The history of medicine is a process of “Shennong tasting hundreds of herbs”. Aside from daily experiments, many groundbreaking advances and discoveries are often accidental.
As spring arrives, more friends around me are sneezing and coughing. Most people will buy antibiotics like cephalosporins at the slightest cough or runny nose, but are antibiotics really effective for colds?
Let’s start with the ancestor of antibiotics—penicillin.
1
Discovery of Antibiotics
In 1928, British scientist Alexander Fleming discovered penicillin. It is said that Fleming inoculated bacteria onto a petri dish for experiments and then forgot to clean the dish before going on vacation for three weeks.
When the microbiologist returned to the lab, he found that the petri dish, full of bacteria, was contaminated with a mold, and there was no bacterial growth around this mold. Thus, penicillin was finally discovered.
As a groundbreaking antibacterial drug, penicillin saved countless soldiers’ lives during World War II. At that time, the leading cause of death among soldiers was not gunshot wounds, stab wounds, or blood loss, but bacterial infections during treatment in field hospitals. When penicillin was applied to assist soldiers’ treatment and prevent wound infections, the results were remarkable.

Later, penicillin was used effectively for pneumonia, meningitis, and purulent pharyngitis, extending the average human lifespan by 15 years and solidifying its status as a “miracle drug”.
2
Why Are Antibiotics Used for Colds?
In English, a cold is referred to as a common cold, which literally translates to an ordinary cold, something common and usual. The common cold is a common acute viral infection of the upper respiratory tract, clinically manifested by nasal congestion, sneezing, runny nose, fever, cough, and headache.
Modern medicine considers the common cold to be a self-limiting disease, meaning it does not require special treatment and can heal on its own through the immune system. The typical duration of a common cold is about 7 days, with recovery time varying based on individual immunity.
Many years ago, doctors believed that the common cold could lead to bacterial complications, such as bacterial pharyngitis and tonsillitis. Influenced by the then “miracle drug” penicillin, it was commonly believed that using antibiotics for patients with common colds could prevent these complications.
Before the founding of the People’s Republic of China, penicillin in our country was largely dependent on imports, and its price was even more precious than gold. The book “The Rise of the Antibiotic Industry in the East” mentions that a 20,000-unit, 0.12 g vial of penicillin was equivalent to 0.9 g of gold or 13.1 kg of rice. The powerful efficacy of penicillin also delighted doctors at that time.
By the 1950s to 1970s, the fermentation and extraction processes for the four major antibiotics (penicillin, streptomycin, tetracycline, and oxytetracycline) were developed. Antibiotics were no longer reliant on imports, and their prices became more reasonable, leading to broader clinical applications.
The dangers of antibiotics were not noted until the 1970s and 1980s, when studies began to investigate the harm of antibiotics to the human body. A World Health Organization survey showed that the rate of antibiotic use among hospitalized patients in China reached as high as 80%, with the ratio of broad-spectrum antibiotics and the combined use of more than two antibiotics reaching 58%, far exceeding the international level of 30%.

Let’s review: the common cold is caused by a virus and is a self-limiting disease that can heal on its own through the immune system. Antibiotics target bacteria and can kill bacteria by reaching a certain concentration in the bloodstream throughout the body, preventing bacteria from damaging the body. Thus, antibiotics have no effect on the common cold and are even a misuse of medication!
Professor Chen Daijie from Shanghai Jiao Tong University mentioned in a speech that “the development and spread of bacterial resistance is very rapid, while the development of new antibiotics is severely lagging behind.” When superbugs outpace humans, it means we have no medicine to treat them.
To combat self-limiting diseases like the common cold, the most important thing is to enhance one’s own immunity.
3
What Is Immunity?
Immunity is a defense mechanism of the body that helps maintain stability and health. First, let’s clarify the often-confused concepts of antigens and antibodies.
Antigen: A substance that can specifically recognize and bind to T lymphocytes and B lymphocytes, triggering a specific immune response and can bind specifically to corresponding products inside and outside the body. Antigens can be bacteria, viruses, or even pollen or some components within the body; in general, antigens are substances that can provoke an immune response.
Antibody: A substance synthesized and secreted by B lymphocytes after an immune response, which can bind to antigens, marking them to induce other immune mechanisms to attack the antigens. In other words, antibodies do not possess aggressiveness; they act as GPS messengers, telling the body which are the “bad guys” (antigens).
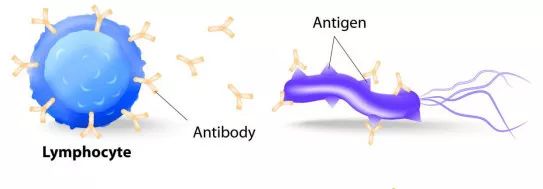
(Image: Lymphocyte: Lymphocyte; Antibody: Antibody; Antigen: Antigen)
The immune response in the body is like two countries at war; antigens are the enemy troops, and the immune system is our defending army.
First, the enemy troops (antigens) attack, breaking through the body’s first line of defense (skin, mucous membranes, and their secretions).
At this point, the enemy troops (antigens) enter the central battlefield (body fluids), and our second line of defense—patrolling soldiers (phagocytes and antimicrobial substances in body fluids)—is ready to take out the enemy troops.

In fact, most of the enemy troops are eliminated at the first and second lines of defense, but a few stubborn enemies escape the pursuit of the patrolling soldiers and gradually grow within the body.
At this time, the body’s third line of defense (immune organs and immune cells) must be activated. The patrolling soldiers (phagocytes, etc.) report the enemy situation to the commander (T lymphocytes), and after careful consideration, the commander takes the following strategies:
First move: T lymphocytes proliferate and differentiate, personally engaging the enemy troops, and will also carry some weapons like lymphokines, etc. (This is cellular immunity, simply understood as the commander splitting into many to eliminate the enemy troops).
Second move: The commander (T lymphocytes) gives orders to the GPS troops (B lymphocytes), and thus the GPS troops begin tracking and locating, dispatching small GPS (antibodies) to attach to the enemy troops. With these small GPS (antibodies), the patrolling soldiers of the second line of defense and the proliferated T lymphocytes can quickly, accurately, and fiercely deal with the enemy troops.
Through this battle, our army (immune system) achieves victory.

From this, we also know that there are four key roles in the immune response—patrolling soldiers (phagocytes, etc.), the commander (T lymphocytes), GPS troops (B lymphocytes), and small GPS (antibodies). To enhance immunity, we need to improve the combat capabilities of these four.
In daily life, we often say to supplement vitamin C, which, aside from its skin-whitening effects favored by women and its prevention of the now-rare scurvy, is more importantly known for enhancing immunity.
Unsubstantiated effects are pointless. As mentioned above, we will discuss how vitamin C affects these four key roles to enhance immunity.
4
How Does Vitamin C Enhance Immunity?
Patrolling Soldiers (Phagocytes, etc.)
Phagocytes are an important component of the immune system. Vitamin C enhances immunity by regulating Th1 cytokines to activate macrophages (a type of phagocyte) to eliminate pathogens. Additionally, vitamin C is a strong antioxidant that inhibits lipid peroxidation, reducing or avoiding damage to phagocytes, thereby strengthening immunity.

Commander (T Lymphocytes)
T lymphocytes are indispensable regulatory cells in the immune system. Current in vitro and in vivo experiments indicate that vitamin C enhances immune function by promoting T cell development or inhibiting IL-2-dependent T cell growth activity.

GPS Troops (B Lymphocytes)
Vitamin C has two potential effects on B lymphocytes: (1) Vitamin C indirectly affects B lymphocytes by acting directly on other immune cells (dendritic cells). (2) Vitamin C directly affects B cells by regulating ROS (reactive oxygen species) levels within B cells through its own chemical or antioxidant actions.

Small GPS (Antibodies)
The production of antibodies is primarily the result of the combined actions of T lymphocytes, B lymphocytes, and phagocytes. Vitamin C promotes the production of antibodies.

Let’s Summarize
Vitamin C is an essential nutrient and immune modulator in the human body. It corrects immune system disorders by affecting the proliferation and differentiation of various immune cells, the secretion of cytokines, and antioxidant actions, which is beneficial for the body to resist disease.
To put it simply: Vitamin C can enhance the phagocytic capacity of white blood cells, improve resistance to diseases, increase tolerance to cold, and promote the formation of antibodies in the body, thereby enhancing immune function.
References:
[1] Zhang Lixin, Gao Zhixing. Effects of High-Dose Vitamin C on Cellular Immune Function in Irritable Bowel Syndrome. Shandong Medical Journal, 2012, 52(1):90-91.
[2] Martin P, Frei B. Both intracellular and extracellular vitamin C inhibit atherogenic modification of LDL by human vascular endothelial cells. Atherosclerosis, Thrombosis, and Vascular Biology, 1997, 17(8):1583-1590.
[3] Manning J, Mitchell B, Appadurai DA, et al. Vitamin C Promotes Maturation of T-Cells. Antioxidants & Redox Signaling, 2013, 19(17):2054-2067.
[4] Yanagihara Y, Basaki Y, Kajiwara K, et al. A thiol antioxidant regulates IgE isotype switching by inhibiting activation of nuclear factor-kappaB. Journal of Allergy and Clinical Immunology, 1997, 100:33-38.
[5] Lee JR. Reactive oxygen species play roles in B cell surface receptor CD40-mediated proximal and distal signaling events: effects of an antioxidant, N-acetyl-L-cysteine treatment. Molecular and Cellular Biochemistry, 2003, 252(1-2):1-7.
[6] Guaiquil VH, Vera JC, Golde DW. Mechanism of vitamin C inhibition of cell death induced by oxidative stress in glutathione-depleted HL-60 cells. Journal of Biological Chemistry, 2001, 276(44):40955-40961.
[7] Bowie AG, O’Neill LA. Vitamin C inhibits NF-kappa B activation by TNF via the activation of p38 mitogen-activated protein kinase. Journal of Immunology, 2000, 165(12):7180-7188.
[8] Li J, Milne RW, Nation RL, et al. Pharmacokinetics of colistin methanesulphonate and colistin in rats following an intravenous dose of colistin methanesulphonate. The Journal of Antimicrobial Chemotherapy, 2004, 53(5):837-840.
[9] Evans ME, Feolad J, Rapp RP. Polymyxin B sulfate and colistin: old antibiotics for emerging multiresistant gram-negative bacteria. The Annals of Pharmacotherapy, 1999, 33(9):960-967.
[10] Zhang Chunping, Xiao Xilong, Lin Bin. Study on the Pharmacokinetics and Bioavailability of Colistin Sulfate in Pigs. Journal of Animal Husbandry and Veterinary Medicine, 2002, 33(6):598-601.
Source: Life Science Education
