (given in millimeters on the diagnostic summary sheet). Be careful to observe the depth of the second molar’s palatal cusp tip, which may create a balancing side interference if you cannot disocclude it with proper incisal guidance.
5. Paint the occlusal surface of the maxillary cast with a separating medium.
6. For a decompression splint, place a .3mm foil shim in each condylar housing by fixing it beneath the Bennett insert. For a myopathic splint, verify that the condyles are well centered in the discs.
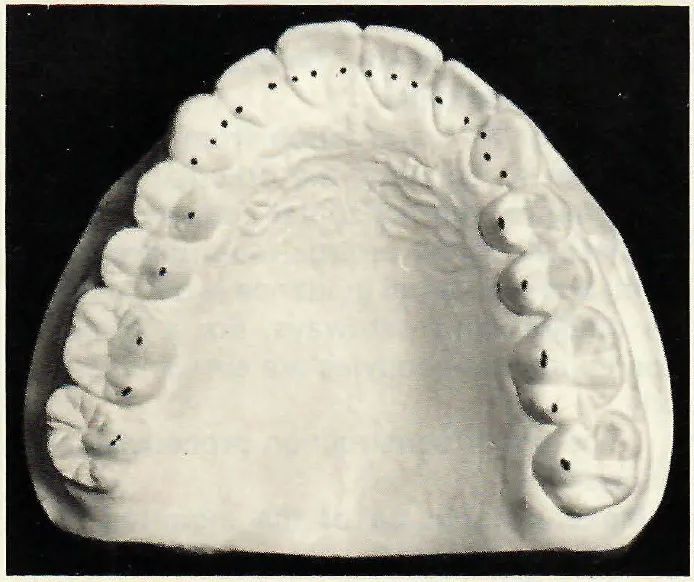
7. On the opposing cast, mark the posterior palatal cusp centric holding stops and the F1 occlusal stops on the palatal concavities of the anterior teeth (Fig. 116).
8. Cover the matrix with tooth-colored, quick-cure acrylic to occlude with the marked occlusal surfaces on the maxillary cast. Separate the acrylic at one cuspid so that the splint will be processed in two sections to minimize distortions. Don’t cover the matrix entirely if the acrylic has a tendency to distort; better retention is obtained by having only matrix material, rather than acrylic, below the heights of contour.
9. Cure the splint with heat and pressure to eliminate pores.
10. Reprocess the separation area at the cuspid to eliminate cross-arch distortions and rejoin the sections of the splint.
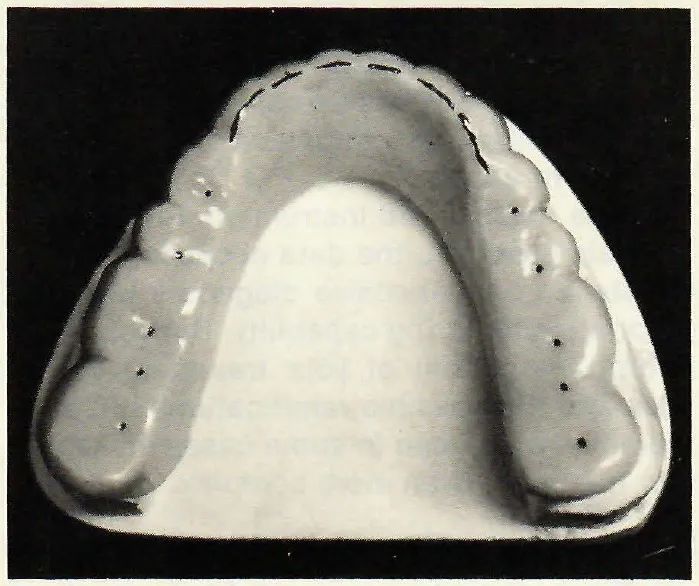
11. Trim away excess acrylic to leave a dimple 2mm long, 1mm wide, and .5mm deep where each palatal cusp contacts the splint on a flat plane (Fig. 117).
12. Place the splint on the articulated mandibular cast. Check the posterior centric holding stops and anterior F1 positions. If it is impossible to provide adequate anterior guidance from F1, make sure that all anterior teeth are in contact with the splint, then alter the guidance mechanisms to the cuspids or first premolars.
13. Lightly polish the splint and place it in water.
14. Deliver the splint to the patient. Instruct the patient to soak the splint occasionally in mouthwash.
Myopathic Splint
The myopathic splint is designed to relax the musculature and stabilize the gnathostomatic system for patients whose signs and symptoms indicate muscle problems. Diagnosis must establish whether the muscle problems are intraoral, extraoral, or both.
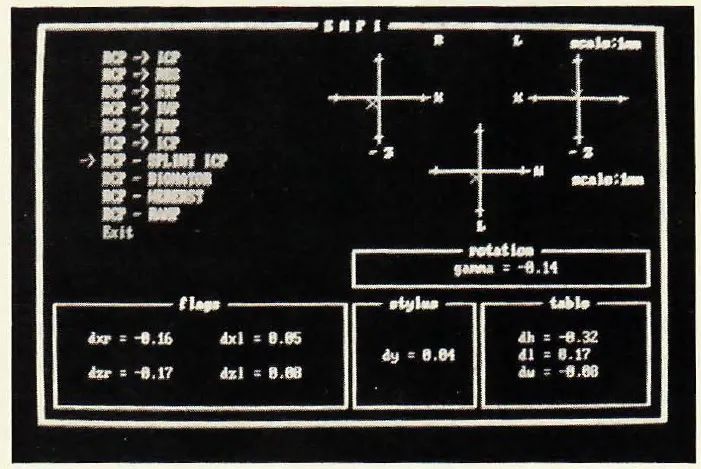
The splint is constructed as a flat plane posteriorly, with incisal guidance. Verify that the splint position is in harmony with the reference position by using a functional occlusion clutch and the Electronic Mandibular Position Indicator (E.M.P.I.) program of CADIAX (Fig. 119; see Part 7, JCO, December 1988).
The patient must first exercise and balance the closing muscle groups. Start biofeedback therapy so the patient is aware of muscle function, and solicit the patient’s cooperation in controlling the muscles during treatment.
Refer the patient to a physical therapist if there is a posture problem or muscle pain. Request a full workup from the therapist, and reinforce the physical therapy by explaining to the patient the necessity for the skeletal system to be balanced if the splint is to work appropriately. If necessary, refer the patient for psychological therapy and solicit active cooperation.
Administer small, controlled doses of medication if absolutely necessary. A hyperactive patient must be pacified before the splint is introduced.
Don’t tell the patient that the occlusion is terrible or that there is a prematurity, a slide in centric, a left-to-right deviation, etc. Tell the patient that you want him or her to relax with the splint, and to wear it only when he or she feels anxiety or tension. Night-time wear is permissible, but not desirable. Instruct the patient to increase water intake; check the medical history to see if diuretics are being used.
Have the patient come in immediately if the splint does not feel equal on both sides. See the patient daily for three days and then weekly for three weeks.
Patients with muscle problems must exercise the muscles to get them in balance before splint therapy. Direct the exercises toward the closing groups–the posterior bands of the temporalis, masseters, suprahyoids, and digastrics. If you insert a myopathic splint first, you will simply pacify these muscles, rendering the therapy useless. Computerized axiography (see Part 7, JCO, December 1988) is a good way to evaluate muscle balance and progress during treatment.
Deep masseter spasms will require reciprocal-action exercises and a few days of verticalization therapy. Follow up with biofeedback.
Active muscle exercise is required with any splint so that isotonic action will eliminate isometric spasm, retrain the superior head of the lateral pterygoid, and stretch this muscle. Have the patient sit at a table and cradle the mandible in both hands while resting the elbows on the table. The patient then elevates the head by opening the mouth, using only the opening muscles so that the entire weight of the skull is felt. The patient closes by relaxing these muscles.
This exercise is used for all splints and should be done for two to three minutes, three times a day, for three weeks. The patient should be completely relaxed and in a quiet environment. The exercises reinforce the rotational movement of the disc, but should not be done to the point that the patient becomes tired.
Decompression Splint
This splint is prescribed under the following circumstances: the Mandibular Position Indicator (M.P.I.) shows compression between RP and intercuspal position (ICP) (see Part 4, JCO, September 1988); the resiliency test is low; axiography with a functional occlusion clutch shows compression; the medical history indicates degenerative joint disease; a Fischer angle shows flattening of the condyle; transverse movements of .3mm can induce pain; the disc is medially displaced.
Construction is the same as with the myopathic splint except for the insertion of the .3mm shims placed into the condylar housings perpendicular to the hinge-axis. For partially or totally edentulous patients, .5mm shims should be used.
Instruct the patient to wear the splint whenever there is a possibility of the teeth coming together, but not during meals. The splint should not be worn at night unless the patient is more comfortable with it in, because the periodontium is already being stressed during daytime wear.
Monitor the system carefully. Distraction is contraindicated if there are loose ligaments, which are most often caused by the loss of bone supporting the discs where they attach to the medial and lateral poles of the condyles. Even though the splint is decompressing to unload the system, the elevating muscles are still needed to keep the disc properly centered. Studies have shown that in arthrotic cases, the superior head works together with the abnormal inferior head to pull the disc forward, creating a pathological muscle action.
Add .3mm to the splint after one week if the M.P.I. or functional occlusion clutch shows that decompression is not taking place. In any event, add .2mm to the splint after two or three weeks.
Compression Splint
A compression splint is used when the M.P.I. shows distraction between RP and ICP; the resiliency test is high, indicating a very loose joint; axiography shows considerable looseness in the system; the functional occlusion clutch shows distraction and looseness. The splint helps correct loose ligaments by using the muscles to stabilize the condyle within the disc.
Construction is the same as with the myopathic splint, except that the articulator is programmed at RP with the condyles placed .3mm superiorly. Clinical management is the same as with the myopathic splint.
Monitor the difference between RP and splint position using either the M.P.I. or the axiograph and functional occlusion clutch. Compress further if necessary, and continue to carefully check the ligamentous situation.
Verticalization Splint
This splint is designed to increase or decrease lower facial height. The ideal lower facial height is calculated in the CADIAS program (see Part 6, JCO, November 1988) at millimeter increments of incisal pin opening or closing. The computer graphics illustrate the positions of the mandible and teeth with the ideal vertical dimension, and a complete diagnostic summary is done at this new vertical. A good monitoring guideline is to observe the decline in deviations from the norms in all analyses.
The vertical dimension is nature’s way of compensating for skeletal discrepancies. Class II patients compensate by decreasing the vertical, and Class III patients by increasing it. The CADIAS analysis, which is based on my research with more than 2,000 asymptomatic patients, establishes an ideal vertical position for each patient according to the skeletal classification.
Anterior Repositioning Splint
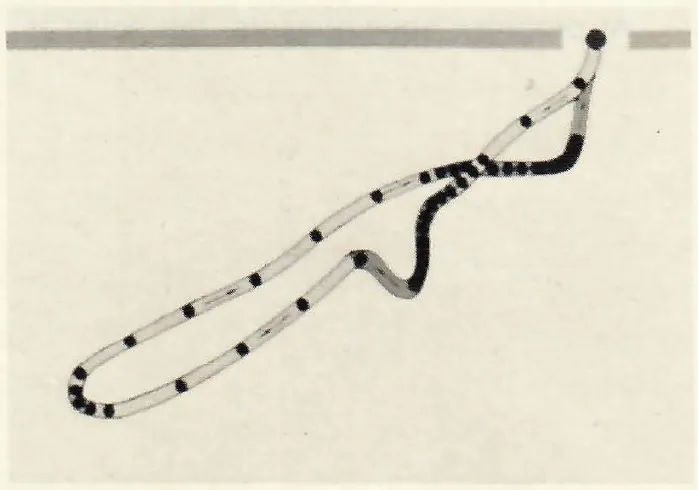
An anterior repositioning splint can reduce the joint, balance the muscle groups, and eliminate joint noises if they are disturbing to the patient. Note that joint noise in itself is not a disease. Be sure to distinguish between a luxation-reduction click (Fig. 120) and a ligamentous click (see Part 8, JCO, January 1989).
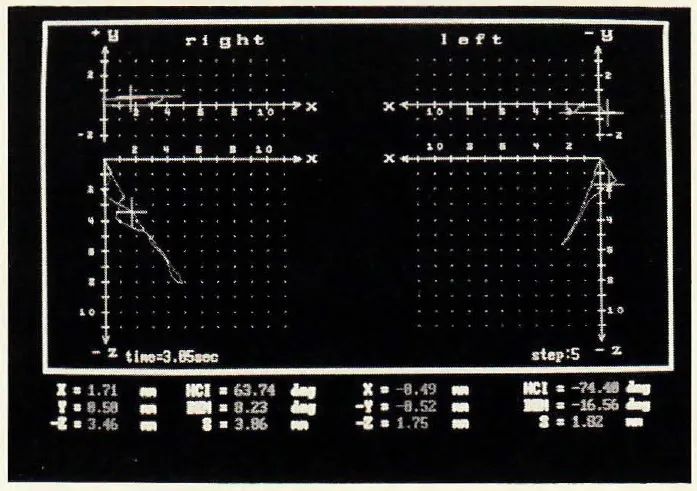
In construction, an anterior guidance ramp is placed mesial to the first maxillary premolar at the point of luxation. The CADIAX system provides the X, Y, Z coordinates of this position for articulator programming (Fig. 121).
The splint can be worn nearly full-time, but must be taken out at meals for chewing efficiency. The patient should be instructed to eat soft foods and not function posteriorly.
After two weeks, reduce the distal incline of the guidance ramp by .5mm with a round bur. Add self-curing acrylic to the occluding surfaces and place the splint immediately in the mouth. Have the patient protrude and retrude the mandible until the acrylic sets. Grind away the excess. Tell the patient to continue the exercises, but now moving backward and forward on the splint to stretch the pterygoid muscles, at least five times a day.
This “walking back” technique of ramp reduction is continued until the optimal position is achieved and verified as stable with axiography.
In most cases, the patient will not continue to luxate. If the patient feels that the condyle will come out of the disc, adjust the splint cranially for more stabilization. When in doubt, use axiography with a functional occlusion clutch to show the patient when the condyle is in or out of the disc.
The most important principle of reorientation therapy is that the closing muscles must be passive. This means that a myopathic splint, biofeedback, physical therapy, and/or muscle exercises must sometimes be used before anterior repositioning. Closing muscles will not be deactivated in a patient who has improper head posture, who cannot relax, or whose pain has not been relieved.
There are several drawbacks to repositioning therapy. Protrusion limits the range of motion, which is not good for a synovial joint. Repositioning shortens the lateral pterygoids, which magnetic resonance imaging has shown can lead to atrophy, and makes Bennett 90°. The retrodiscal pad area of the bilaminar zone is also violated, forcing the muscles forward without any assistance. Finally, you must remember that all derangements have loose ligaments, and you must be careful not to distract in such cases.
Splint Adjustments
At progress appointments, the splint is adjusted as follows:
1. Instruct the patient to wear the splint for at least an hour before the adjustment.
2. Take several minutes to chat and make sure the patient is completely relaxed.
3. Have the patient hold his or her head at a 45° angle with normal posture.
4. Standing behind the patient, use four fingers of each hand to support the mandible on both sides (Fig. 122).
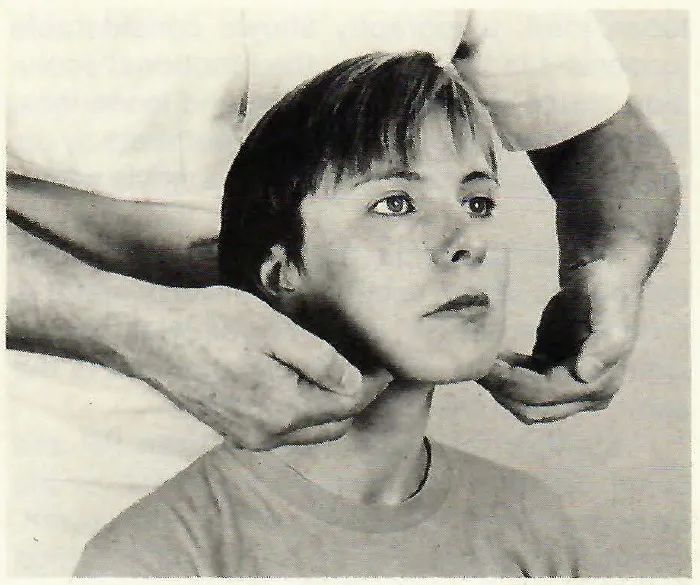
5. Instruct the patient to open and close very slowly.
6. Probe with your fingers so that you feel the patient contact the splint. You are using muscle input to evaluate whether the muscle-ligament-occlusion relationship is harmonious.
7. Gently mark the splint contacts with articulating paper, and correlate the marked spots with what your fingers feel.
8. If the splint is not balanced, have the patient grind the paper momentarily. Avoid doing “tap-tap-tap” grinding, because you and the patient lose control over the procedure. If the balancing takes more than several minutes, take a new reference position interocclusal record and remake the splint.
The original casts were mounted in the reference position of the day they were taken, and verified with the interocclusal records taken the same day. Consequently, a progress interocclusal record can be interposed between the original mounted casts, and M.P.I. can measure the difference between the original and progress reference positions. CADIAX performs the same task using a functional occlusion clutch.
Follow-Up Treatment
Splint therapy is not effective in Class II, division 2 cases and simply wastes valuable treatment time. I proceed immediately to orthodontic treatment in these cases.
After successful splint therapy, a final instrumental analysis must be performed before further treatment. Following the hinge-axis pathways is the only way to create records verifying the proper execution of treatment concepts.
ACKNOWLEDGMENT: Dr. Slavicek and JCO would like to thank William Missert, President of William Missert, Inc., a full-service commercial dental laboratory, and its subsidiary, Gamma Institute USA, for his invaluable assistance in the production of this series.