
This study aims to use frequency-domain OCT (FD-OCT) to assess the changes in GCC thickness and RNFL thickness in patients with AION, exploring the sensitivity of both metrics in evaluating AION severity.
[Clinical Research] Assessment of GCC and RNFL Thickness in AION Diagnosis
Hu Liying Li Zhiqing Li Xiaorong
300384 Tianjin Medical University Eye Hospital Tianjin Medical University School of Optometry Tianjin Medical University Eye Research Institute
Corresponding Author: Li Zhiqing
Email: [email protected]
DOI:10.3760/cma.j.issn.2095-0160.2017.10.010
[Abstract] Background Anterior ischemic optic neuropathy (AION) is a common ocular condition with a poor prognosis, where early diagnosis is crucial for visual outcomes. Frequency-domain optical coherence tomography (FD-OCT) can display the fine structure of retinal tissues in real-time and quantitatively measure the thickness of the ganglion cell complex (GCC) and retinal nerve fiber layer (RNFL) in the macular region. Previous studies have primarily used RNFL thickness to assess the loss of retinal ganglion cells (RGCs) in AION patients, while recent research indicates that GCC thickness can detect retinal structural changes in AION patients, but comparative studies on the diagnostic efficacy of RNFL thickness and GCC thickness for AION are rare. Objective To evaluate the diagnostic efficacy of OCT-measured GCC and RNFL for AION. Methods A diagnostic test study design was employed, enrolling 15 AION patients (15 eyes) who visited Tianjin Medical University Eye Hospital from December 2013 to July 2014, along with 14 age- and sex-matched normal controls (14 eyes) from the same hospital. FD-OCT was used to measure GCC thickness and RNFL thickness in the macular region, with GCC thickness metrics including the thickness above and below the 6 mm × 6 mm area surrounding the macula, and average GCC thickness, calculating focal loss volume (FLV) and global loss volume (GLV); RNFL thickness metrics included the thickness above, below, and average RNFL thickness. The differences between the AION group and the normal control group were compared. The area under the receiver operating characteristic (ROC) curve (AUC) was used to evaluate the diagnostic efficacy of the OCT-measured GCC and RNFL thickness for AION. Results Compared to the normal control group, the AION group’s macular region GCC thickness above, below, and average was significantly thinner (t=-3.402, P=0.002; t=2.690, P=0.012; t=2.913, P=0.007). The AION group’s FLV and GLV values were (8.39±4.54)μm³ and (19.57±10.66)μm³, significantly lower than the normal control group’s (0.64±0.48)μm³ and (1.14±0.91)μm³, with statistically significant differences (t=5.036, 6.723, both P<0.01). The AION group’s RNFL thickness above, below, and average was significantly thinner than the normal control group (t=2.815, P=0.009; t=2.392, P=0.024; t=2.863, P=0.008). The AUC values for FLV and GLV in AION eyes were both 1.000, while the AUCs for GCC thickness above, average, and below in the macular region were 0.871, 0.819, and 0.795, respectively; the AUCs for average RNFL thickness and RNFL thickness above and below the disc were 0.814, 0.809, and 0.762, respectively. Conclusion OCT-measured GCC thickness and RNFL thickness have comparable diagnostic abilities for AION, with FLV and GLV demonstrating strong detection capabilities for RGC layer assessment in AION patients, suggesting that GCC thickness and RNFL thickness measurements can complement each other in AION diagnosis.
[Keywords] Ischemic optic neuropathy/diagnosis; Optical coherence tomography; Retinal ganglion cells; Retina; Nerve fibers
Anterior ischemic optic neuropathy (AION) is a common ocular condition that can cause acute vision loss, predominantly seen in individuals over 45 years of age, characterized by painless vision loss, visual field defects, and disc pallor with edema. Relative afferent pupillary defect (RAPD) may be positive. AION is primarily caused by vascular degenerative diseases, inflammatory occlusion, increased blood viscosity, and low ocular blood flow; its main pathological mechanism is the obstruction of axoplasmic flow at the optic disc, leading to the necrosis and apoptosis or loss of retinal ganglion cells (RGCs). RGCs and their fibers exist in three layers: the inner plexiform layer, RGC layer, and nerve fiber layer, collectively known as the ganglion cell complex (GCC), which can thin with RGC death. In most areas of the retina, RGCs are distributed in a single layer, while in the macular region, they increase to 8-10 layers, with about half of the RGCs in the entire retina located in the macular region. The measurement of GCC and RNFL thickness around the optic disc can assess RGC loss. Optical coherence tomography (OCT), as a new imaging technique for tissue cross-sectional scanning, has high resolution, can display the fine structure of retinal tissues in real-time, and can objectively and quantitatively measure GCC and RNFL thickness with good reproducibility. Studies have reported that GCC can be used to assess neuronal damage in glaucoma; previous studies primarily assessed RGC loss in AION patients through RNFL thickness measurements, and animal studies have confirmed that OCT can dynamically observe changes in retinal nerve thickness in experimental AION mice. However, there are few studies on the relationship between RNFL and GCC changes and AION, with recent studies reporting the relationship between RNFL and GCC thickness and visual prognosis in AION patients. This study aims to evaluate the changes in GCC thickness and RNFL thickness in AION patients using frequency-domain OCT (FD-OCT) to explore the sensitivity of both metrics in evaluating AION severity.
1.1 Data
1.1.1 General Data A diagnostic test study design was used, enrolling 15 AION patients (15 eyes) who visited Tianjin Medical University Eye Hospital from December 2013 to July 2014, including 10 males and 5 females, aged 40-64 years, with an average age of (49.75±8.71) years; 11 patients had a course of 1-2 months, and 4 patients had a course of 2-3 months, with an average of (1.6±0.2) months. A control group of 14 individuals (14 eyes) with no ocular diseases was selected from staff health checks and outpatient visits at Tianjin Medical University Eye Hospital, including 8 males and 6 females, aged 40-68 years, with an average age of (47.64±9.63) years. There were no statistically significant differences in age and sex between the two groups (P=0.855, 0.586). This study was approved by the ethics committee, and informed consent was obtained from all subjects.
1.1.2 Inclusion Criteria for Subjects AION patients were included based on the criteria referenced from literature: (1) Sudden vision loss; (2) Fundoscopic examination showing local or diffuse edema of the optic disc, with possible hemorrhage at the disc margin after dilation; (3) Normal erythrocyte sedimentation rate and C-reactive protein, excluding arteritic AION; (4) Normal intraocular pressure (non-contact measurement); (5) No significant refractive medium opacities, or only mild opacities that do not affect fundus examination; (6) No history of glaucoma or family history; (7) No history of ocular surgery or trauma; (8) OCT examination SSI ≥50. Normal control subjects were included based on the following criteria: (1) Best corrected visual acuity no less than 1.0; (2) Normal intraocular pressure; (3) Normal visual field; (4) Normal fundoscopic examination after dilation, cup-to-disc ratio <0.3, no hemorrhage or notches at the disc margin; (5) No significant refractive medium opacities; (6) No history of ocular diseases or family history; (7) No history of ocular surgery; (8) OCT examination SSI ≥50.
1.2 Methods
RTVue FD-OCT (A4.0.0.143, Optovue, Inc.) examination was performed in a darkroom, with subjects receiving compounded tropicamide eye drops for dilation. Subjects were seated in front of the OCT instrument, adjusting the device so that their chin was at the same level as the chin rest and their forehead was fixed to the head frame. The chin rest height was adjusted so that the built-in camera of the OCT was perpendicular to the corneal surface of the examined eye and at the same level as the pupil, with the subject fixating on the blue cursor emitted from the OCT. The disc and GCC scanning modes were selected, with the disc scan mode being a circular scan around the optic disc RNFL with a diameter of 4 mm, displaying an RNFL thickness curve at a diameter of 3.45 mm, measuring RNFL thickness above, below, and average RNFL thickness. The GCC scanning mode was a scan of the inner retinal layers from the internal limiting membrane to the inner nuclear layer in the macular region, centered 1 mm temporally from the fovea, with a scanning range of 7 mm × 7 mm and sampling of 6 mm × 6 mm, displaying GCC thickness above, below, and average GCC thickness in the 6 mm × 6 mm surrounding the macula, calculating focal loss volume (FLV) and global loss volume (GLV). Images with SSI ≥50 were saved.
1.3 Statistical Methods
Statistical analysis was performed using SPSS 17.0 software. The data for each examination index were verified to be normally distributed using the W test, expressed as x±s. An independent two-sample t-test was used to compare differences in GCC thickness above, below, and average GCC thickness, FLV, GLV, and average RNFL thickness above, below, and average RNFL thickness between the AION group and the normal control group. Receiver operating characteristic (ROC) curves were plotted, and the area under the curve (AUC) was calculated, with AUC ≥0.9 indicating high diagnostic efficacy, 0.7≤AUC<0.9 indicating moderate diagnostic efficacy, and 0.5≤AUC<0.7 indicating low diagnostic efficacy.
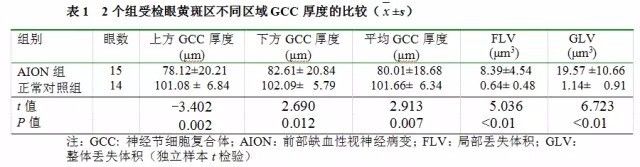
2.1 Comparison of GCC Thickness in Different Areas of the Macular Region between the Two Groups
Compared to the normal control group, the AION group’s macular region GCC thickness above, below, and average was significantly thinner, with statistically significant differences (t=-3.402, P=0.002; t=2.690, P=0.012; t=2.913, P=0.007). Compared to the normal control group, the AION group’s FLV and GLV were significantly larger, with statistically significant differences (t=5.036, 6.723, both P<0.01) (Table 1).
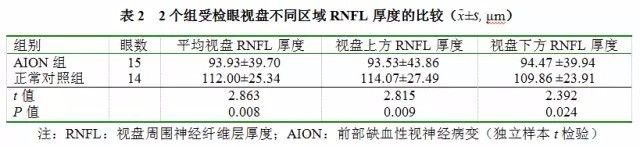
2.2 Comparison of RNFL Thickness in Different Parts of the Optic Disc between the Two Groups
Compared to the normal control group, the AION group’s RNFL thickness above, below, and average was significantly thinner, with statistically significant differences (t=2.815, P=0.009; t=2.392, P=0.024; t=2.864, P=0.008) (Table 2).
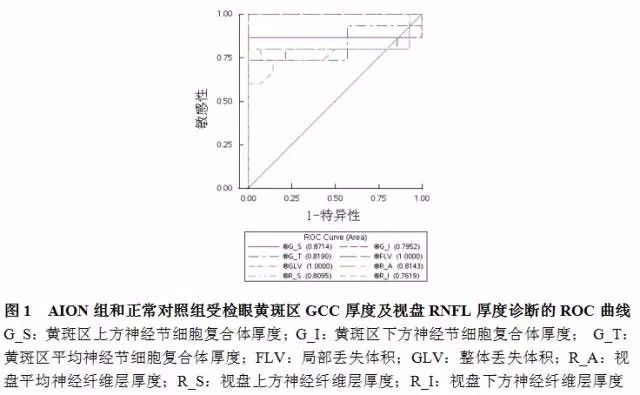
2.3 Accuracy of OCT-Measured GCC and RNFL Thickness in AION Diagnosis
All OCT parameters measured had diagnostic significance for AION, but the diagnostic abilities varied among parameters. The AUC values for FLV and GLV were both 1.000, indicating the highest diagnostic ability, while the AUC values for GCC thickness above, average, and below in the macular region were 0.871, 0.819, and 0.795, respectively; the AUC values for average RNFL thickness and RNFL thickness above and below the disc were 0.814, 0.809, and 0.762, respectively (Figure 1).
AION is a common optic nerve condition that often leads to severe visual impairment, with an incidence second only to glaucoma. AION may initially present as optic disc congestion and edema, progressing to RGC and axonal loss, and optic nerve atrophy. Early diagnosis of AION is a critical factor affecting visual prognosis, as timely and effective treatment can preserve or restore some visual function in patients. Therefore, exploring early diagnostic methods for AION is of significant clinical importance.
AION is caused by ischemia in the prelaminar region, leading to RGC loss and optic nerve atrophy, resulting in visual field defects. The extent of visual field defects and the degree of RGC loss depend on the affected RGC regions. Current research has focused on RNFL loss, but since the macular region is where RGCs are concentrated, further exploration is needed to determine whether changes in thickness in this area can contribute to the early diagnosis and monitoring of AION. In recent years, the rapid development of FD-OCT technology has made precise measurement of GCC thickness in the macular region possible, providing an objective and effective method for measuring RNFL thickness in AION patients. Studies have shown that FD-OCT can accurately measure GCC loss, aiding in the clinical diagnosis of AION and the observation of its characteristics; therefore, this study aims to explore the diagnostic capability of FD-OCT in detecting RGC loss in AION patients and assess which measurement—GCC thickness or RNFL thickness—is more sensitive for monitoring AION severity. The results of this study indicate that compared to the normal control group, AION patients have significantly reduced GCC in the macular region and significantly thinner RNFL, suggesting RGC loss in the macular region of AION patients. Existing literature has reported thinning of both GCC and RNFL thickness in AION patients using FD-OCT, consistent with the results of this study.
The results of this study show that the AUC values for FLV and GLV measured by OCT are both 1.000, confirming the high diagnostic value of these indicators for AION. The ROC values for average GCC thickness and GCC thickness above and below the macula in distinguishing AION patients from normals ranged from 0.795 to 0.871; the AUC values for average RNFL thickness and RNFL thickness above and below the disc ranged from 0.762 to 0.814, indicating moderate diagnostic efficacy for these measurements. This suggests that both GCC and RNFL thickness measurements can play complementary roles in assessing RGC loss in AION patients. Gonul et al. reported that GCC had a higher AUC value for diagnosing and assessing AION compared to RNFL, but the difference was not statistically significant, while FLV and GLV had the highest diagnostic value, consistent with our findings. Tan et al. suggested that FLV and GLV are more effective for diagnosing glaucoma than measuring GCC thickness alone.
In conclusion, this study using the new generation of FD-OCT found that GCC thickness in AION patients is significantly reduced, and both GCC thickness measurement and RNFL thickness measurement have comparable diagnostic efficacy for AION. FLV and GLV have the strongest diagnostic capabilities for assessing the GCL in AION patients. Therefore, GCC scanning in the macular region can serve as a complementary or alternative method to RNFL examination. The findings of this study provide new insights for diagnosing AION; however, due to the small sample size included, further clinical studies with larger samples are needed to validate these results.
References: Omitted
Source: Selected from Medical Space Strategic Partners[Journal of Chinese Experimental Ophthalmology], please indicate the source when reprinting!

Medical Space – Making Connections Valuable
Four main modules: MS.TV, Medical Literature, Industry News, Medical Friends Circle

Long press to scan the QR code Follow 
·END·
