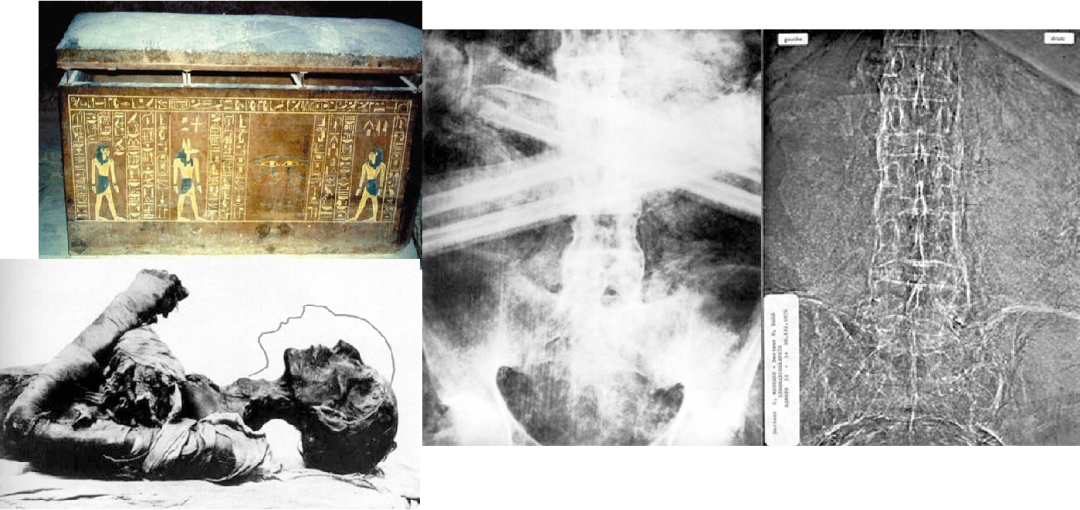
Abstract:The history of axial spondyloarthritis dates back several centuries. Significant achievements have been made since the late 19th century. This historical review attempts to demonstrate how closely the progress in rheumatology clinical medicine is related to advances in basic science.
Ankylosing Spondylitis (from the ancient Greek “vertebra” and ἄγκυλος ‘ankylos’ meaning “bent, curved”; Latinized as ankylosing spondylitis “inflammation of the bent/stiff vertebrae”), also known as ankylosing spondylitis (AS) or Bechterew’s disease or Strümpell-Marie-Bechterew disease, is a chronic inflammatory rheumatic disease characterized by pain and stiffness affecting the axial skeleton. This disease typically begins in the third decade of life, is more common in men than women, and often leads to inflammatory back pain, stiffness, and reduced mobility. According to the 2009 ASAS classification criteria, the name was recently changed to axial spondyloarthritis (axSpA) to better encompass the early disease that theoretically occurs before structural damage to the bones.
Initially, it primarily affects the sacroiliac joints (SIJ) and later often involves the spine. Other manifestations of spondyloarthritis (SpA), such as anterior uveitis, occur in about 1/3 of patients, while psoriasis and inflammatory bowel disease are other associated disease manifestations. Comorbidities such as cardiovascular disease are major causes of complications and mortality. This narrative review, based on four centuries of scientific work on AS and axSpA, provides a highly subjective overview of our understanding of the disease’s history. An appendix lists a timeline of what we consider the most important scientific events.
(1) Early history, pathology, and clinical descriptions
(2) Imaging
(3) Classification criteria
(4) Pathophysiology, including genetics
(5) Measurement of disease activity and response criteria
(6) Different drug treatments

Early History
First Description of Ankylosing Spondylitis
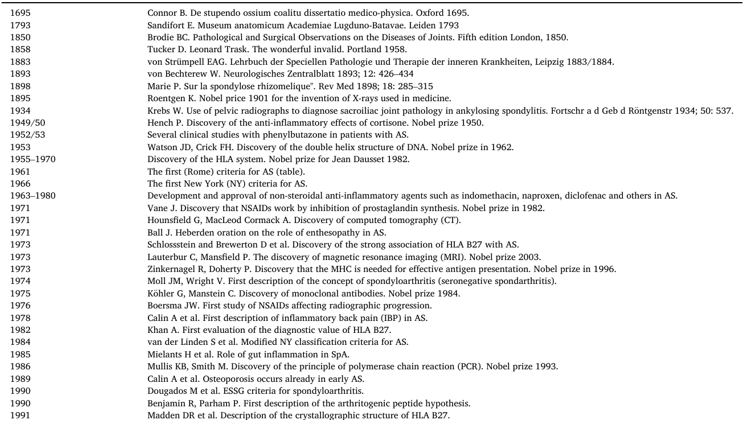
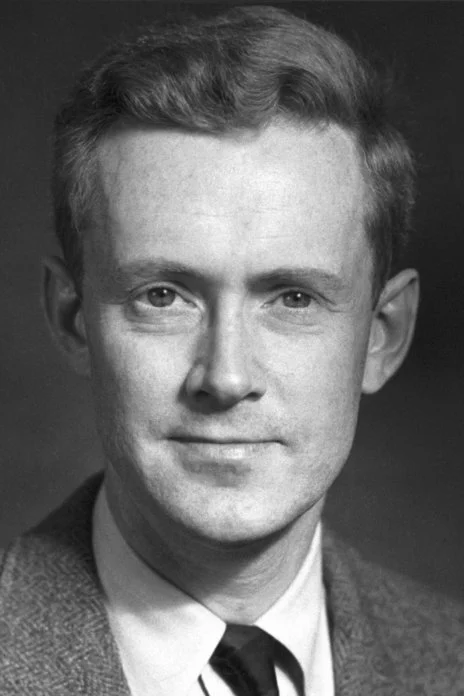
Pharaoh Ramses II of ancient Egypt likely suffered from ankylosing spondylitis.
Pelvic X-rays of Pharaoh Ramses II and others: vertebral bamboo-like changes, sacroiliac joint fusion, likely indicating ankylosing spondylitis, with his mummy in his sarcophagus. What would the head position be if the post-mortem fractures were correctly aligned?
However, today, in some Arab countries, the recognized association of AS with MHC class I molecule HLA B27 is less evident. Regardless, the first scientific publication can be credited to the Irishman B. Connor (1666-1698), who encountered an unusual skeleton in a cemetery during his stay in Paris, which showed clear signs of new bone formation due to AS. His medical doctoral thesis at the University of Reims was published in 1691. At the end of the 18th century, anatomy professor E. Sandifort (1742-1814) published a book at Leiden University, which included photographs of a patient’s fused bones suggestive of ankylosing spondylitis, although the disease was not explicitly mentioned.
Leonard Trask, an American born in 1805, suffered a neck and spine twist from a horse riding accident in his twenties. After several attempts to cure him, he had further accidents that led to increasingly strange postures, resulting in loss of mobility and work, but also making him a spectacle. As published in 1858, his condition remained unresolved until his death in 1861, and he is likely the first recorded patient with AS in America.
Book documenting Leonard Trask’s deformities
When Henry Gray dedicated his work “Gray’s Anatomy” to Sir Benjamin Brodie (1783-1862), the president of the Royal College of Surgeons of England, in 1858, he became the dean of the college. His work “Pathology and Surgical Observations on Joint Diseases” was published in its 5th edition in 1850, providing the first clinical description of the typical manifestations of AS (Chapter 12, Section 4, below page 353).
Brody was also the first to describe iritis (anterior uveitis) as a complication of AS. Decades later, Charles Hilton Fagge (1838-1883), a physician at Guy’s Hospital in London, was the first medical doctor to write an article on AS, describing a case of “simple early closure” in 1877. Adolf von Strümpell (1853-1925), who worked at Leipzig University at the time, described a physical case of AS in an internationally recognized textbook: his “Lehrbuch der Speciellen Pathologie und Therapie der inneren Krankheiten” (two volumes, Leipzig, 1883/1884) has been published in over 30 editions and translated into multiple languages.
Russian neurologist Wladimir Michailowitsch Bechterew (1857-1927) was very similar to his colleague Ivan Pavlov in St. Petersburg, advocating for a scientific understanding of psychological processes. In 1884, he won an 18-month overseas scholarship scientific competition, which brought him together with leading figures in psychology and neurology in Berlin, Leipzig, and Paris, where he received treatment in JM Charcot’s neurology department. In 1893, he became a professor of neurology and psychiatry in St. Petersburg. In 1913, he was dismissed for critical political remarks, but after the October Revolution in 1918, he founded the Brain Research Institute, later named after him. In 1922, he was asked to examine the ailing Lenin (who died in 1924). In 1927, he remained in Moscow as the chairman of the first All-Russian Congress of Neuropathologists and Psychiatrists, at which time Josef Stalin’s personal physician sought his help. Professor Bechterew spent three hours with the General Secretary of the Communist Party of the Soviet Union (CPSU), after which he announced his devastating diagnosis: severe paranoia. A day later, he died, under the care of two doctors belonging to the Russian secret service. His body was cremated without an autopsy, against the wishes of his family. In his most cited publication, not all cases were considered to have AS. Although he believed there was neurological involvement, spinal stiffness was the main symptom in his last three patients, including two women over 50 and the most severe case, a 39-year-old male. Neurologist Pierre Marie (1853-1940), a professor of anatomy at the University of Paris and successor to J.M. Charcot, who was also the head of the neurology department at Hôpital Salpêtrière in Paris, also described cases of AS. In the following years, AS was often referred to as Bechterew-Strümpell-Marie disease.
Imaging
Wilhelm Conrad Röntgen (1845–1923) was a German physicist and university lecturer. He discovered X-rays at the Physics Institute of the University of Würzburg on November 8, 1895. In 1901, when the first Nobel Prize was awarded, he was awarded the Nobel Prize in Physics. This discovery revolutionized medical diagnostics and led to other significant discoveries in the 20th century—for example, Antoine Henri Becquerel (1852-1908) discovered radioactivity in early 1896 in Paris while trying to explain the newly discovered radiation through fluorescence. This led to the observation that uranium salts fluoresce when exposed to light, capable of darkening photographic plates.
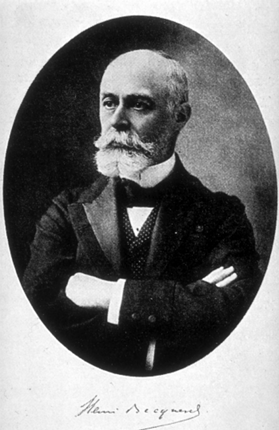
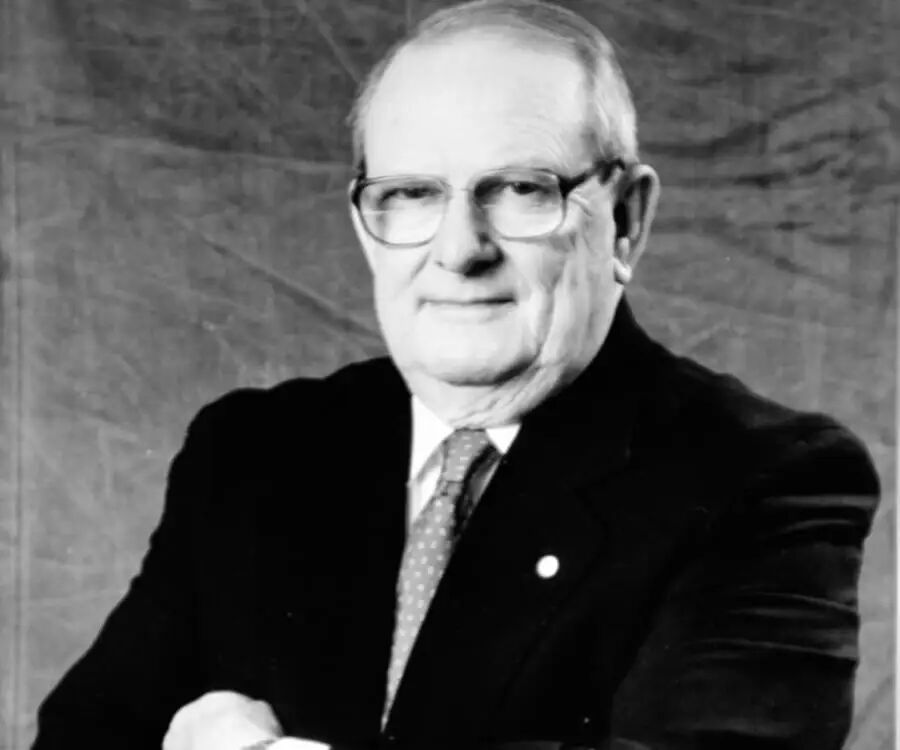
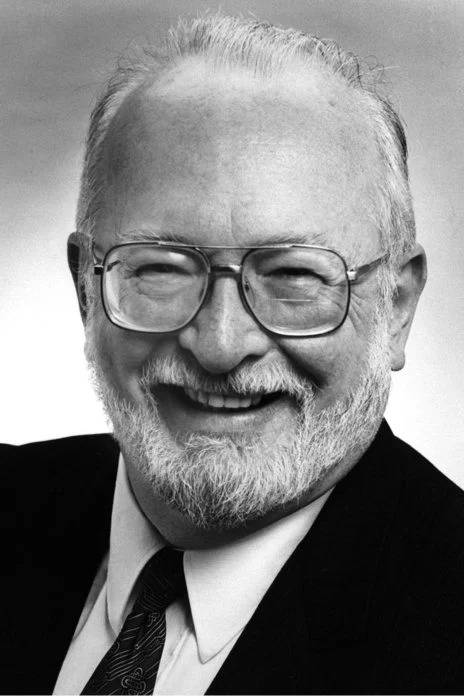
Henri Becquerel (1852–1908)
In 1903, he was awarded the Nobel Prize in Physics along with Marie Curie and Pierre Curie. In the 20th century, X-ray imaging was also used for sacroiliac joints. German rheumatologist W. Krebs discovered that conventional pelvic X-rays could be used to diagnose radiological changes in the sacroiliac joints, which are characteristic of AS. He also reported that typical radiological changes in the SIJ almost always occur in AS patients.
New Imaging Technologies
Two major inventions to mention here are X-ray computed tomography (CT) and magnetic resonance imaging (MRI). Sir Godfrey Newbold Hounsfield (1919-2004), a British electrical engineer, and South African-American physicist Allan MacLeod Cormack (1924-1998) jointly received the Nobel Prize in Physiology or Medicine in 1979 for their development of CT diagnostic technology. His name is “immortalized” in the Hounsfield scale, which is used for the quantitative measurement of radiation density in CT scans, defined in Hounsfield units (HU).

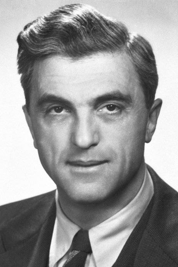
Godfrey Newbold Hounsfield Allan MacLeod Cormack
MacLeod Cormack mentioned after the award: “It is no exaggeration to say that Hounsfield and I could write our understanding of medicine and physiology on a small prescription pad.
Currently, the use of CT is not as prevalent as MRI, but CT remains the gold standard for detecting SIJ erosion, while low-dose CT is a method for detecting spinal pathological changes, such as bone spurs in AS patients. The major drawback has always been radiation exposure, but using low-dose techniques seems to have largely mitigated this issue.
The scientific principle behind MRI is a physical phenomenon in which atomic nuclei in a strong constant magnetic field are disturbed by a weak oscillating magnetic field and respond by producing electromagnetic signals characteristic of the atomic nuclei’s magnetic field frequency—known as nuclear magnetic resonance (NMR). For this discovery, Felix Bloch and Edward Purcell were awarded the Nobel Prize in Physics in 1952.
Felix Bloch Edward Purcell
American chemist Paul Christian Lauterbur (1929-2007) and British physicist Sir Peter Mansfield (1933-2017) jointly received the Nobel Prize in Physiology or Medicine in 2003 for their contributions to the development of MRI. Lauterbur may have conceived the idea of MRI one day while brainstorming in a restaurant in the suburbs of Pittsburgh when he was a student and researcher at the University of Pittsburgh and the Mellon Institute of Industrial Research, where the first model of MRI was sketched on a napkin. He first referred to it as imaging technology.

Paul Christian Lauterbur Peter Mansfield
Mansfield invented the “slice selection” for MRI, which allows selective imaging of axial slices of the subject rather than imaging the entire subject. His understanding of how to mathematically analyze radio signals from MRI enabled these signals to be interpreted into useful images. He also discovered how to form images quickly by developing an MRI protocol called echo planar imaging. The State University of New York chose not to seek a patent due to cost issues, but the University of Nottingham did apply for a patent, which later made Mansfield wealthy. MRI is now part of the axSpA classification criteria and is a mature standard technique for detecting SIJ inflammation and structural changes in clinical practice and clinical research, as shown in the first study in 2000. The advantage of MRI in detecting sacroiliitis in patients without radiological changes in the SIJ was first confirmed in 1994 and later in 1998 in AS patients.
Since 2003, we have realized that not only inflammatory changes in the SIJ (bone marrow edema) but also structural changes contribute to the assessment, diagnosis, and classification of axSpA.
Imaging Progress
To quantify imaging progress, a scoring system was provided in 2005, the modified Stoke AS spine score (mSASSS).
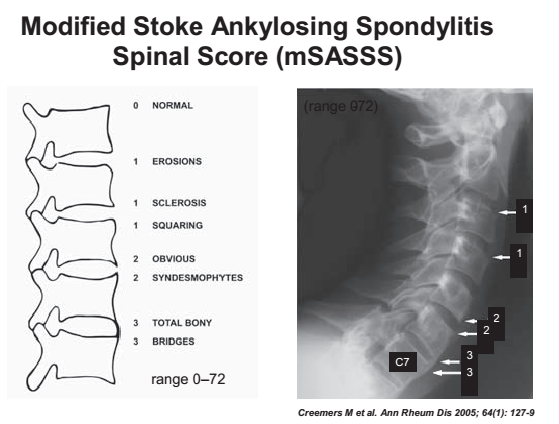
A few years later, the first systematic study comparing two interventions was published. The comparison between two NSAID-based strategies (mainly celecoxib) (continuous administration vs. on-demand administration) showed that the former was associated with less radiographic progression. This result was later confirmed in a post-hoc analysis, indicating that patients with elevated CRP levels had lower mSASSS change scores after continuous treatment. In a similar study design, but using diclofenac, these results could not be confirmed. The OASIS (AS International Study Outcomes) produced imaging progression results in a cohort of 186 patients, showing that the progression process varied greatly among individual patients, with an average annual progression rate of nearly 1.0 mSASSS U/year. Imaging progression was significantly accelerated in male, HLA-B27 positive patients and those with baseline mSASSS ≥10. Further analysis indicated that this rate largely depended on disease activity. For every 1 unit increase in ASDAS, mSASSS would increase by 0.72 units over two years. Over the years, increasing evidence has shown that TNFi has an inhibitory effect on imaging progression.
According to the only head-to-head study conducted so far in axSpA, this may be similar to IL-17i. The impact of JAK inhibitors on imaging progression in axSpA appears to be similar. Many clinical trials have shown that the clinical effects of bDMARDs are related to the reduction of axial inflammation. The first study published in 2008 indicated that axial inflammation seen on MRI is a risk factor for new bone formation. Fatty degeneration also plays a role in the development of new bone formation. Currently, several methods can improve the performance of MRI in axSpA. ASAS has proposed several updated recommendations on how to handle MRI, two of which were only recently proposed. Importantly, not only new bone formation but also osteoporosis and low bone density can be seen in both early and late stages of axSpA. Therefore, the prevalence of spinal fractures in AS is certainly increased.
Classification Criteria
Diagnosis and Classification Criteria for Ankylosing Spondylitis
All published AS, SpA, and axSpA criteria to date are not diagnostic criteria but classification criteria. The first criteria established in Rome (Table 1) were quite good as they included a history of inflammatory back pain, physical examination of the SIJ, and imaging studies (Table 1). The criteria also allowed for the inclusion of imaging-negative patients. The next modification of the criteria was conducted in 1966 in New York, which focused more on X-ray criteria, followed by the assessment study by Moll & Wright in 1973 and the revised New York criteria proposed by van der Linden in 1984.
Table 1. Diagnostic Criteria for Ankylosing Spondylitis (Rome, 1961)
Interestingly, Moll and Wright suggested that the criteria be numerically weighted, as the finding of thoracolumbar pain was too sensitive and nonspecific, while chest and back mobility restrictions were too insensitive and nonspecific. The authors of the revised New York criteria in 1984 (Table 2) believed that, according to the final recommendations, radiological sacroiliitis is a necessary condition for diagnosing AS, as the sacroiliac joints are normal in <1% of typical AS patients. However, they emphasized that sacroiliitis is not limited to AS and may also occur in psoriatic arthritis, Reiter’s syndrome, and even rheumatoid arthritis.
Table 2. Revised New York Criteria for Ankylosing Spondylitis (1984)
The authors concluded that the lumbar pain criteria lack specificity, and the chest expansion criteria are too insensitive. However, studies have found that the Rome criteria for low back pain lasting >3 months are very useful. Current studies indicate that clinical history as a screening test for AS has only moderate sensitivity. As a modification of the New York criteria, it has been proposed to replace the New York pain criteria with the Rome pain criteria. The clinical criteria for “inflammatory back pain” first published in 1977 include chronic (>3 months) and age of onset (<40 years), further characterized by morning stiffness in the lower back >30 minutes, insidious onset, and improvement with exercise rather than rest. The 1984 revised New York criteria and later proposals also included modifications to this definition. In 1974, Moll and Wright published a publication in which the concept of SpA was first classified as “seronegative spondyloarthritis.” They proposed to group these seven entities together: AS, psoriatic arthritis, reactive arthritis, arthritis associated with Crohn’s disease and ulcerative colitis, as well as Whipple’s disease and Behçet’s syndrome. The latter two are no longer considered part of the SpA spectrum.
Belgian researchers H. Mielants conducted several clinical studies using ileocolonoscopy, which showed that a significant proportion of SpA patients had intestinal inflammation similar to Crohn’s disease, but most of these patients were asymptomatic. The first attempt to broaden the scope of AS was almost simultaneously conducted by B. Amor, who initiated the activities of the European Spondyloarthritis Study Group (ESSG), which established criteria for what is now referred to as spondyloarthritis. The aim was to include all manifestations of SpA, such as axial manifestations, seronegative oligoarthritis or lower limb polyarthritis, dactylitis, and other undifferentiated SpA cases, importantly, heel pain caused by enthesitis, as J. Ball had already indicated in his Heberden lecture in 1970, later emphasized again in D. McGonagle’s MRI studies.
However, the two main criteria in the ESSG criteria are inflammatory back pain or synovitis (asymmetrical or predominantly occurring in the lower limbs), along with at least one of the following: positive family history, psoriatic inflammatory bowel disease, urethritis or acute diarrhea, alternating buttock pain, enthesitis, or sacroiliitis determined by X-ray.
The Assessment of SpondyloArthritis International Society (ASAS) group published new classification criteria for axSpA in 2009 (Table 3), incorporating clear MRI findings and HLA B27, including patients before structural lesions occur in the SIJ. Currently, the ASAS group is collaborating with the Spondyloarthritis Research and Treatment Network (SPARTAN) to investigate whether these criteria can be improved by achieving higher specificity. The recently reported uncertainty in disease diagnosis also reflects the new criteria placing HLA-B27 and MRI in a prominent position. In this paper, it was reported that nearly one-third of patients with chronic back pain were reliably diagnosed with axSpA, but even after two years, 5% to 30% of patients still had diagnostic uncertainty.
Table 3. 2009 ASAS Classification Criteria for Axial Spondyloarthritis (SpA)
Pathophysiology, Including Genetics
Major Histocompatibility Complex
The major histocompatibility complex (MHC) is an extended gene on vertebrate DNA that contains a set of closely linked polymorphic genes that encode cell surface proteins that have fundamental functions in the adaptive immune system. These cell surface proteins are known as MHC molecules and come in different classes. Jean Dausset first demonstrated the existence of MHC genes in humans and described the first human leukocyte antigen (HLA), which we now refer to as HLA-A2, a class I antigen similar to HLA B27. He was awarded the Nobel Prize in 1980. The name of the gene (MHC) comes from its discovery through studies on transplant tissue compatibility. However, the main function of MHC molecules is to bind antigens from different sources, including self-proteins and pathogens, and present the antigens to the cell surface for appropriate T cell recognition. MHC determines the donor compatibility for organ transplantation and also plays a role in susceptibility to autoimmune diseases. The role of MHC in antigen presentation was discovered by R. Zinkernagel and P. Doherty, who were awarded the Nobel Prize in 1996 for this work.
HLA-B27 and Other Genes
For a long time, AS has been considered a highly heritable disease, with many patients having a positive family history. As first reported in 1973, the class I surface molecule HLA-B27, encoded by the B locus in the MHC on chromosome 6, is closely associated with AS and is also closely related to inflammatory diseases such as reactive arthritis and anterior uveitis.
The physiological function of HLA molecules such as HLA-B27 is to present peptides derived from self-antigens and/or non-self-antigens to T cells. The current main hypothesis is the arthritogenic peptide theory, which is based on the assumption that CD8+ T cells recognize pathogenic peptides (such as microbial antigens) derived from self and/or non-self. An important argument supporting this research comes from GWAS studies that identified two new genetic loci for AS, namely the tumor necrosis factor receptor 1 (TNFR1) shedding aminopeptidase regulator (ARTS1) and interleukin (IL)-23 receptor (R), which also plays a role in Crohn’s disease. The former is now referred to as endoplasmic reticulum (ER) aminopeptidase 1 (ERAP1), which is involved in the antigen processing and presentation pathway. ERAP1 is primarily located in the ER, where it trims peptides at the N-terminus to fit the pre-processing of MHC class molecules. Importantly, ERAP1 polymorphism is only associated with HLA-B27+ AS.
Crystallography made significant strides, a technique that had been studied shortly after the invention of X-rays, aiding in the detection of the double helix structure of DNA and the first crystal structure of the large molecule myoglobin.
Studies of the structure of HLA-B27 through crystallography showed that polymeric self-peptides (9 amino acids) exist in the molecular B pocket groove, with arginine at position 2. Shortly thereafter, synovial cloning experiments indicated that the immune response suppressed by HLA-B27 might indeed play a role, later identifying self-peptides derived from cartilage and other peptides. Alternative hypotheses for the pathogenic role of HLA-B27 have been proposed. P. Bowness suggested the possible role of free HLA-B27 heavy chains, which form disulfide-linked dimers lacking β2-microglobulin, relying on residues Cys67 in its extracellular α1 domain and its innate immune receptors.
HLA-B27 molecules also show misfolding during the assembly process in the endoplasmic reticulum, which may lead to intracellular stress and autophagic responses as described by R. Colbert. Recently, the selection of a TCR-driven yeast display library based on HLA-B*27:05 identified self-antigens and microbial antigens recognized by common TRBV9 CD8 TCR derived from synovial fluid and blood of AS patients. This finding further supports the arthritogenic peptide hypothesis. However, to date, the exact mechanism by which HLA-B27 leads to diseases such as axSpA remains undetermined.
As early as 1990, there was hope that the HLA-B27 transgenic rat model, which simultaneously expresses HLA-B27 and human β2-microglobulin, could help find clues to the pathogenesis. In fact, transgenic rats with high copy numbers of HLA-B27 develop spontaneous inflammatory diseases in SpA-related organs (joints, spine, gut, and skin). The most impressive finding remains that these animals showed no disease symptoms under sterile conditions. This is now the basis for microbiome-related studies in SpA patients. The first statistical assessment of the diagnostic value of HLA-B27 testing for AS was published in 1982 and remains relevant.
Polymerase Chain Reaction
Polymerase chain reaction (PCR) is a laboratory method that can rapidly produce billions of copies of specific DNA samples, thereby amplifying very small DNA or RNA samples, even a portion sufficient to prove its existence. This has significant implications for nearly all fields of medicine. The technique was invented in 1983 by American biochemist Kary Mullis (1944-2019) at the biotechnology company Cetus Corporation. Mullis and British-Canadian biochemist Michael Smith (1932-2000), professors in the Department of Biochemistry at the University of British Columbia (UBC), developed other fundamental methods of DNA manipulation and jointly received the Nobel Prize in Chemistry in 1993. After working in a DNA laboratory for seven years, Mullis successfully demonstrated the effectiveness of the PCR technique on December 16, 1983. In his Nobel Prize speech, he stated that this breakthrough did not compensate for the breakup with his girlfriend. Mullis experienced several interruptions in his career and did not truly obtain a prominent university position. However, he received $10,000 from his company, which sold the patent for $300 million to Roche Molecular Systems. Smith made significant contributions to the establishment of site-directed mutagenesis based on oligonucleotides and its development in protein research.
From 1975 to 1976, Smith worked with Nobel laureate F. Sanger at the MRC Molecular Biology Laboratory in the UK, standing at the forefront of gene and genome organization research. He, along with Sanger, introduced a technique called oligonucleotide-directed site-specific mutagenesis. This addressed the issue of how to effectively determine the impact of single mutated genes. Introducing site-specific mutations into genes required the development of synthetic DNA technology. A similar technique, in situ hybridization (ISH), had been described in the late 1960s. This is a hybridization that uses labeled probes (such as complementary DNA, RNA, or modified nucleic acid chains) to locate specific sequences in a part or portion of tissue.
PCR technology has greatly transformed the diagnostic potential of medical research. In rheumatology, the ability to identify very small amounts of microbial DNA or RNA has become crucial, such as in Lyme arthritis or Whipple’s disease. Additionally, HLA alleles, such as HLA-B27, can be distinguished through PCR rather than FACS. ISH can detect inflammatory cytokines in inflammatory tissue biopsy specimens.
The geographical distribution of HLA-B27 primarily follows a north-south decline. Thus, the prevalence of HLA-B27 in Nordic and Eskimo populations is as high as 25%, while in some regions of Africa, it is less than 3%. This may be due to the strong ability of HLA-B27 to present viral peptides.
PCR technology can identify allele subtypes, most of which have very small amino acid differences. In Europe, the main subtypes are HLA-B2702 and HLA-B2705. This varies in other countries, such as China, where HLA-B2704 is dominant. All three subtypes are associated with AS. However, studies have found that the HLA-B2706 subtype found in Thailand and the HLA-B2709 subtype found in Sardinia are not associated with AS. The reasons for this are unclear, but there is some evidence that peptide groups may differ. Although the pathogenesis of axSpA has not yet been elucidated, it seems clear that genes such as HLA-B27, ERAP-1, and IL-23R contribute significantly. Additionally, the role of mechanical stress on the joints has been a focus of research, including the connection between inflammation, responsible cytokines, and new bone formation, including issues of bone immunology. Many interesting papers and hypotheses have been published in this area over the past decade.
The Impact of Physical Labor and Exercise
There is currently ongoing discussion regarding the impact of exercise and physical labor on imaging progression and function. According to a recent study from Norway, while physical labor may have negative effects (indicating more new bone formation), exercise may even lead to reduced disease activity. In another axSpA cohort, higher levels of daily physical activity (PA) were associated with better patient-reported outcomes and lower depression scores.
Assessment Tools
New Assessment Tools
Not only the development of clinical research in this field but also an important step for daily practice was the introduction of the first standard to assess AS disease activity and function. The AS International Society (ASAS) assessment foundation occurred in late 1995. An important step forward was the development of a new disease activity score, the ASDAS, followed by a consensus recommendation on different cut-off values. The development of the ASAS Health Index (HI) was a lengthy process based on discussions within ASAS regarding the severity of axSpA. It combines different concepts of pain, function, and structural damage (imaging progression). The recently updated axSpA core outcome set indeed includes seven mandatory domains for all trials: disease activity, pain, morning stiffness, fatigue, physical function, overall function, and health status, as well as adverse events, including mortality. Additionally, three extra domains must be assessed for improvement in disease-modifying antirheumatic treatment (important but optional): musculoskeletal manifestations, peripheral manifestations, and structural damage. Finally, three additional domains: spinal mobility, sleep, work, and employment, are defined as important but optional assessment dimensions in all trials.
Drug Treatments
Acetylsalicylic Acid (Aspirin)
For centuries, salicylic acid or salicin found in willow bark has been known to relieve pain. The field of effective pharmacotherapy began as early as 1853 when acetylsalicylic acid (ASS) was first mentioned in the chemical literature by French chemist Charles F. Gerhardt. However, the true birth of ASS occurred on August 10, 1897, when Bayer chemist Felix Hoffmann recorded the pure isolation of ASS in his laboratory notebook. It took only a year from synthesis to the first clinical application. Another year passed before the trademark was registered, thus beginning commercial release. On February 1, 1899, aspirin was registered as a trademark at the Berlin Patent Office, registration number 36,433. Since 1899, Bayer has extensively promoted aspirin. This substance is now considered one of the most commercially successful brands in pharmaceutical products.
Corticosteroids
Between 1935 and 1940, two different research groups isolated cortisone from animal adrenal cortex and conducted different labeling. This research was led by Edward Calvin Kendall of the Rochester Mayo Foundation and Ukrainian refugee Tadeusz Reichstein of the Swiss Federal Institute of Technology in Zurich. Cortisone was later found to be an oxidized product of the hormone cortisol. The partial synthesis of cortisone from deoxycholic acid was first achieved at Merck Laboratories during World War II. In 1948, physician Philip S. Hench (1896-1965) managed to obtain 9g of cortisone “for research purposes.” His colleagues at the Mayo Clinic, Charles Slocumb and Howard Polley, first injected 100 mg of “compound E” into a severely RA patient in September 1948, who had not experienced pain for the first time in years. Two years later, in 1950, Kendall, Reichstein, and Hench jointly received the Nobel Prize in Medicine for their discovery of adrenal cortex hormones, their structure, and biological effects. Early studies on the use of cortisone in AS achieved some success. However, at the same time, it can be said that the evidence for the efficacy of prednisone in AS is quite limited, as the required doses are too high, and the effects do not last.
The First Non-Steroidal Anti-Inflammatory Drug
Since the early 1950s, several non-steroidal anti-inflammatory drugs (NSAIDs) have been developed and approved (initially not explicitly for AS, as it was not yet recognized as an entity but mixed with RA as rheumatoid spondylitis). NSAIDs are quite effective in treating AS. The earliest reports were on phenylbutazone (Geigy patent), followed by indomethacin, naproxen, diclofenac, etc. It was known early on that gastrointestinal toxicity was the most important adverse event. Phenylbutazone was very effective in treating active AS and is still sometimes used today, but due to rare but quite serious adverse events (such as agranulocytosis), it is only used under very strict indications. NSAIDs are currently recommended as first-line treatment for active axSpA internationally. A good response to NSAIDs is considered a possible hint for diagnosing axSpA.
In addition to clinical efficacy, the first hint that NSAIDs might have an inhibitory effect on bone formation in AS was published in 1976 in a relatively small study with limited methodological strength.
The Role of Prostaglandins in Inflammation and the Inhibition of Cyclooxygenase-1 and 2
Until the 1970s, high doses of ASS were used in severe cases of RA and other diseases, even exceeding 5g/day. However, for unclear reasons, ASS seemed to have poorer effects on AS compared to other inflammatory rheumatic diseases. Decades later, Sir John Robert Vane (1927-2004), professor of experimental pharmacology in London, discovered that ASS works by inhibiting prostaglandins. He was awarded the Nobel Prize in Medicine in 1982. Nearly a decade later, two types of cyclooxygenase (COX) were discovered: one is the constitutive COX-1, usually present in most cells and tissues, unresponsive to glucocorticoids, while the other is the inducible COX-2, expressed only in inflammatory cells (such as macrophages) during inflammation and regulated by glucocorticoids. This initiated a fierce competition over who had the best selective drugs for COX-2. Initially, rofecoxib seemed to win the game with fewer gastrointestinal side effects, but its cardiac toxicity in high-risk patients was overlooked, and the OTC (over-the-counter) activity threatened many lawsuits—leading to its withdrawal from the market globally in 2004. It later became increasingly clear that cardiac toxicity applies to all non-steroidal anti-inflammatory drugs, with naproxen generally having the lowest risk, possibly due to its inhibitory effect on platelet aggregation.
Production of Monoclonal Antibodies
The hybridoma technology used to produce monoclonal antibodies represents one of the most significant methodological advances in biomedicine. The cells producing antibodies and all their progeny produce the same antibody molecule (monoclonal antibodies). For a long time, scientists hoped to produce monoclonal antibodies with predetermined specificity. In 1975, when Georges J.F. Köhler (1946-1995) and César Milstein (1927-2002) described the hybridoma technology for producing monoclonal antibodies, this dream became a reality. They immortalized these cells by fusing antibody-producing cells with tumor cells. This method allows for the unlimited production of monoclonal antibodies with predetermined specificity. Monoclonal antibodies have opened up new fields in theoretical and applied biomedical research, allowing for precise diagnosis and treatment of diseases. In 1984, Köhler and Milstein were awarded the Nobel Prize for their work. Hybridoma technology has opened up new fields of medical treatment, including rheumatology. We are very fortunate to be part of this revolution in rheumatology treatment.
Treatment with New bDMARDs and tsDMARDs
The first 25 years of the 21st century have been characterized by clinical trials using monoclonal antibodies and fusion proteins targeting pro-inflammatory cytokines. This is particularly important for axSpA, as traditional synthetic (cs) DMARDs do not work for axial diseases compared to RA.
After proving that TNF is expressed in the SIJ of AS patients, the next step supported by the German Rheumatology Research Center (DRFZ) led by A. Mitchison and later A. Radbruch was to treat these patients with anti-tumor necrosis factor (TNF) antibodies, which was fundamentally successful in an open pilot study, later confirmed in a placebo-controlled multicenter study. At the same time, studies showed that TNFi could improve not only colitis but also Crohn’s disease.
A few years later, a study from Leeds reported higher response rates in patients (under 30 years, symptom duration <2 years) with all HLA-B27 and MRI-determined axial inflammation—this study recruited an early axSpA patient group for clinical research. A total of five TNF inhibitors approved for AS have been studied: infliximab, etanercept, adalimumab, golimumab, and certolizumab pegol, with the first three biologicals already approved.
After failures with anti-IL-1, anti-IL-6, and anti-IL-23, the next successful study was with the anti-IL-17 antibody secukinumab, followed by ixekizumab and most recently bimekizumab. Later, targeted synthetic (ts) DMARDs were also shown to be effective for axSpA: JAK inhibitors such as tofacitinib, filgotinib, and upadacitinib. Importantly, these drugs are effective for axSpA patients, including both r-axSpA and nr-axSpA, and have been approved by EMA and FDA.
The first study indicated that bDMARDs, in this case, TNFi, are effective not only in AS but also in nr-axSpA as early as 2013. The first study combined two indications, r-axSpA and nr-axSpA, with another TNFi in a clinical trial, which appeared only a year later.
So far, only one study has followed the principles of targeted therapy. Data indicate that this strategy is superior to standard regimens, although not the primary outcome.
Conclusion
In summary, the history of axSpA has seen new developments, primarily driven by technological discoveries such as X-rays, MRI, MHC, and HLA-B27, closely followed by PCR and monoclonal antibody technologies paving the way for these achievements. We hope this data will help young rheumatologists understand how scientific progress is made. In the early days, clinical observations and pathology were the most important. Since the last century, technological advances have primarily driven our understanding of the disease. The strong heritability and the association of axSpA and AU with HLA-B27 remain prominent phenomena that must be fully understood to elucidate the pathogenesis of these diseases. Similarly, the role and contribution of psoriasis and IBD also need to be clarified. The recently reported uncertainty in diagnosing diseases reflects the current standards placing HLA-B27 and MRI in uncertain positions. In fact, the specificity of both HLA-B27 and MRI tests for early diagnosis is limited. The focus in the coming years will clearly include these issues. This obviously includes the differences observed between male and female patients in several aspects.
According to the Rome criteria proposed in 1961, a diagnosis of ankylosing spondylitis should be made when there is bilateral sacroiliitis and one of five clinical criteria, or when there are four clinical criteria present. Therefore, using these criteria, a diagnosis/classification without radiological evidence of disease was made over 60 years ago. However, the term nr-axSpA should not be used for diagnosis but only for classification.

References
1. Braun J, Sieper J, Dougados M. The history of ankylosing spondylitis/axial spondyloarthritis– what is the driving force of new knowledge. Semin Arthritis Rheum. 2025,71:152611.
2. Rudwaleit M, van der Heijde D, Landew´e R, et al. The development of assessment of SpondyloArthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 2009,68(6):777–783.
3. Schuchart S. Famous discoverers of diseases: the life and sudden death of Wladimir M. Bechterew. Dtsch Arztebl 2020,117(25):40.
4. Jonsson BA. Henri Becquerel’s discovery of radioactivity – 125 years later. PhysMed 2021,87:144–146.
5. de Koning A, de Bruin F, van den Berg R, et al. Low-dose CT detects more progression of bone formation in comparison to conventional radiography in patients with ankylosing spondylitis: results from the SIAS cohort. Ann Rheum Dis 2018,77(2): 293–299.
6. Baraliakos X, Østergaard M, Poddubnyy D, et al. Effect of secukinumab versus adalimumab biosimilar on radiographic progression in patients with radiographic axial spondyloarthritis: results from a head-to-head randomized phase IIIb study. Arthritis Rheumatol 2024,76(8): 1278–1287.
7. Baraliakos X, Østergaard M, Lambert RG, et al. MRI lesions of the spine in patients with axial
spondyloarthritis: an update of lesion definitions and validation by the ASAS MRI working group. Ann Rheum Dis 2022,81(9):1243–1251.
8. Marques ML, Ramiro S, van Lunteren M, et al. Can rheumatologists unequivocally diagnose axial
spondyloarthritis in patients with chronic back pain of <2 years duration? Primary outcome of the 2-year SPondyloArthritis Caught Early (SPACE) cohort. Ann Rheum Dis 2024,83(5):589–598.
9. Barkham N, Keen HI, Coates LC, et al. Clinical and imaging efficacy of infliximab in HLA-B27-positive patients with magnetic resonance imaging-determined early sacroiliitis. Arthritis Rheum 2009;60(4):946-954.
10. van der Heijde D, Deodhar A, Baraliakos X, et al. Efficacy and safety of bimekizumab in axial spondyloarthritis: results of two parallel phase 3 randomized controlled trials. Ann Rheum Dis 2023,82(4): 515–526.
11. van der Heijde D, Baraliakos X, Gensler LS, et al. Efficacy and safety of filgotinib, a selective Janus kinase 1 inhibitor, in patients with active ankylosing spondylitis (TORTUGA): results from a randomized, placebo-controlled, phase 2 trial. Lancet 2018,392(10162):2378–2387.
Yimaitong is a professional online doctor platform, with the mission of “perceiving the pulse of world medicine and assisting clinical decision-making in China.” Yimaitong has a series of products including “Clinical Guidelines,” “Medication Reference,” “Medical Literature King,” “Medical Knowledge Source,” “e-Research Communication,” and “e-Pulse Broadcasting,” fully meeting the needs of medical practitioners for clinical decision-making, acquiring new knowledge, and improving research efficiency.
