
Editor’s Note
When a school-aged male child experiences a decline in vision in both eyes, and after excluding refractive diseases, visual function issues, glaucoma, and other conditions, if the fundus shows no abnormalities, yet OCT indicates a lattice-like change in the temporal side of the macular nerve epithelium, and VEP shows a slight decrease in the P100 amplitude in both eyes, what disease could you suspect? After 5 years of follow-up, if the patient shows significant thinning of the ganglion cell complex (GCC) thickness, and VEP indicates a delay in the P100 wave peak, what diagnosis might come to mind? This issue’s case investigation is brought to you by Professor Chen Juan from Changsha Aier Eye Hospital, featuring a case of unusual pediatric macular degeneration.
Highlights of This Issue
· The patient is a 9-year-old boy who was admitted due to “noticing poor vision in both eyes for 5 days.” Corrected vision was 0.8 in the right eye and 0.6 in the left eye. No abnormalities were found during specialized examinations, glaucoma screening, or fundus photography. OCT showed a lattice-like change in the temporal side of the macular nerve epithelium, and VEP indicated a slight decrease in P100 amplitude in both eyes. After differential diagnosis, he was diagnosed with “congenital retinoschisis,” and since there was no risk of retinal detachment, he was placed under observation.
· However, during the 5-year follow-up, the patient’s vision declined, and OCT showed a significant thinning of the ganglion cell complex (GCC); VEP indicated that the left eye’s 1-degree grid P100 wave amplitude showed no significant abnormalities, with a delay in peak time; computerized visual fields indicated a paracentral scotoma in the left eye. This raised the alert of Professor Chen Juan’s team, prompting genetic testing on the patient, which confirmed the true cause of the disease and appropriate treatment was provided.
Patient Information
The patient is a 9-year-old boy. (Initial diagnosis on 2015-09-18)
Main Complaint: Noticed poor vision in both eyes for 5 days.
Present Illness: Noticed a decline in vision in both eyes 5 days ago. Distant vision is unclear, and he cannot see the blackboard clearly during class, but near vision is clear. No eye swelling or pain, no photophobia or tearing. No headaches or tinnitus.
Past Medical History: No history of eye diseases or family history of eye diseases. At age 6, he suffered from “encephalitis” and was treated in a children’s hospital, with no change in vision at that time. His vision was “normal” during the school entrance health check. No history of trauma or surgery.
Personal History: Full-term delivery, had “jaundice” after birth, which subsided after a few days. Growth and development are normal, and vaccinations are done as scheduled.
Specialized Examination:
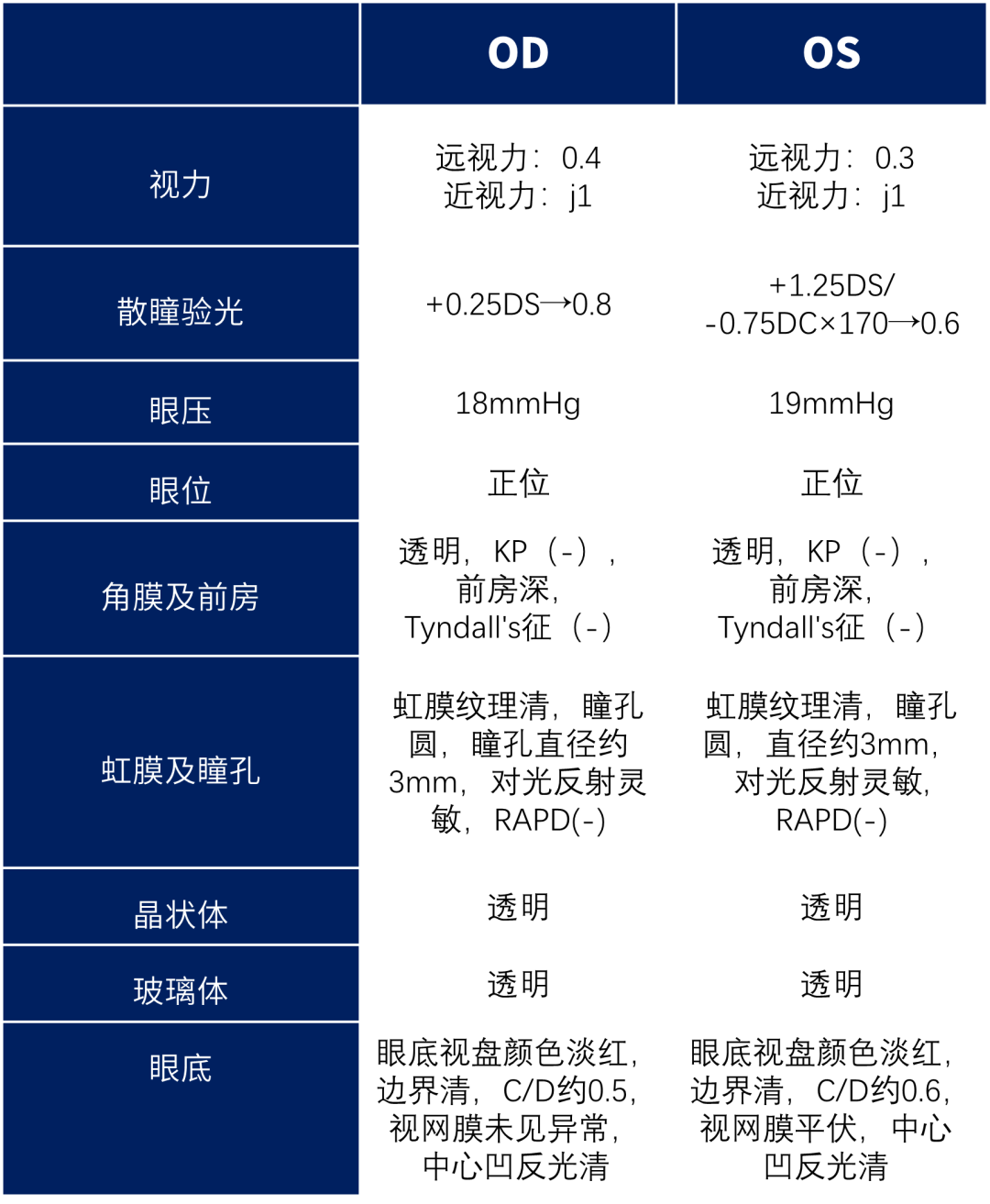
Ocular Auxiliary Examination:
Anterior segment photography:

Figure 1 Fundus photography of both eyes (2015-09-19)
Preliminary Diagnosis
Differential Diagnosis
• Refractive error: The child’s refraction indicated some degree of hyperopia and astigmatism, but considering the possible hyperopic reserve in a 9-year-old child, the refraction results are not deemed abnormal.
• Amblyopia: The child’s best corrected vision was 0.8 in the right eye and 0.6 in the left eye. Amblyopia is defined as a situation where the best corrected vision in one or both eyes is lower than that of age-matched normal children, with no organic lesions found in the eye examination; further examination is needed to rule out organic lesions.
• Pediatric glaucoma: The child’s intraocular pressure was normal, but the cup-to-disc ratio was slightly larger, requiring further glaucoma-related examinations.
• Macular degeneration: Preliminary outpatient examination did not reveal any obvious abnormalities, requiring further fundus examination.
Further Examination
(1) Glaucoma screening: Corneal thickness (CCT): Right eye: 481 um, Left eye: 484 um; 24-hour intraocular pressure normal; RNFL and visual fields showed no abnormalities.
(2) Electrophysiological examination: Retinal electroretinogram (ERG): F-ERG basically normal, mfERG left eye lower than right eye peak; Visual evoked potential (VEP): P100 time normal in both eyes, amplitude slightly decreased.
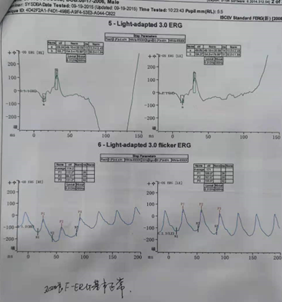
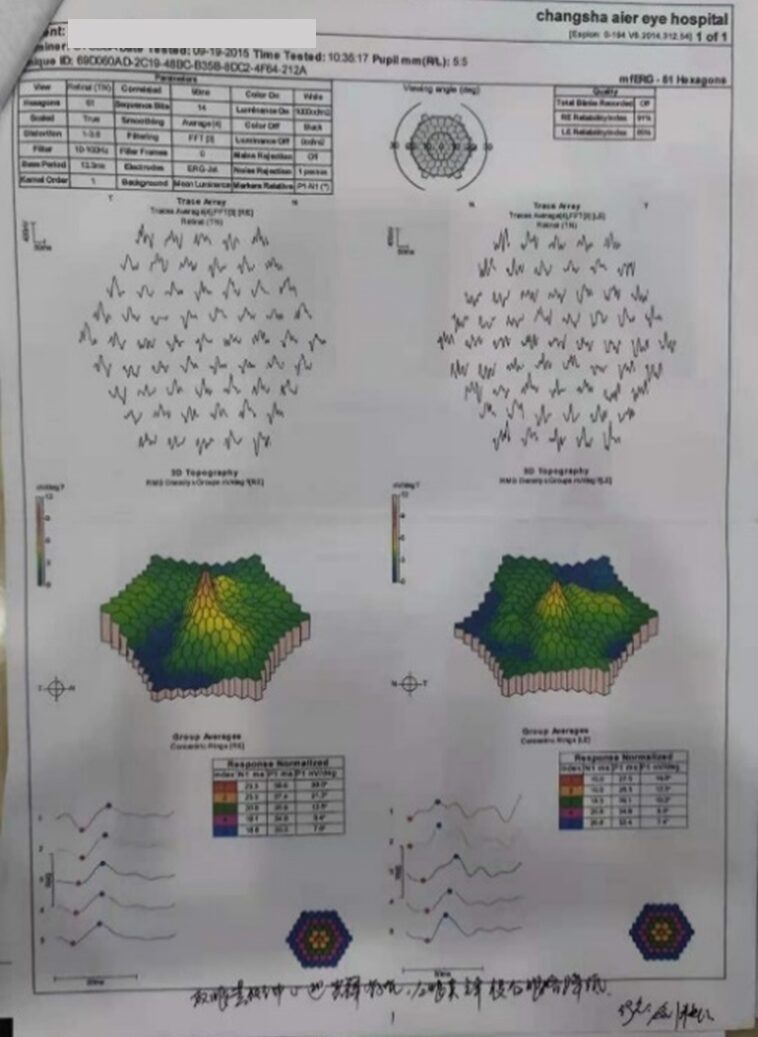
Figure 2 Bilateral retinal electroretinogram (2015-09-19)
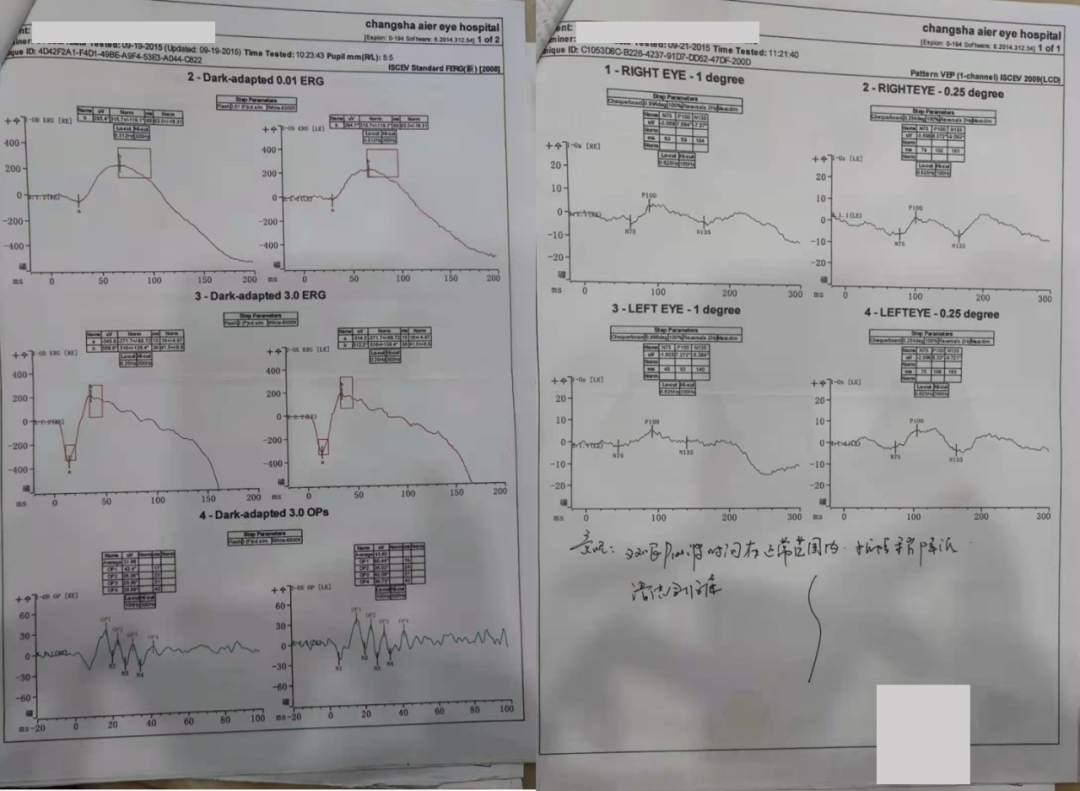
Figure 3 Bilateral visual evoked potential (2015-09-19)
(3) OCT examination: Bilateral macular fovea visible, nerve epithelium shows a lattice-like change.
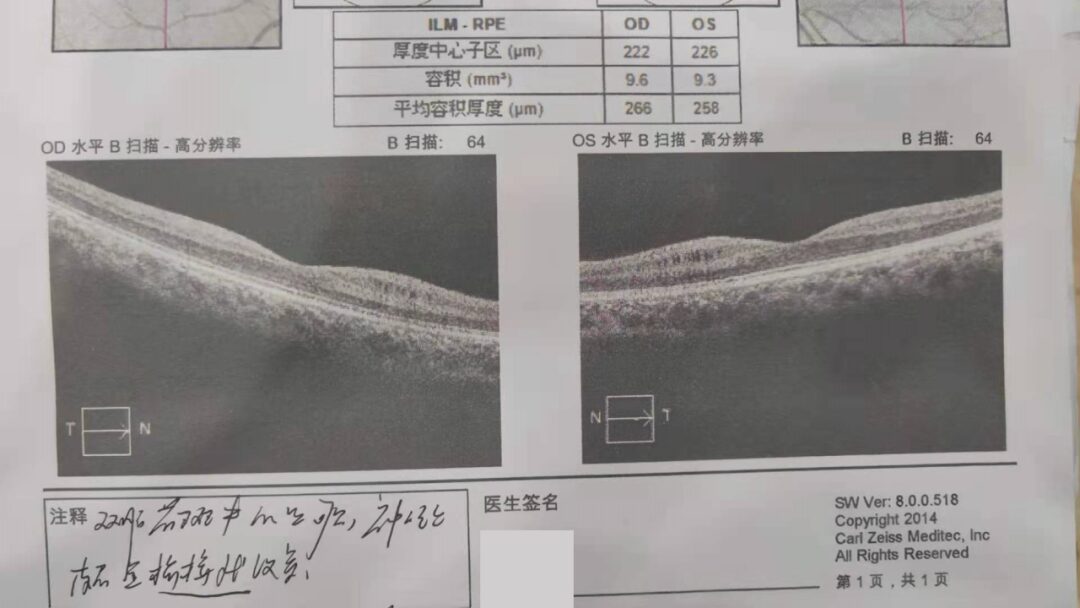
Figure 4 Bilateral posterior segment OCT (2015-09-19)
Considered to be pediatric macular degeneration.
Further Differential Diagnosis
• Macular edema: Often secondary to vascular, inflammatory, retinal degenerative diseases, or post-intraocular surgery. It is recommended to perform fundus fluorescein angiography, but the child was uncooperative, and the parents refused.
• Macular telangiectasia (MacTel): Type 1 is more common in young males and typically occurs in one eye. Retinal vein or artery-like dilation is a special manifestation of Coats’ disease. Type 2 is the most common and usually occurs in middle-aged patients. Capillary changes in the macular area, formation of a cavity at the fovea, loss of outer retinal structure. This does not match the presentation of this patient. [1]
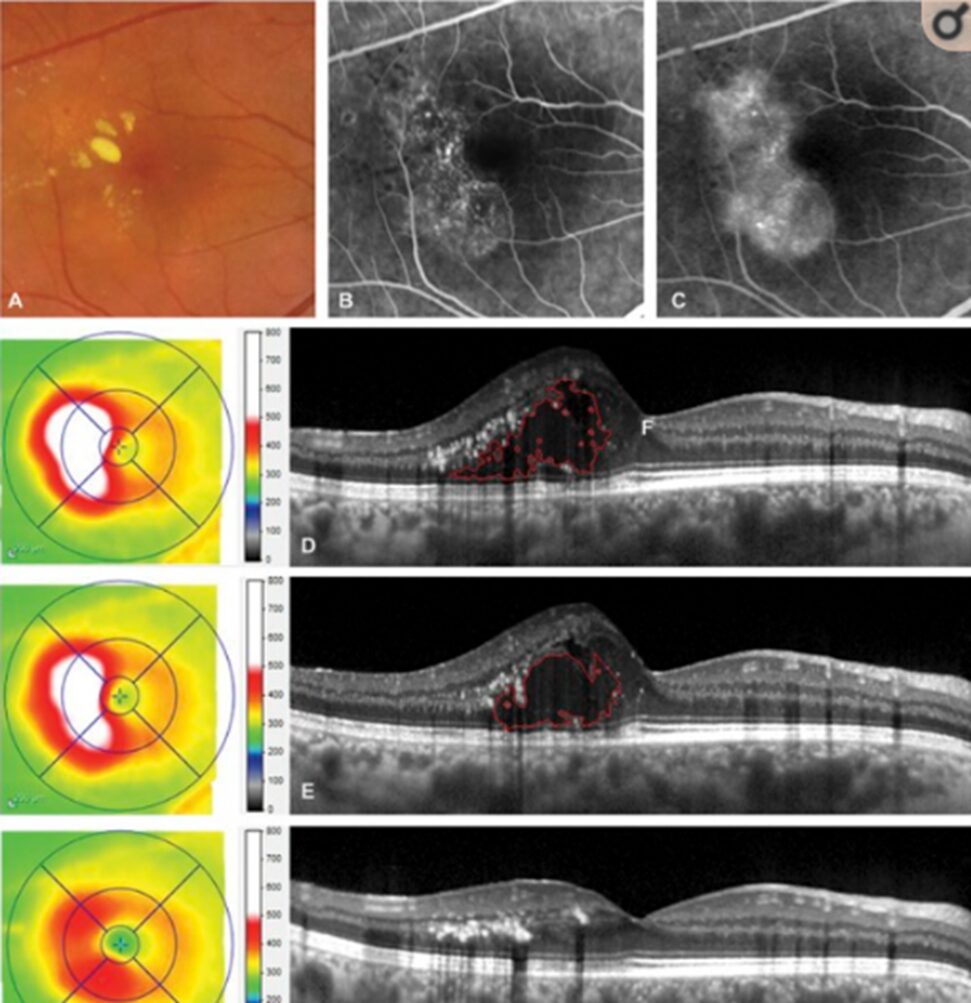

Figure 5 MacTel fundus photography and typical OCT changes
(Not this patient)
• Congenital retinoschisis (XLRS): X-linked recessive inheritance, incidence 0.004-0.02%, affecting male children, bilateral involvement. The macular area shows radiating changes, with 50% of patients having peripheral retinal schisis, typically in the temporal lower quadrant, with a lace-like change. Vitreous hemorrhage and retinal detachment can occur. OCT shows cystic changes between retinal layers and vertical bridge-like connections (lattice-like changes). ERG b-wave amplitude is significantly decreased. [2]Matches the presentation of this patient.
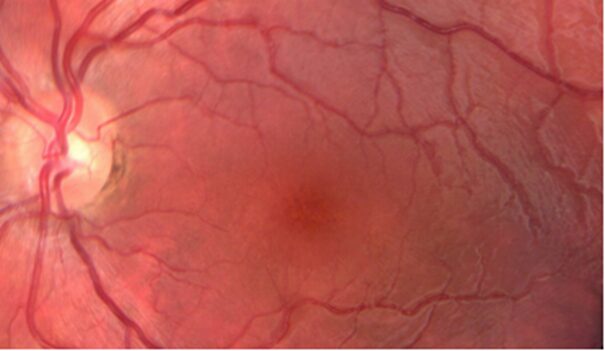
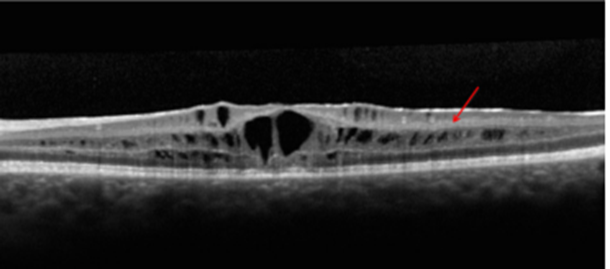
Figure 6 XLRS fundus photography and typical OCT changes (Not this patient)
Treatment
Treatment options for congenital retinoschisis:
(1) Follow-up: For patients with better vision and no risk of retinal detachment, follow-up is recommended. This patient was placed under follow-up observation.
(2) Preventive treatment: For retinal schisis with a risk of retinal detachment, preventive treatment is recommended.
(3) Surgery: If the macula is threatened and vision is affected, or if there is a full-thickness hole, recurrent vitreous hemorrhage, or retinal detachment, vitreous surgery is indicated.
Follow-up and Questions
Follow-up on 2016-04-22:
Vision: OD: 0.5 (unaided), -0.75DS→0.8 (corrected); OS: 0.5 (unaided), +0.25DS/-1.00DC×175→0.6.
Fundus photography: No abnormalities found.
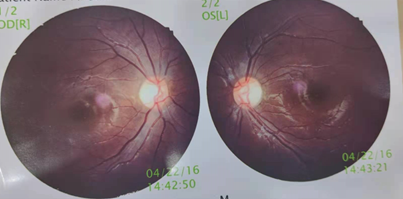
Figure 7 Fundus photography of both eyes (2016-04-22)
OCT not checked, continued observation.
Follow-up on 2017-10-18:
Vision: OD: 0.4 (unaided), OS: 0.5 (unaided).
Fundus photography: No significant changes compared to before.
Posterior segment OCT: No significant changes compared to before.
Continued observation was recommended.
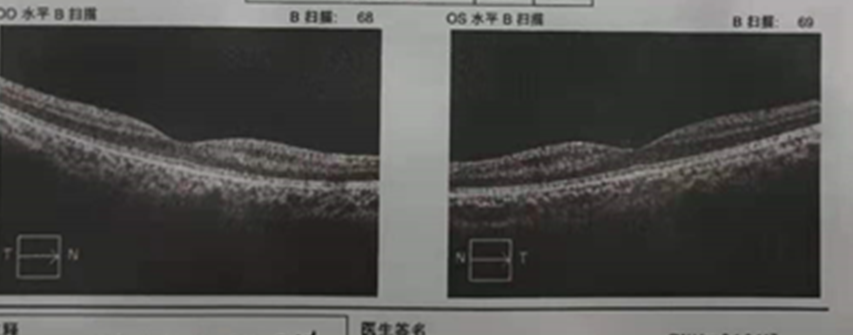
Figure 8 Bilateral posterior segment OCT (2017-10-18)
Follow-up on 2020-10-03:
Vision: OD: 0.25 (unaided), -2.75DS/-0.75DC×180→0.7 (corrected); OS: 0.4 (unaided), -0.25DS/-0.75DC×165→0.5+ (corrected).
During this visit, the child was older and willing to cooperate with FFA examination. Due to a slight decline in vision, VEP and other tests were repeated.
Fundus photography: No significant changes compared to before.
OCT&OCTA: Retinal schisis only limited to the area between the optic disc and the fovea, not involving the fovea and the temporal side of the fovea, limited to the inner nuclear layer. Ganglion cell complex (GCC) thickness significantly decreased.
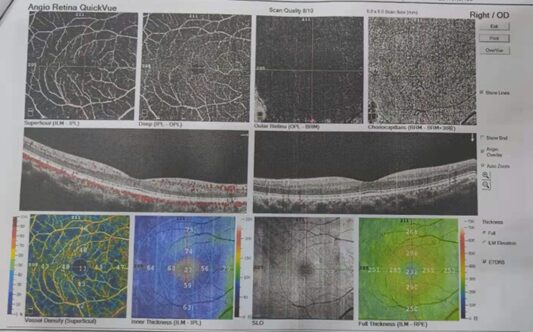

Figure 9 Bilateral posterior segment OCT (2020-10-03)
VEP: Left eye 1-degree grid P100 wave amplitude showed no significant abnormalities, peak time delayed.
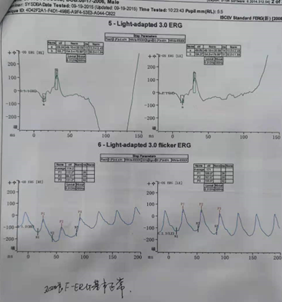
Figure 10 Bilateral VEP (2020-10-03)
Computerized visual fields: A paracentral scotoma is visible in the left eye.
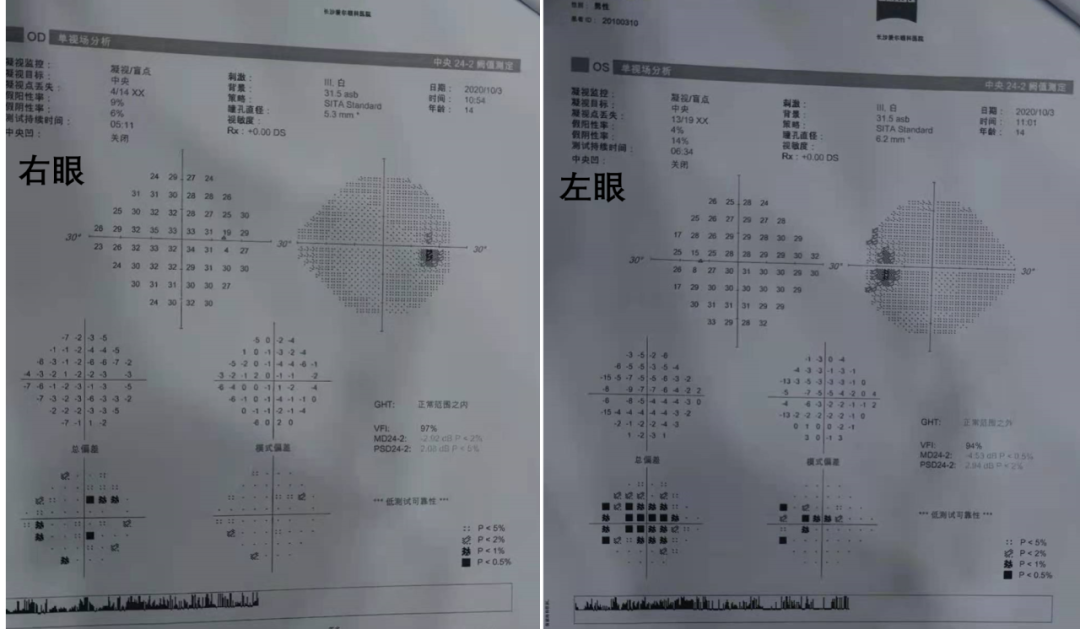
Figure 11 Bilateral computerized visual fields (2020-10-03)
FFA: The left eye showed slightly low fluorescence at the optic disc, no leakage.
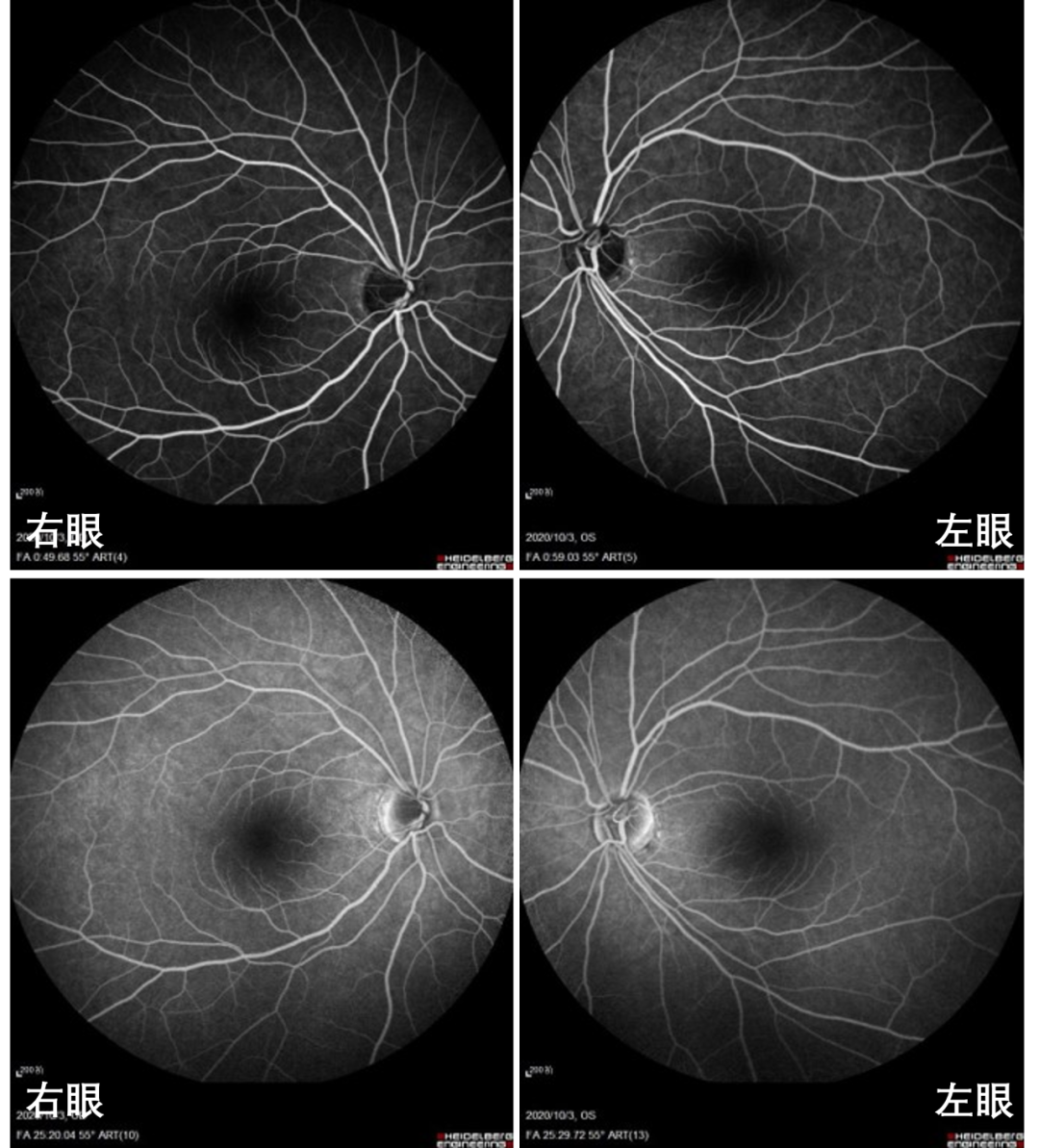
Figure 12 Bilateral FFA (2020-10-03)
Based on these examination results, what considerations do you have? What should the next steps be?
Clarifications
Genetic testing on the patient’s peripheral blood: m.12811T→C mutation
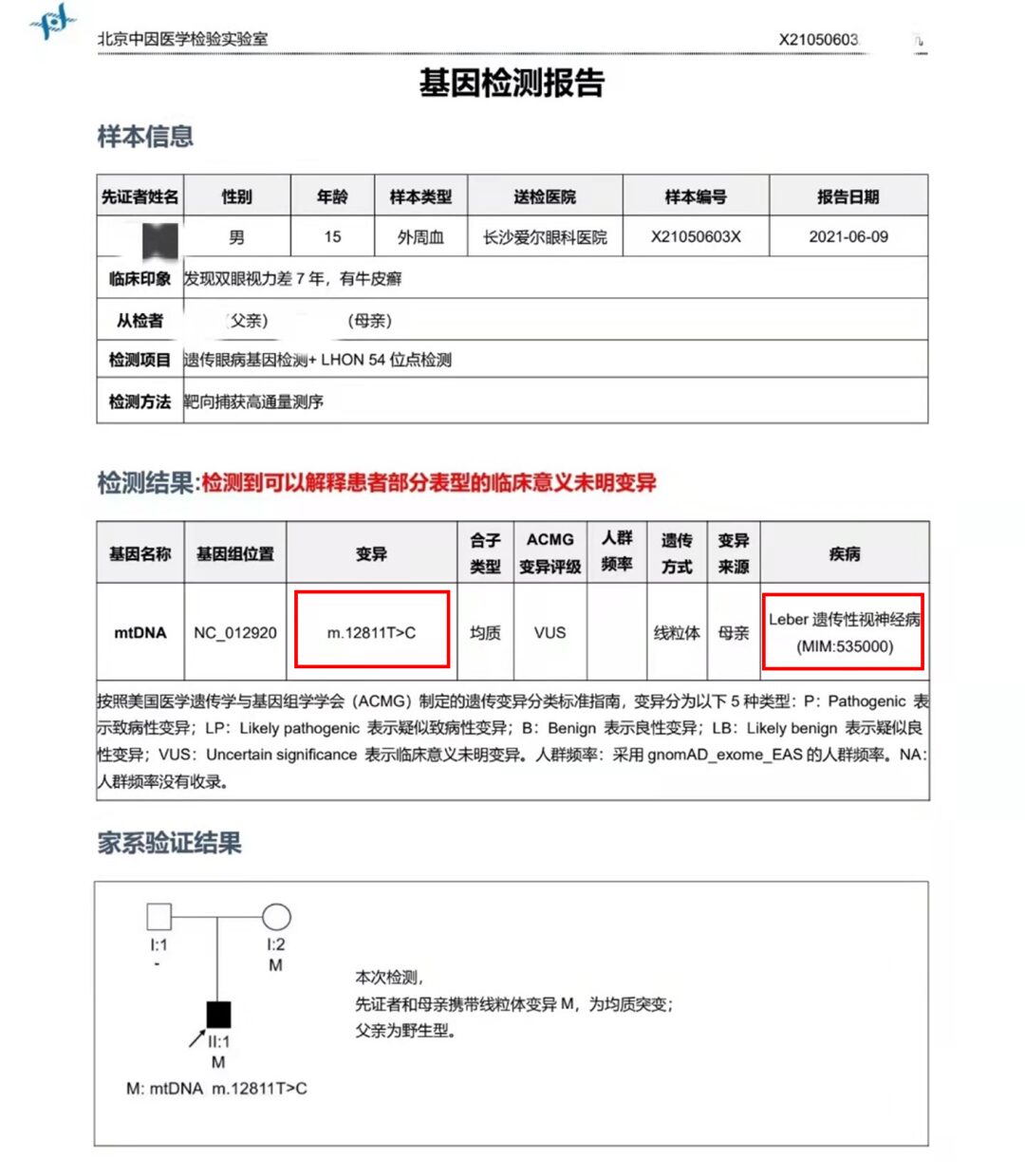
Figure 13 Patient’s genetic test report
Diagnosis
Leber Hereditary Optic Neuropathy (LHON)
Leber Hereditary Optic Neuropathy (LHON) is a maternally inherited mitochondrial disease that leads to acute or subacute painless vision loss. [3] More than 90% of patients’ lesions are caused by mitochondrial DNA mutations at m.11778G>A, m.3460G>A and m.14484T>C loci. [4] Damage or apoptosis of retinal ganglion cells (RGCs) is the main pathophysiological mechanism of LHON. DNA mutations lead to decreased activity of mitochondrial respiratory chain complex I, resulting in mitochondrial dysfunction and energy supply impairment, leading to functional loss or apoptosis of retinal ganglion cells. [3] The 12811 mutation represents a mild phenotype, and little is known about it; any hypotheses regarding its clinical course are controversial. [5]
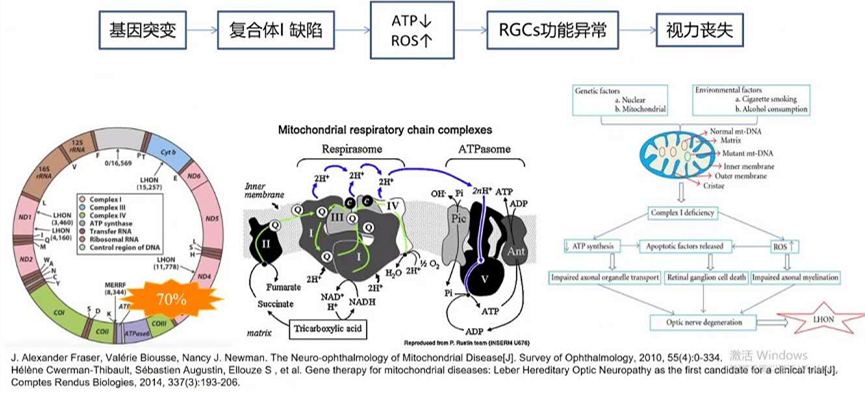
Figure 14 Pathophysiological mechanism of LHON
Clinical Stages of LHON:
• Preclinical stage: Asymptomatic, microvascular changes around the optic disc.
• Acute stage: Painless acute or subacute central vision decline, optic disc congestion, disc surrounding vein dilation, early FFA shows capillary dilation around the optic disc, with no leakage.
• Chronic atrophy stage: Occurs 6 months after onset, optic disc pallor, reduced blood vessels around the disc, FFA shows reduced, narrowed, and delayed filling of arteries.
LHON Diagnostic Criteria:
• Simultaneous or sequential occurrence of painless acute or subacute vision loss in both eyes.
• In the acute phase, optic disc congestion, surrounding capillary dilation, and nerve fiber layer swelling; late optic nerve atrophy, particularly temporal side.
• Visual field defects manifest as central or paracentral scotomas.
• VEP amplitude and peak time abnormalities.
• Family history of maternal members with disease or carrier status, mtDNA testing confirms the presence of mutations.
• Exclusion of intracranial tumors and other central nervous system diseases via CT or MRI. [6]
*Microcystic macular edema (MME) was discovered and named by Gelfand during OCT examinations of patients with multiple sclerosis; it is not an independent eye disease but a specific imaging term occurring in the retinal inner nuclear layer. MME can be seen in various eye diseases (multiple sclerosis, optic nerve glioma, age-related macular degeneration, tobacco-alcohol optic neuropathy, etc.), characterized by small cystic, discrete, well-defined low reflectance areas in the retinal inner nuclear layer; the exact mechanism is unclear but may relate to Müller cells. [7] Some scholars have reported observing MME in LHON patients [8], which was also noted in this patient.
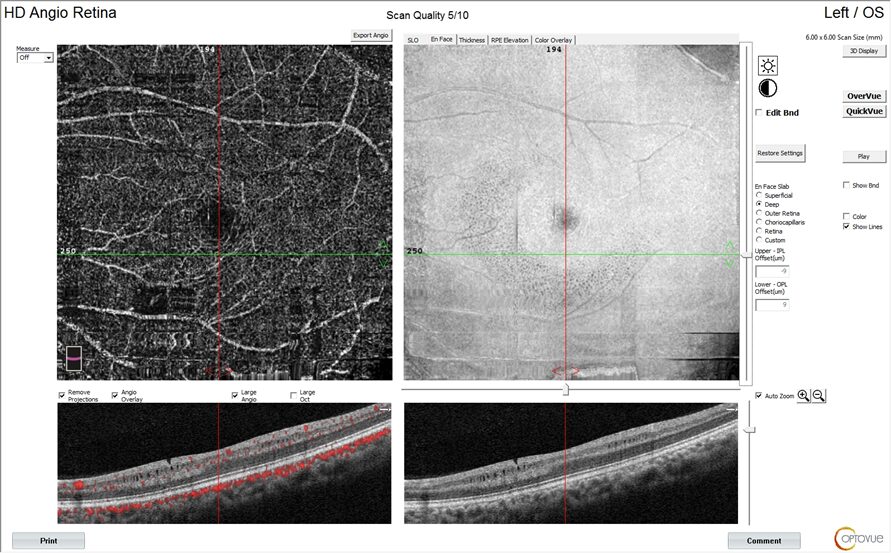
Figure 15 Microcystic macular edema in this patient
Treatment
• Idebenone, a short-chain coenzyme Q10 analogue, has antioxidant effects, overcoming the respiratory chain interruption caused by mitochondrial point mutations leading to complex I dysfunction, directly delivering to complex III, restoring ATP generation, and clearing oxygen free radicals. This patient was prescribed Idebenone treatment at an external hospital and will be followed up at our hospital in the future.
• Gene therapy, mitochondrial replacement therapy, etc., are not yet widely applied.
Summary
In 1871, Theodor Leber described a unique pattern of painless subacute vision loss among young individuals in four families and recognized the maternal inheritance and male predominance of this presentation [9]. Leber Hereditary Optic Neuropathy (LHON) is a hereditary mitochondrial optic neuropathy, with mitochondrial DNA mutations being more than 90% m.3460G>A (MTND1), m.11778G>A (MTND4), and m.14484T>C (MTND6), with m.12811T>C mutation representing a mild phenotype; hypotheses regarding its clinical course remain controversial. LHON is characterized primarily by acute or subacute onset, painless vision loss, and central visual field defects; in the subacute phase, optic discs may appear congested, accompanied by swelling of the retinal nerve fiber layer (RNFL) around the disc and increased dilation and tortuosity of surrounding capillaries. During this stage, OCT imaging of the macula has shown significant thinning of the ganglion cell complex. As the disease progresses to the chronic stage, in addition to the pallor of the retinal edges and obvious RNFL thinning, the “cupping” phenomenon of the optic disc can sometimes be observed. In addition to vision loss, a minority of LHON patients may present with other neurological features as part of a more severe “LHON +” phenotype, including ataxia, juvenile encephalopathy, spasticity, and peripheral neuropathy [9]. For patients with corresponding clinical manifestations, vigilance should be heightened, and mtDNA testing can confirm the presence of mutations. Idebenone is currently the only drug proven effective through clinical studies; gene therapy and mitochondrial replacement therapy are also being explored.
References
|
1 |
Kowalczuk L, Matet A, Dirani A, Daruich A, Ambresin A, Mantel I, Spaide RF, Turck N, Behar-Cohen F. EFFICACY OF INTRAVITREAL AFLIBERCEPT IN MACULAR TELANGIECTASIA TYPE 1 IS LINKED TO THE OCULAR ANGIOGENIC PROFILE. Retina. 2017 Dec;37(12):2226-2237. doi: 10.1097/IAE.0000000000001424. |
|
2 |
Rao P, Dedania VS, Drenser KA. Congenital X-Linked Retinoschisis: An Updated Clinical Review. Asia Pac J Ophthalmol (Phila). 2018 May-Jun;7(3):169-175. doi: 10.22608/APO.201803. Epub 2018 Apr 9. |
|
3 |
Carelli V, Carbonelli M, de Coo IF, Kawasaki A, Klopstock T, Lagrèze WA, La Morgia C, Newman NJ, Orssaud C, Pott JWR, Sadun AA, van Everdingen J, Vignal-Clermont C, Votruba M, Yu-Wai-Man P, Barboni P. International Consensus Statement on the Clinical and Therapeutic Management of Leber Hereditary Optic Neuropathy. J Neuroophthalmol. 2017 Dec;37(4):371-381. doi: 10.1097/WNO.0000000000000570. |
|
4 |
Newman NJ. From genotype to phenotype in Leber hereditary optic neuropathy: still more questions than answers. J Neuroophthalmol. 2002 Dec;22(4):257-61. doi: 10.1097/00041327-200212000-00001. |
|
5 |
Leber hereditary optic neuropathy harboring a rare m.12811 T>C mitochondrial DNA mutation. Can J Ophthalmol. 2021 Jun;56(3):e82-e84. |
|
6 |
Leber遗传性视神经病变的临床实践指南.Chin J MedGenet,March 2020,Vol.37,No.3 |
|
7 |
Gelfand JM, Nolan R, etc. Microcystic macular oedema in multiple sclerosis is associated with disease severity. Brain. 2012 Jun;135(Pt 6):1786-93 |
|
8 |
Kessel L, Hamann S, Wegener M, Tong J, Fraser CL. Microcystic macular oedema in optic neuropathy: case series and literature review. Clin Exp Ophthalmol. 2018 Dec;46(9):1075-1086. doi: 10.1111/ceo.13327. Epub 2018 Jun 20. |
|
9 |
Sundaramurthy S, SelvaKumar A, Ching J, Dharani V, Sarangapani S, Yu-Wai-Man P. Leber hereditary optic neuropathy-new insights and old challenges. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2461-2472. doi:10.1007/s00417-020-04993-1. |
Only represents the expert’s opinion and does not represent the views of Zhaoke. This article is used for the purpose of providing scientific knowledge, practical experience, cutting-edge progress, and supporting medical education, and does not constitute any advertising or sales intent, nor does it provide any advice or opinions regarding disease diagnosis and clinical treatment. The copyright of this article is protected, and it cannot be copied or reproduced without permission.