3D printing technology, also known as additive manufacturing, is a type of rapid prototyping technology that constructs physical objects based on digital model files using various adhesive materials through a layer-by-layer printing method. 3D printing technology includes laser or electron beam sintering and melting technology, thermoplastic extrusion deposition manufacturing technology, and photopolymerization molding technology, among others. In the 1980s, 3D printing technology began to be applied to the printing of physical models based on CT scan data. In recent years, 3D printing technology has gradually been applied in clinical settings, from 3D printed models to 3D printed guides and prosthetics, all demonstrating good therapeutic results, facilitating personalized and precise diagnosis and treatment of orthopedic diseases. This article provides a brief introduction to the common applications of 3D printing technology in orthopedics.
Introduction
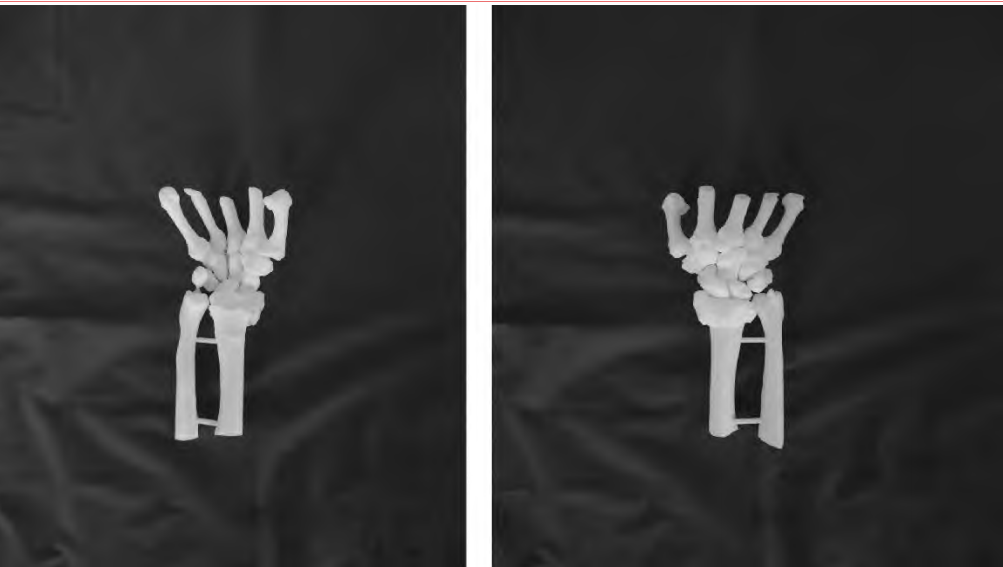
The above image shows a 3D printed model of a distal radius fracture. (From clinical practice)
Application of 3D Printed Models in Orthopedics
The production of 3D printed models generally requires the collection of thin-slice CT data of the area to be printed from the patient, which is imported into the computer software Mimics in DICOM format for processing. The software is used to design the 3D printed model, and a 1:1 scale physical model is printed using a 3D printer. Currently, 3D printed models are mainly used for anatomical teaching, preoperative communication, and preoperative surgical planning. For certain fractures with complex surrounding anatomical structures, 3D printed models allow for repeated preoperative surgical planning, ensuring precise operations during surgery, reducing the risk of nerve and vascular damage, and aiding in faster postoperative recovery for patients. The personalized customization of 3D printed models enables patients and their families to better understand the condition in a clear and comprehensible manner, facilitating preoperative communication and helping to avoid potential doctor-patient conflicts.
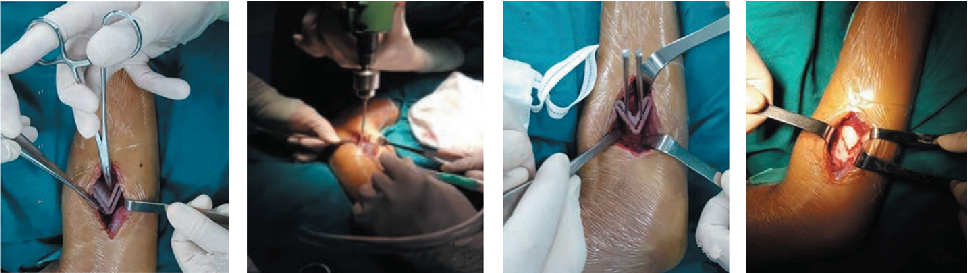
The above image shows a patient with rotational deformity of the upper radius undergoing minimally invasive conical osteotomy treatment using a personalized 3D printed navigation module. (From reference 2)
Application of 3D Printed Osteotomy Guides in Orthopedics
The preparation of 3D printed personalized osteotomy guides begins with obtaining thin-slice CT scan images of the patient, which are imported into Mimics software for three-dimensional reconstruction. Using mirroring technology, the image of the healthy side is overlaid with that of the deformed side to clarify the location and degree of the deformity. Subsequently, a virtual cutting plane is set in the area of deformity healing, and the cut bone segment is rotated and moved to match the healthy side, designing a personalized 3D printed osteotomy guide, which is then printed using a 3D printer. Currently, 3D printed osteotomy guides are mainly used for the treatment of fracture malunion, osteotomy for joint preservation in arthritis, and osteotomy during joint replacement surgery. Each patient has individual differences, and the severity of the condition varies, making empirical osteotomy a significant challenge for surgeons. The clinical application of 3D printed osteotomy guides simplifies many complex osteotomy surgeries, greatly saving surgical time, allowing even less experienced surgeons to perform them easily, and achieving good functional recovery post-surgery due to precise osteotomy accuracy.
The above image shows the application of a 3D printed navigation guide in a calcaneal fracture surgery. (From clinical practice)
Application of 3D Printed Navigation Guides in Orthopedics
The preparation of 3D printed navigation guides begins with obtaining imaging data of the fracture site, typically using thin-slice CT scan images, which are imported into specialized 3D printed navigation guide design software, such as Mimics. The software is used to reconstruct the model of the fracture site, simulate reduction, plan the placement and trajectory of internal fixation devices, measure the length of the internal fixation devices, and design a 3D printed navigation guide that fits the body surface. Through cylindrical navigation holes, internal fixation devices such as Kirschner wires or screws can be inserted accurately and efficiently. The STL format file is generated and input into the 3D printer, which uses materials such as photosensitive resin to print a 1:1 scale 3D printed physical navigation guide. Currently, 3D printed navigation guides are widely used for the placement of internal fixation devices in spinal fractures, pelvic fractures, femoral neck fractures, and calcaneal fractures. The use of 3D printed navigation guides for treating various fractures provides clinical physicians with a new option, allowing for more accurate placement of internal fixation devices, shorter surgical times, and faster postoperative recovery, effectively reducing the incidence of related complications and achieving satisfactory treatment outcomes.Application of 3D Printed Prosthetics in OrthopedicsThe production of 3D printed prosthetics involves importing CT data into Mimics software to construct a three-dimensional model. Subsequently, image fusion technology is used to mirror the healthy side image to the affected side, designing the preliminary shape of the prosthetic based on the range and morphology of the osteotomy or bone defect. Various metal materials are then used to print the prosthetic on a 3D printer. Currently, 3D printed prosthetics are mainly used for various types of bone defects, such as traumatic bone defects, bone defects after tumor resection, and infectious bone defects, as well as prosthetics for various joint replacements. The construction of ultra-porous fixation interfaces on 3D printed prosthetics facilitates bone ingrowth. The personalized design of prosthetics provides a better match, offering a good treatment solution for complex bone defect issues, and is well-received by clinical physicians.
Currently, the clinical promotion and application of 3D printing technology also face certain issues, such as the high cost of 3D printing equipment; the need for further development of 3D printing materials; the time required for physical printing, which cannot meet the needs of emergency patients; and the significant increase in patient costs associated with clinical applications. The application of 3D printing technology in orthopedics is still under continuous exploration and development, with enormous application prospects that are worth looking forward to.
References
[1] Zhang Cheng, Li Chao, An Chao, et al. Application of 3D Printing Technology in Orthopedic Rehabilitation Treatment [J]. Medical Equipment, 2022, 43(2):93-97,108
[2] Zhang Cheng, Chen Shutao, Gao Wuchang. Research on the Application of 3D Printed Osteotomy Guides in Osteotomy Orthopedics [J]. Medical Equipment, 2020, 41(3):98-101
-END-
Disclaimer: This article is original by Zhang Cheng and is intended for learning and communication purposes only. Unauthorized reproduction is prohibited!
 Good Medical Skills welcomes your submissions
Good Medical Skills welcomes your submissions
If you would like to share your clinical diagnosis and treatment experiences with more colleagues, allowing more people to see you and benefit, we welcome your submissions!
Submission requirements: Original academic content of over 1500 words
Submission method: haoyishu-zy03 (WeChat)
Medicine knows no bounds; every effort we make will be remembered by the world in another way. We look forward to your excellence!
Recommended Reading
Morning Read | A New Plaster Technique for Treating Tongue-Type Calcaneal Fractures with Soft Tissue InjuryMorning Read | [Popular Science] What You Don’t Know About Low Back Pain – Lumbar Facet Joint InstabilityMorning Read | How to Handle Misdiagnosed Calcific Tendonitis of the Shoulder
Click the card below to quickly follow us
👇 Click below [Read the original text] to download the Good Medical Skills APP and start your learning journey!