
The liver is one of the most important organs for maintaining life activities in the human body, being the largest digestive gland and the organ with the most active metabolism. It undertakes extremely important and complex functions, such as: synthesis and storage, bile secretion, detoxification, defense, and hematopoietic functions. The liver reserve function is an indicator for assessing the liver’s potential, reflecting its compensatory ability when the internal and external environment is imbalanced. The most prominent characteristic of the liver, unlike other organs, is its strong regenerative ability; a normal liver can tolerate the removal of 70% without significant physiological dysfunction, providing unlimited possibilities for partial hepatectomy in the treatment of liver diseases.
For patients with different grades of liver function, the ability to undergo liver resection and the choice of surgical methods vary. Correctly assessing the liver reserve function and the resectability of liver cancer before surgery helps accurately determine the amount of liver to be removed during the operation and reduces the incidence of post-hepatectomy liver failure (PHLF). Currently, there are various preoperative assessment methods for liver surgery, including routine biochemical tests, clinical scoring systems, imaging examinations combined with three-dimensional reconstruction technology, and dynamic liver function tests. This article will review the advantages and disadvantages of commonly used clinical preoperative assessment methods.

1Routine Biochemical Tests
Routine serum biochemical tests are the simplest, most commonly used, and economical means of assessing liver function. Different serological indicators can reflect liver function from different perspectives. Currently, under the influence of precision medicine, the application of combined serological indicators to assess liver function has become more important.
1.1 Albumin (Alb) and Serum Prealbumin (PA)
Both are primarily synthesized by the liver and can reflect the synthetic function of the liver to some extent, but each has its differences. Alb has a long half-life of 3 to 4 weeks, which means that the Alb level measured clinically reflects liver function with a delay. A decrease in Alb is also related to many other factors such as: lesions in liver cells, lack of amino acid supply, increased protein consumption, gastrointestinal losses, etc., which reduce the sensitivity of Alb in reflecting liver function reserve. In comparison, PA has a shorter half-life of about 1.9 days, making it more sensitive for reflecting liver synthetic function. Some studies suggest that dynamically observing PA is of significant value in predicting the prognosis of liver disease, but many factors still affect PA, such as trauma, infection, biliary diseases, and liver abscesses.
1.2 Bilirubin
Bilirubin reflects the liver cell’s uptake, conjugation, transformation, and excretion functions, serving as both an indicator of liver cell damage and liver function. It is divided into conjugated and unconjugated bilirubin; isolated elevation of the former is common in biliary obstruction diseases, while isolated elevation of the latter is often seen in hemolytic diseases. Both significantly higher than normal values suggest hepatocellular jaundice. Thus, the accuracy of bilirubin in reflecting liver function is influenced by hemolysis, biliary obstruction, and other factors.
1.3 Hyaluronic Acid
Hyaluronic acid is essentially a mucopolysaccharide produced by liver tissue stromal cells, which can be degraded into acetate and lactate by liver sinusoidal endothelial cells. In patients with liver diseases, especially cirrhosis, serum hyaluronic acid levels are significantly elevated and correlate strongly with the degree of liver damage. Therefore, the level of serum hyaluronic acid reflects the function of liver endothelial cells and has significant clinical importance for diagnosing the degree of liver fibrosis and cirrhosis. The normal value of serum hyaluronic acid is <120.0 ng/mL; some scholars suggest that a serum hyaluronic acid level greater than 400 ng/mL is a standard for liver damage. Wang et al. proposed a combination of hyaluronic acid with magnetic resonance imaging technology HA-Target-Cy5.5-DOTA-Gd (HTCDGd) for accurate staging of liver fibrosis.
1.4 Type IV Collagen 7S
Type IV collagen is a basement membrane protein located around liver sinusoids and serves as an immunohistochemical marker for the basement membrane. In normal liver, there is no basement membrane around the sinusoids; however, when liver fibrosis occurs, capillarization appears, and the basement membrane forms, leading to an increase in type IV collagen 7S in the blood. Ishii et al. found that for long-term recovery of liver function post-surgery, the recovery time for the group with preoperative type IV collagen 7S ≤6 ng/mL was significantly shorter than for the group with preoperative type IV collagen 7S >6 ng/mL. Preoperative type IV collagen can predict early liver failure in different subgroups of patients undergoing liver resection and influence long-term recovery of liver function post-surgery.
1.5 Other Serological Indicators
ALT and AST are markers of liver damage associated with hepatocyte necrosis; the higher the degree of liver damage, the higher the liver enzymes. However, the elevation of liver enzymes does not accurately reflect liver function. The liver can synthesize various clotting factors such as V, VII, VIII, IX, X, XI, and XII, so the levels of clotting factors in the blood can reflect liver function to some extent. Prothrombin time (PT) and International Normalized Ratio (INR) are currently commonly used liver function indicators, often used in combination with other indicators or as part of scoring systems. Antithrombin III is a glycoprotein produced by the liver that can inactivate some enzymes in the coagulation system. Mizuguchi et al. found a correlation between antithrombin III and liver function indicators such as Alb, bilirubin, PT, and indocyanine green retention rate (ICG-R15) in 158 patients undergoing liver resection for hepatocellular carcinoma. Additionally, reports suggest that other serological indicators such as Mac-2 binding protein glycosylation isomers, type I collagen, and tissue inhibitors of metalloproteinases have clinical significance in predicting the occurrence of post-operative PHLF.

2Imaging Assessment Methods
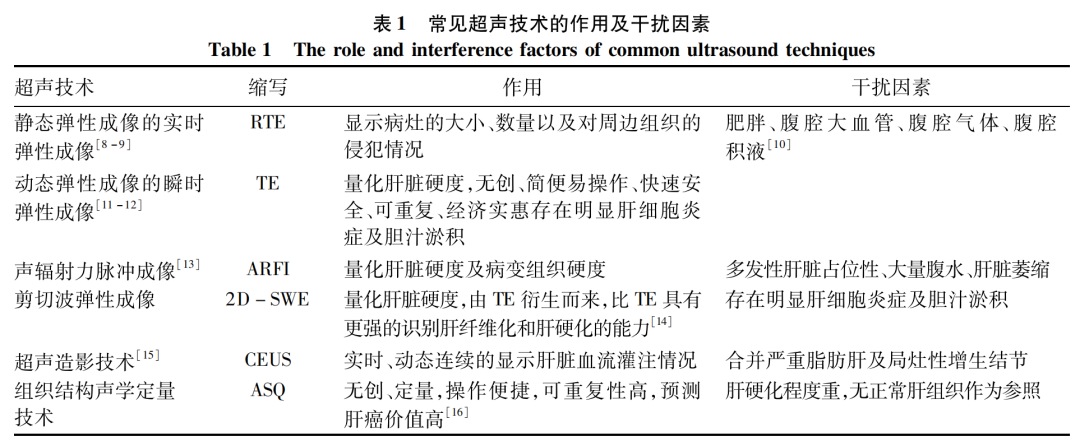
2.1 Ultrasonography
Ultrasound is one of the initial screening methods for liver diseases, and commonly used ultrasound techniques are shown in Table 1.
2.2 CT and 3D Reconstruction Technology
Preoperative liver function and the volume of the remaining liver significantly affect postoperative liver function recovery. Measuring the volume of the remaining liver preoperatively helps predict the occurrence of PHLF. Through CT perfusion imaging and three-dimensional reconstruction technology, the total liver volume and tumor volume can be measured, and the volume of the remaining liver can be accurately calculated to achieve the purpose of preoperative assessment of liver cancer resectability. The widespread application of three-dimensional reconstruction technology is also attributed to the development of the concept of “precision hepatectomy”. Recent studies have shown that CT three-dimensional reconstruction technology can visually and clearly display the liver’s anatomical structure and tumor status, assess the invasion of tumors into intrahepatic blood vessels, bile ducts, and other complex conduits, thus obtaining a more accurate preoperative assessment. Guo et al. studied 120 patients undergoing laparoscopic liver resection and found that preoperative assessment of tumor volume using CT three-dimensional reconstruction technology significantly reduced intraoperative bleeding and shortened hospital stay. The estimated pre-resection liver volume and actual resection liver volume were significantly lower in the observation group compared to the control group, while the remaining liver volume was significantly larger than that of the control group, with no significant differences in estimated and actual lesion volumes between the two groups. Lamadé et al. reported that using three-dimensional images for preoperative tumor assessment improved the accuracy of tumor localization by 37% and the accuracy of surgical resection range by 31%, indicating the clinical significance of three-dimensional reconstruction technology in improving surgical success rates and patient prognosis. Li Lianhai et al. also reported successful cases of increasing postoperative functional liver volume and remaining liver fraction through preoperative three-dimensional reconstruction.
In summary, three-dimensional reconstruction has significant clinical application value in liver resection, especially in the following situations: (1) tumors located in special areas that may invade major blood vessels and bile ducts; (2) severe liver cirrhosis with large tumor volume, where a large liver resection is expected; (3) potential vascular reconstruction during surgery. However, for marginal or small-volume liver tumors, the significance of three-dimensional reconstruction is limited. For patients with severe liver density unevenness or advanced cirrhosis, it is necessary to combine ICG retention rate, serological tests, Child-Pugh score, and ALBI score with other assessment methods.
2.3 Gd-EOB-DTPA Enhanced MRI
Gd-EOB-DTPA is a liver-specific MRI contrast agent. In patients with normal liver function, Gd-EOB-DTPA is excreted about 50% via the biliary tract and 50% via the kidneys. The first attempt to evaluate liver function using Gd-EOB-DTPA dynamic enhanced MRI was made by Yokoyama et al. in 1993, which was validated in animal models. Its high soft tissue resolution provides the possibility for measuring segmental liver volume, enabling the assessment of both local and overall liver function, thereby enhancing the safety of liver resection surgery. Yamada et al. proposed the formula for the safe range of liver resection with Gd-EOB-DTPA as “70×(SLF-962)/1 076(%)”. Some studies have shown that Gd-EOB-DTPA enhanced MRI can accurately predict PHLF after major liver resection. Barth et al. reported that Gd-EOB-DTPA enhanced MRI can also predict the growth of remaining liver after portal vein embolization. In patients with liver cirrhosis, hepatocyte uptake of Gd-EOB-DTPA is reduced, and biliary excretion decreases, leading to compensatory increases in renal function, thus prolonging the time the contrast agent remains in the bloodstream, increasing the signal intensity of the hepatic phase portal vein, indicating its role in assessing the degree of liver cirrhosis. Sourbron et al. proposed that Gd-EOB-DTPA enhanced MRI has higher accuracy than CT in differentiating benign from malignant lesions. The competition between bilirubin and Gd-EOB-DTPA during hepatocyte uptake and biliary excretion causes prolonged retention time of Gd-EOB-DTPA in the bloodstream in patients with hyperbilirubinemia, indicating certain limitations in the application of Gd-EOB-DTPA for these patients.
In conclusion, this method provides the dual service of simultaneous structural and functional assessment, and it is radiation-free, showing good clinical application value. However, issues such as long scanning time, high costs, and lack of standardized measurement methods still need to be addressed.

3Clinical Scoring Systems
3.1 Child-Pugh Scoring System and Its Modification
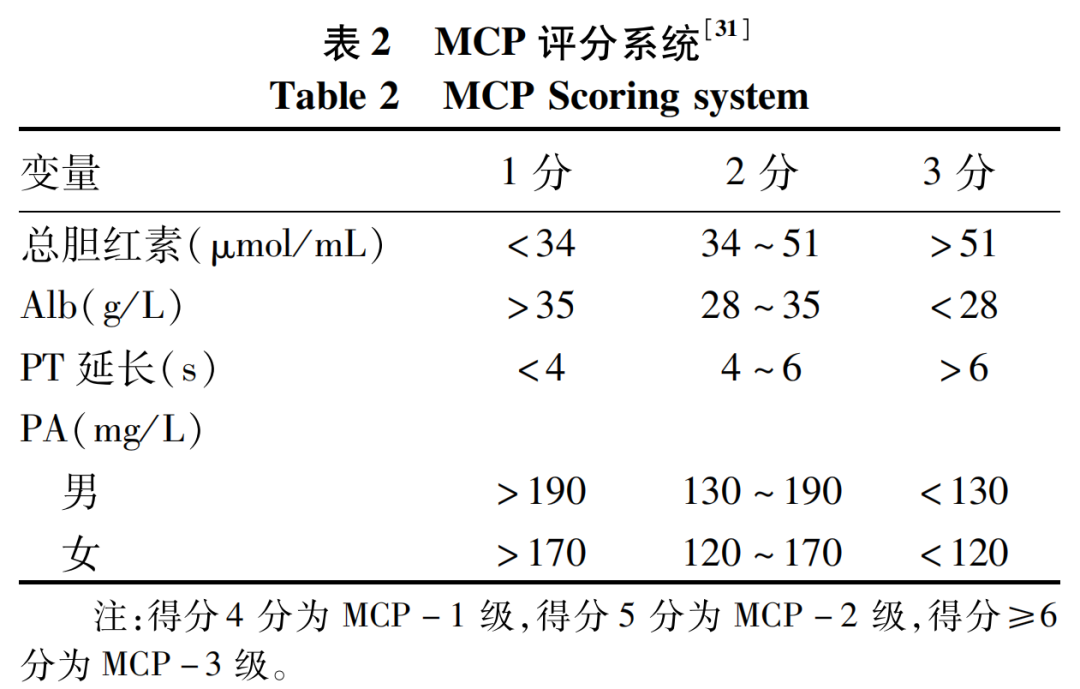
The Child-Pugh scoring system is the most commonly used clinical scoring system, proposed by Child and Turcotte in 1964 and modified by Pugh in 1974. It includes serum bilirubin, Alb levels, plasma PT, hepatic encephalopathy, and ascites, with the first three being quantitative serological indicators and the latter two determined by subjective judgment. Generally, for patients classified as grade A, liver cancer resection is relatively safe; for grade B patients, the choice of surgical method needs to consider other operative factors; for grade C patients, surgical treatment is not recommended or may require prior conservative treatment. In recent years, several studies have shown that even grade A patients can experience PHLF, while some grade B and C patients have shown good postoperative liver function recovery, indicating certain limitations of this scoring system: (1) poor grading effect for non-cirrhotic patients, with low reflection of actual liver function; (2) the presence of two subjective indicators in the scoring system can lead to assessment errors. Some researchers have proposed a modified Child-Pugh scoring system (MCP) that includes serum PA while removing hepatic encephalopathy and ascites, which can somewhat compensate for the original scoring system’s shortcomings.
3.2 Albumin-Bilirubin Score (ALBI)
Considering the certain defects of the Child-Pugh scoring system, Johnson et al. established a new liver function evaluation model called ALBI score in 2015 after analyzing survival data from 1,313 patients with hepatocellular carcinoma using statistical methods. The ALBI score = 0.66×lg[total bilirubin (μmol/L)] – 0.085×[Alb (g/L)], classifying liver function into three levels: ALBI score ≤ -2.60 is grade 1, -2.60 < ALBI score ≤ -1.39 is grade 2, and ALBI score > -1.39 is grade 3. The ALBI score has been widely used to predict postoperative prognosis in patients with viral hepatitis, liver cirrhosis, cholangitis, liver failure, and primary liver cancer. Tsilimigras et al. found that preoperative ALBI scores have high predictive value for 90-day mortality and overall survival in patients undergoing resection for intrahepatic cholangiocarcinoma (ICC). Zou et al. demonstrated that ALBI grading can predict the occurrence of PHLF, and the risk increases with higher ALBI grading. Ma et al. indicated that preoperative and postoperative ALBI scores can be used to predict overall survival in early-stage liver cancer patients. The ALBI score is more detailed than the Child-Pugh scoring system, avoids subjective indicators, and the indicators are easily obtainable. Its disadvantage is that the Alb and bilirubin indicators are somewhat affected by the patient’s nutritional status and biliary obstruction, and it cannot reflect the severity of multiple organ failure in end-stage liver disease patients. Therefore, some researchers have proposed that this scoring should be combined with indicators related to early renal function impairment. Increasing evidence suggests that the ALBI score has higher clinical predictive value than the Child-Pugh scoring system, and assessing liver function using the ALBI score preoperatively and postoperatively is significant for improving the clinical efficacy of liver resection.

4Dynamic Liver Function Measurement
4.1 ICG Clearance Test and Other Common Quantitative Tests
Dynamic liver function quantitative tests use some harmless exogenous substances to determine the liver’s clearance and metabolic capacity by intravenous injection, quantifying liver function reserve. Commonly used tests include ICG clearance test, lidocaine metabolism test, and breath tests. The ICG clearance rate test is a widely used dynamic liver function test; ICG is a fluorescent dye selectively taken up by the liver and excreted via bile. After intravenous injection of 0.5 mg/kg, a healthy liver excretes 97% of the dye within about 20 minutes. The ICG clearance rate can be determined during the perioperative period or intraoperatively using optical transcutaneous sensors for serum sampling or pulse dye densitometry. Common indicators of ICG clearance include the percentage of ICG retained after 15 minutes (ICG-R15) or the ICG plasma disappearance rate (ICG-PDR). ICG-R15 ≤ 15% and ICG-PDR ≥ 18%/min are usually seen in healthy livers. The higher the ICG-R15 value or the lower the ICG-PDR value, the higher the risk of PHLF, which is related to the extent of liver resection. It is generally believed that normal liver function has ICG-R15 ≤ 10%, which can tolerate the resection of two or more liver segments. As ICG-R15 increases, the feasibility of liver resection and the volume of liver to be removed must be carefully considered. The accuracy of ICG in predicting PHLF, liver function decompensation (i.e., postoperative ascites, impaired quality of life and survival rate), and mortality has been confirmed in patients with cirrhosis, hepatocellular carcinoma, and perihilar cholangiocarcinoma. However, the accuracy of ICG in predicting PHLF in non-cirrhotic patients is relatively low, so this test should be more widely applied to patients with cirrhosis. Moreover, the ICG clearance rate of the remaining liver volume is a better predictor of the occurrence of PHLF after preoperative portal vein embolization (PVE) than liver volume itself. The advantages of this test include minimal irritation to the body, few adverse reactions and allergic phenomena, and ease of operation. However, the ICG clearance test is also affected by liver blood flow, intrahepatic shunt conditions, serum bilirubin levels, biliary obstruction conditions, etc., which can reduce the reliability of the ICG clearance test. Furthermore, the ICG clearance test reflects overall liver function; considering the uneven function of various regions of the liver, the evaluation of liver function by ICG-R15 also varies. The Albumin-Indocyanine Green Assessment System (ALICE) is a grading system for patients with cirrhosis and hepatocellular carcinoma that combines serum Alb levels and ICG-R15 values, with the formula: 0.663×log10(ICG-R15[%])-0.0718×Alb(g/L). Some studies have confirmed that ALICE can predict PHLF and mortality in patients undergoing liver resection for hepatocellular carcinoma, which has also been validated in patients with cholangiocarcinoma.
4.2 Radionuclide Liver Function Tests
4.2.1 99Technetiumm-Labeled Galactosyl Human Serum Albumin (99Tcm-GSA) Imaging
GSA is a sialic acid-free glycoprotein analogue that can bind to specific receptors in liver cells, remaining in the liver for about 30 minutes. After intravenous injection, the gamma camera is used to calculate the uptake and blood clearance rates of this substance in the liver through planar dynamic radionuclide imaging, thus evaluating liver reserve function. Some researchers have combined 99Tcm-GSA imaging with SPECT/CT to assess the reserve function of the remaining liver volume, which can effectively predict the occurrence of PHLF and postoperative evaluation of ALPPS. Tokorodani et al. calculated the average uptake rate (SUVmean) of the liver using this method and proposed that SUVmean > 6.7 can accurately predict severe liver fibrosis. Additionally, some studies have found that GSA can be used for liver function assessment and PHLF prediction in patients with concomitant biliary lesions or cholestasis, as GSA is only absorbed by liver cells and is not affected by serum bilirubin levels; unfortunately, the difficulty in obtaining GSA limits the development of this technology.
4.2.2 99Tcm-Bromosulfophthalein Liver-Biliary Imaging (HBS)
Ida’s absorption, excretion, and non-hepatic conversion characteristics are similar to those of ICG. Bromosulfophthalein is the most liver-specific derivative of IDA and can be absorbed by liver-specific proteins, showing a high liver uptake rate and minimal renal excretion. This makes it an ideal liver function assessment method. After intravenous injection of 99Tcm-Bromosulfophthalein, the relative uptake ratio of the liver is calculated through dynamic scintigraphy and corrected for body surface area, allowing precise assessment of liver function in various segments when combined with SPECT/CT. HBS has the advantage of enabling both overall and local liver function assessment, and it can be combined with SPECT/CT for volume evaluation, taking into account the unevenness of liver function. However, Gupta et al. suggested that the effects of hyperbilirubinemia and low Albemia on HBS accuracy still require more clinical research to explore.

5Artificial Intelligence Assessment
In recent years, artificial intelligence has rapidly developed in the field of medical imaging, aligning with the concept of precision surgery. Intelligent radiomics, machine learning, and deep learning are currently hot research topics.
5.1 Intelligent Radiomics
In 2012, Dutch scholar Lambin first proposed the concept of radiomics, which involves collecting relevant imaging features from a large number of imaging studies, using automated feature extraction algorithms to compare them with clinical and genetic data, and mining highly representative radiomic features to quantitatively assess the pathological grading, typing, differentiation degree, and prognosis prediction of liver cancer. The assessment process mainly includes image acquisition, image segmentation, feature extraction, data analysis, and model construction. Traditional imaging diagnosis relies on the clinical experience and discrimination ability of radiologists, while intelligent radiomics can improve the efficiency of clinical practitioners, and its diagnostic accuracy can even exceed that of radiologists. Chen et al. constructed a prediction model for the differentiation degree of hepatocellular carcinoma based on radiomics, which has high predictive value. Yang et al. accurately assessed the risk of microvascular invasion in patients with hepatocellular carcinoma using radiomics, as artificial intelligence can identify various information in images that are not visible to the human eye, providing higher precision in predicting patient prognosis. However, there are currently no unified standards for image acquisition, data processing, and sharing, which limits the development of this technology, and more multicenter experiments are needed to explore it further in the future.
5.2 Machine Learning and Deep Learning
Machine learning based on artificial intelligence endows computers with human-like thinking capabilities, using their vast data processing power to uncover intrinsic links between diseases and clinical data, thereby helping clinicians improve their work efficiency. Deep learning is one of the hottest branches of machine learning, with convolutional neural networks being one of the most important algorithms in deep learning. In recent years, numerous researchers have successfully used 3D convolutional neural network methods for precise segmentation of the liver and liver tumors, significantly guiding the diagnosis and treatment of liver cancer. Furthermore, deep learning has been widely used in studies involving liver fibrosis staging, optimizing imaging diagnostics, tumor grading, and early diagnosis of liver cancer. In the future, with the development of artificial intelligence, we look forward to the emergence of an artificial intelligence-driven “one-stop” liver cancer diagnosis and treatment system.

6Summary and Outlook
How to accurately and comprehensively assess the overall and local reserve functions of the liver is of utmost importance in the preoperative preparation for liver surgery. Under the influence of precision medicine, meticulous assessment of the liver concerns the success of surgery and survival benefits for patients, while reducing the incidence of PHLF is a direct goal of liver surgical treatment. Various liver function evaluation methods have their advantages and disadvantages, and combining multiple examination methods to complement each other is currently the most effective strategy for liver function assessment. Currently, the commonly used Child-Pugh score is employed to select surgical patients, combined with dynamic liver function measurements, imaging analyses, and routine biochemical tests to make surgical decisions. With the introduction of emerging artificial intelligence, the liver function evaluation system will develop towards greater precision, intelligence, and personalization.

http://www.lcgdbzz.org/cn/article/doi/10.3969/j.issn.1001-5256.2023.05.034

Pei Junpeng, Ding Youming. Assessment Methods for Liver Reserve Function Before Hepatectomy[J]. Clinical Journal of Hepatology and Biliary Diseases, 2023, 39(5): 1219-1226
