Cingulate Cortex Weekly
Issue 28
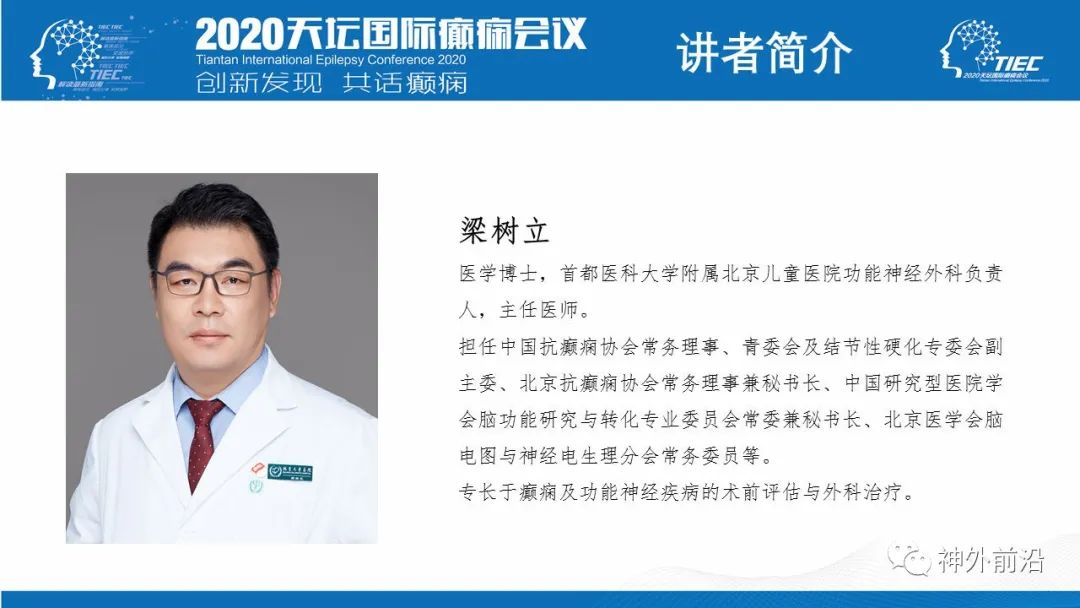
Professor Liang Shuli is a key member of the Chinese Anti-Epilepsy Association, dedicated to the research and treatment of epilepsy for many years with remarkable achievements. This lecture provides a comprehensive introduction to the anatomy, partitioning, and typical symptomatology of the anterior, middle, and posterior cingulate cortex, and discusses treatment strategies and prognostic outcomes for cingulate epilepsy through literature review and clinical examples. The content is very rich and serves as an excellent resource for learning the theories and practices related to cingulate epilepsy.
With the development of stereotactic techniques and advancements in SEEG technology, our understanding of cortical epileptogenic foci has evolved from initially focusing on superficial cortical epilepsy to recognizing more about the internal fissures and deeper cortical foci. Familiarity with the relevant anatomy and symptomatology allows us to perform SEEG implantation, which aids in precisely locating deep epileptogenic foci and improves the Engel I cure rate post-surgery, providing better relief for epilepsy patients.
Zhang Jianguo, Yang Anchao from Beijing Tiantan Hospital
Neurosurgery Frontier News: In recent years, studies on the brain network mechanisms of epilepsy, precise preoperative localization of epileptogenic foci, the development of new antiepileptic drugs, and the exploration of new treatment targets and methods have become hot topics in the field of epilepsy. Scholars at home and abroad have made significant progress in the pathophysiological mechanisms, diagnosis, prevention, and treatment of epilepsy, greatly enhancing the understanding of epilepsy among researchers and clinicians and improving clinical practice.
On August 22, 2020, at the “2020 Tiantan International Epilepsy Conference” surgical special session online meeting co-hosted by the Chinese Anti-Epilepsy Association and Capital Medical University Affiliated Beijing Tiantan Hospital, Professor Liang Shuli from the Functional Neurosurgery Department of the Beijing Children’s Hospital presented a report titled “Cingulate Cortex Epilepsy and Its Surgical Treatment”.
Professor Liang Shuli introduced that the cingulate cortex can be divided into the anterior cingulate cortex (ACC), middle cingulate cortex (MCC), and posterior cingulate cortex (PCC); the ACC is primarily related to excessive movement and emotions, the MCC is related to cognition and movement, while the PCC is mainly associated with temporal lobe epilepsy manifestations and complex subjective sensory changes.
Professor Liang Shuli summarized that the overall surgical prognosis for cingulate cortex epilepsy is relatively good; focal lesions do not necessarily require intracranial electrode and EEG examinations.
Below are the main contents of Professor Liang Shuli’s speech (content reviewed and modified by the speaker):
1. History of Cingulate Cortex Epilepsy
In 1957, Andy and Chinn proposed cingulate cortex epilepsy in an experiment with cats; in 1970, Mazars first proposed diagnostic criteria for cingulate cortex epilepsy; the 1989 ILAE classification included it as a subtype of frontal lobe epilepsy. In fact, cingulate cortex epilepsy categorized under frontal lobe epilepsy primarily refers to anterior cingulate cortex epilepsy.
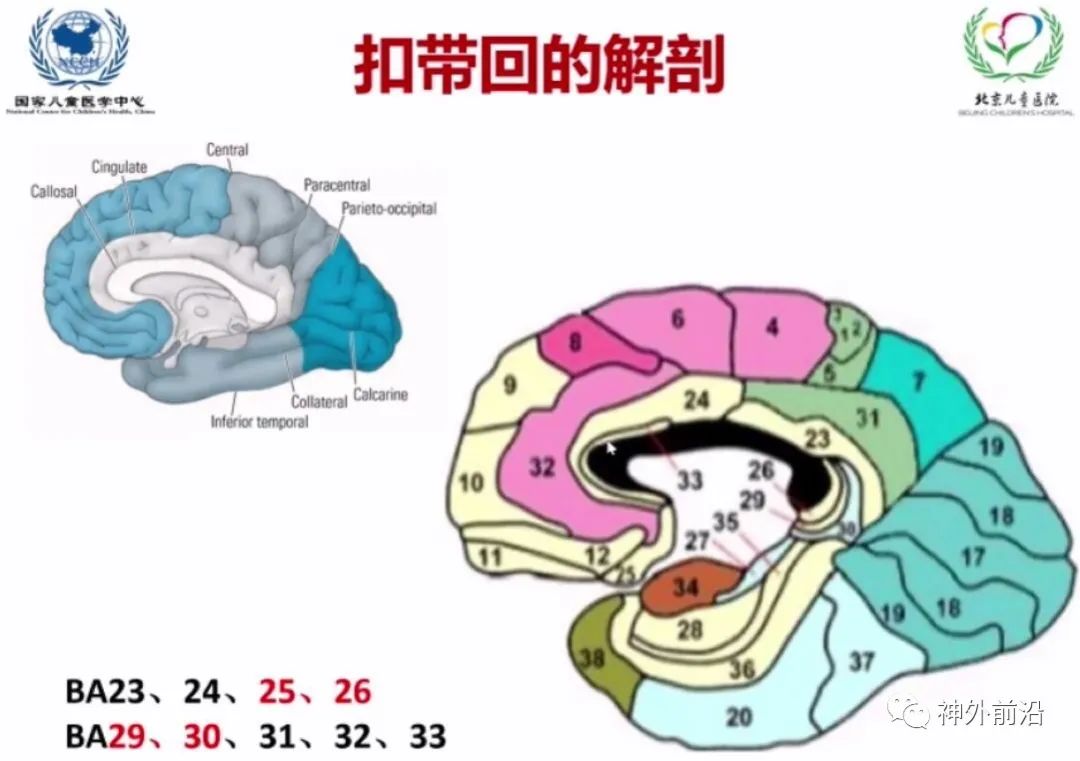
The anatomy of the cingulate cortex, according to the Broadmann areas, mainly includes the ventral BA23, BA24, BA33, dorsal BA31, BA32, as well as the subgenual area like BA25 and posterior areas BA26, BA29, BA30, making a total of 9 brain regions involved in the cingulate cortex.
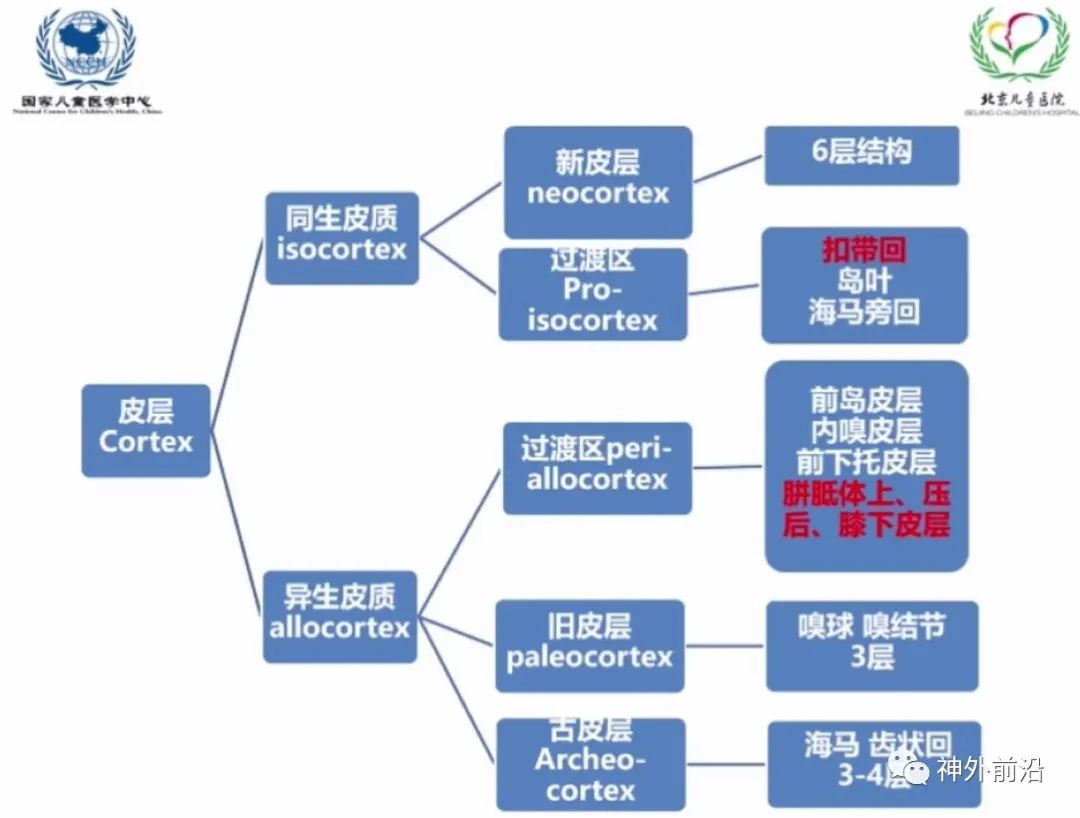
From a developmental perspective, the cortex is divided into homogenous and heterogenous cortices; the new cortex is all homogenous; the old and ancient cortices are heterogenous, but both have transitional areas. The hippocampus, which we often refer to, is actually a transitional area of homogenous cortex, while the corpus callosum and subcallosal areas are mainly transitional zones of heterogenous cortex, lacking the six-layer structure.
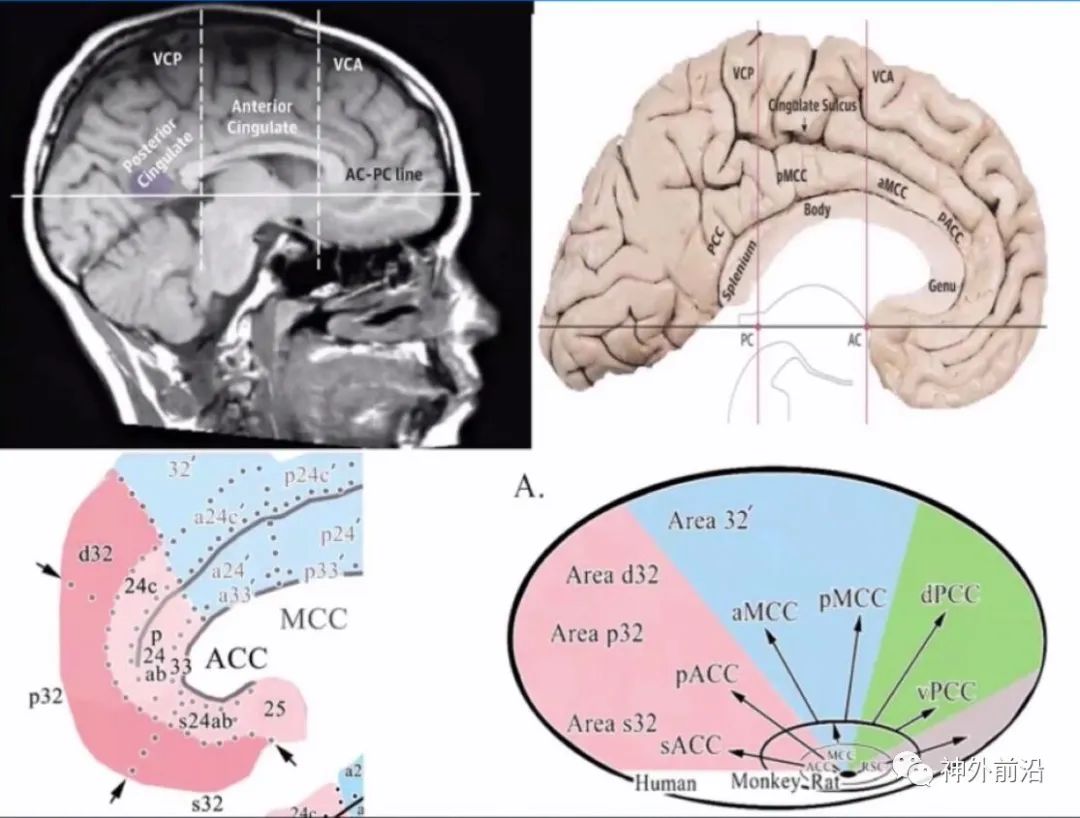
Previously, the cingulate cortex was divided into anterior and posterior parts; now it is divided into anterior, middle, and posterior parts. Based on the vertical line passing through the anterior-posterior AC-PC line, the middle is called the middle cingulate cortex, the front is the anterior cingulate cortex, and the back is the posterior cingulate cortex. Different partitions are primarily based on functional and structural divisions.
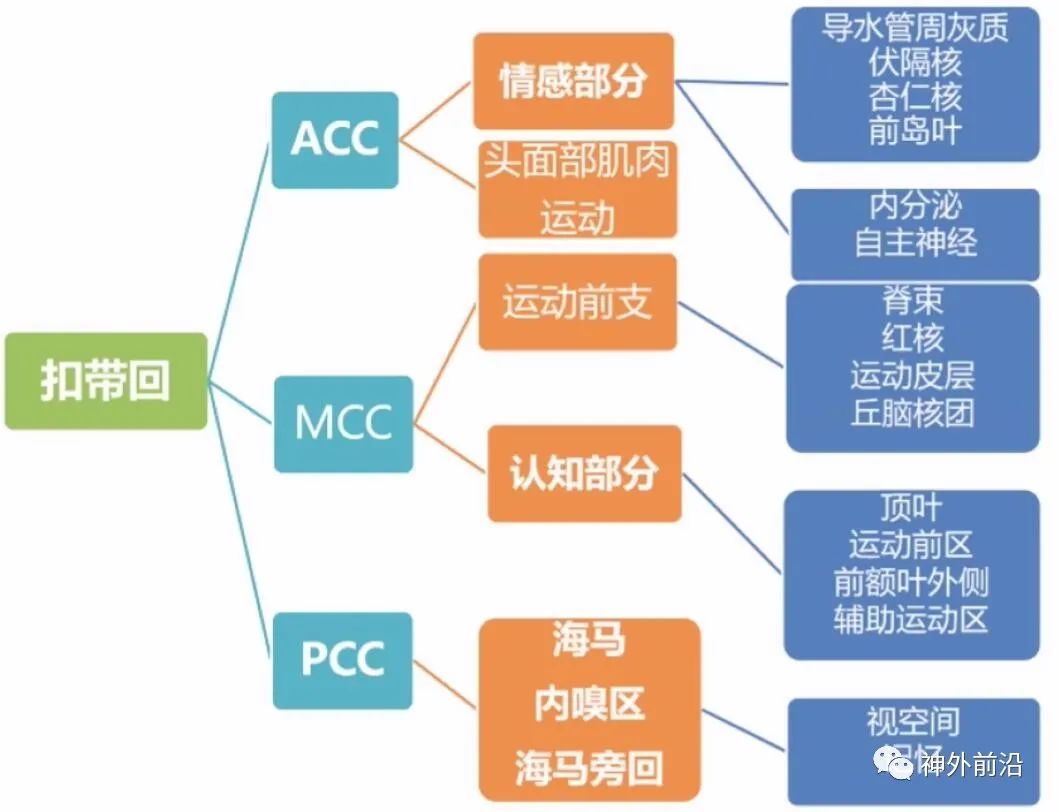
The anterior cingulate cortex, middle cingulate cortex, and posterior cingulate cortex have different functions and connections. The ACC is more related to emotions and facial muscle movements; the MCC is mainly connected with pre-movement and cognition; the PCC primarily connects with the hippocampus and entorhinal area, with the posterior cingulate cortex being closely linked to the hippocampus, while the ACC has a closer connection with the amygdala and anterior insula.
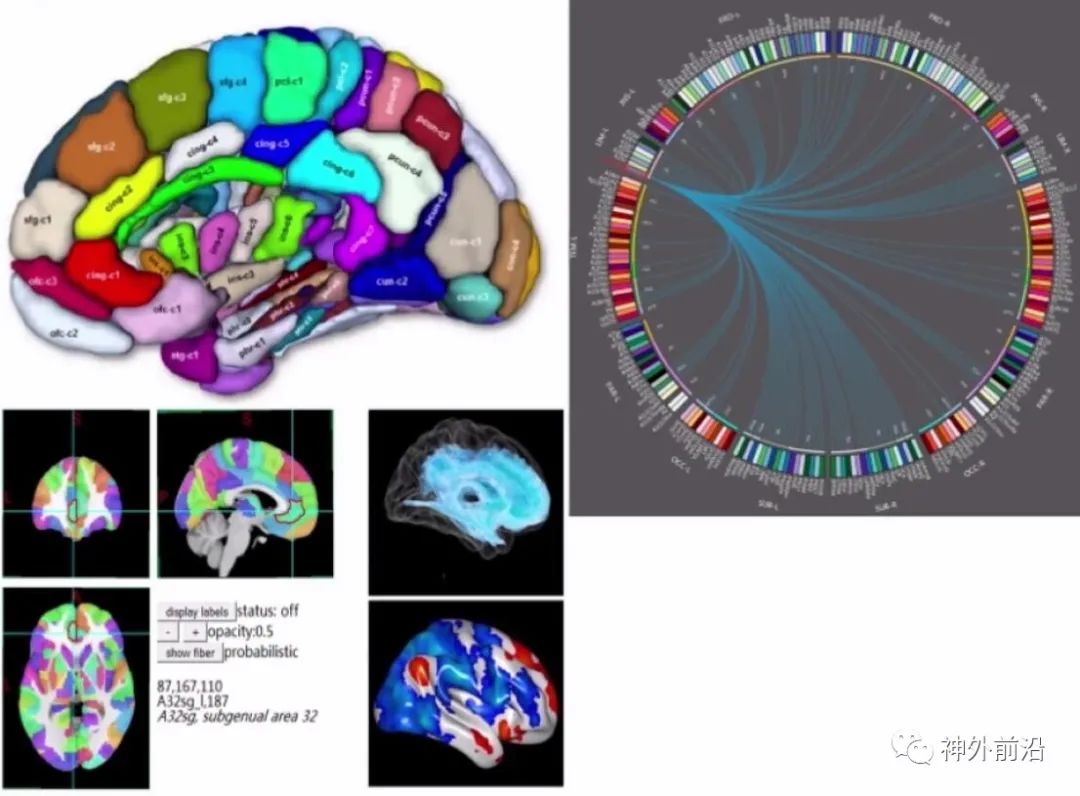
Professor Jiang Tianzi’s new brain partitioning divides the cingulate cortex into 7 areas. In the BA24 area, the cingulate cortex I area has very tight connections, which are shown to be broader through functional MRI and DTI than previously indicated by anatomical connections.
2. Anterior Cingulate Cortex Epilepsy (ACC)
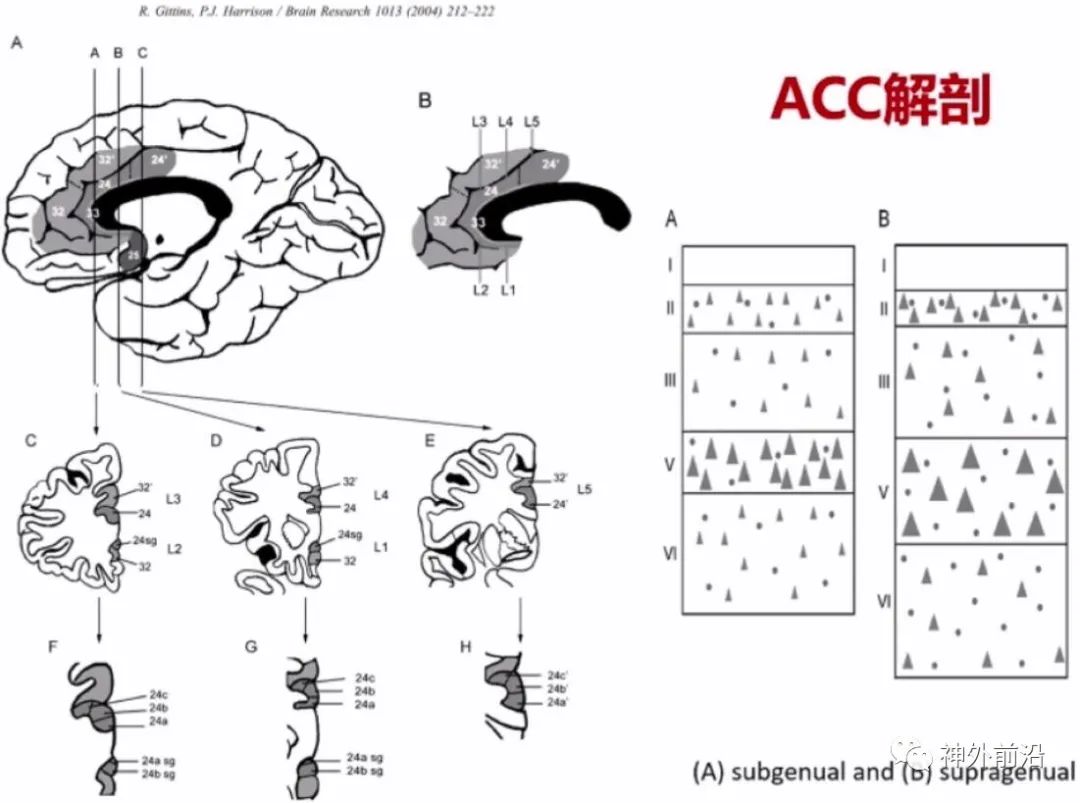
The anatomy of the ACC mainly includes areas 25, 24, the anterior part of 32, and 33; observing a slice ABC, the structures of different regions are also different, although there is no fourth layer or granular cell layer, the ACC’s anterior position is more developed than the A position.
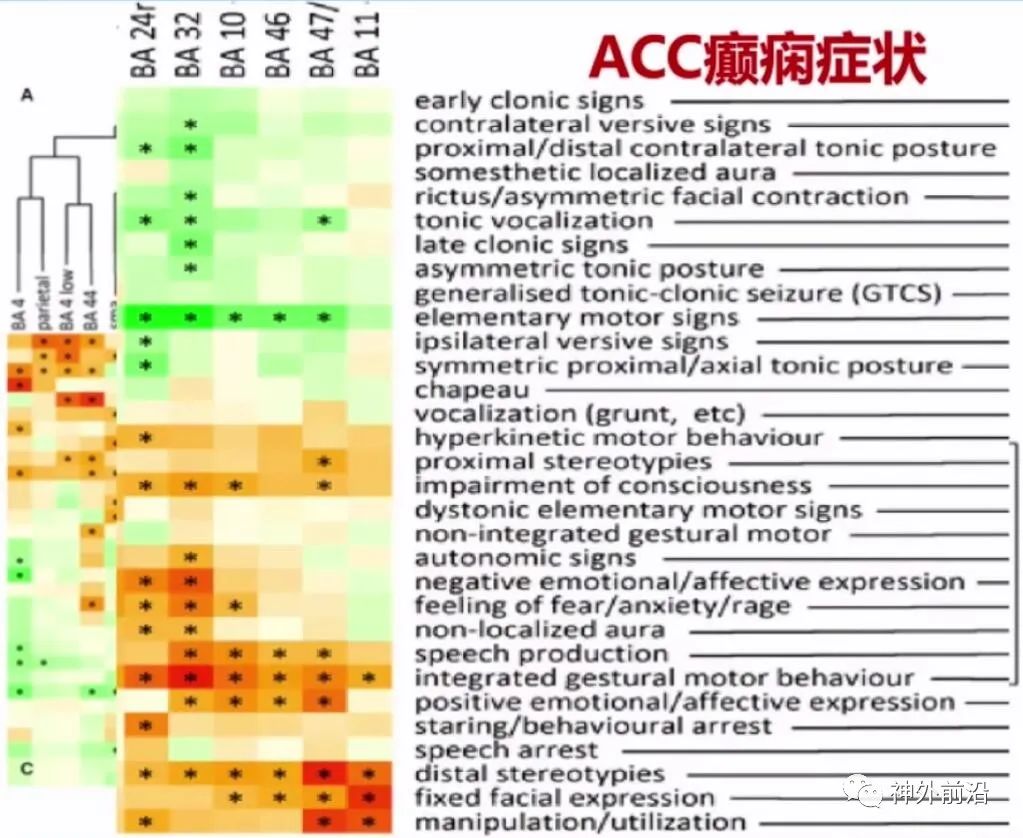
The symptoms of anterior cingulate cortex epilepsy are relatively familiar, as mentioned in an article on frontal lobe epilepsy symptoms, which also discusses the close relationship of BA24 and BA32 with emotions.
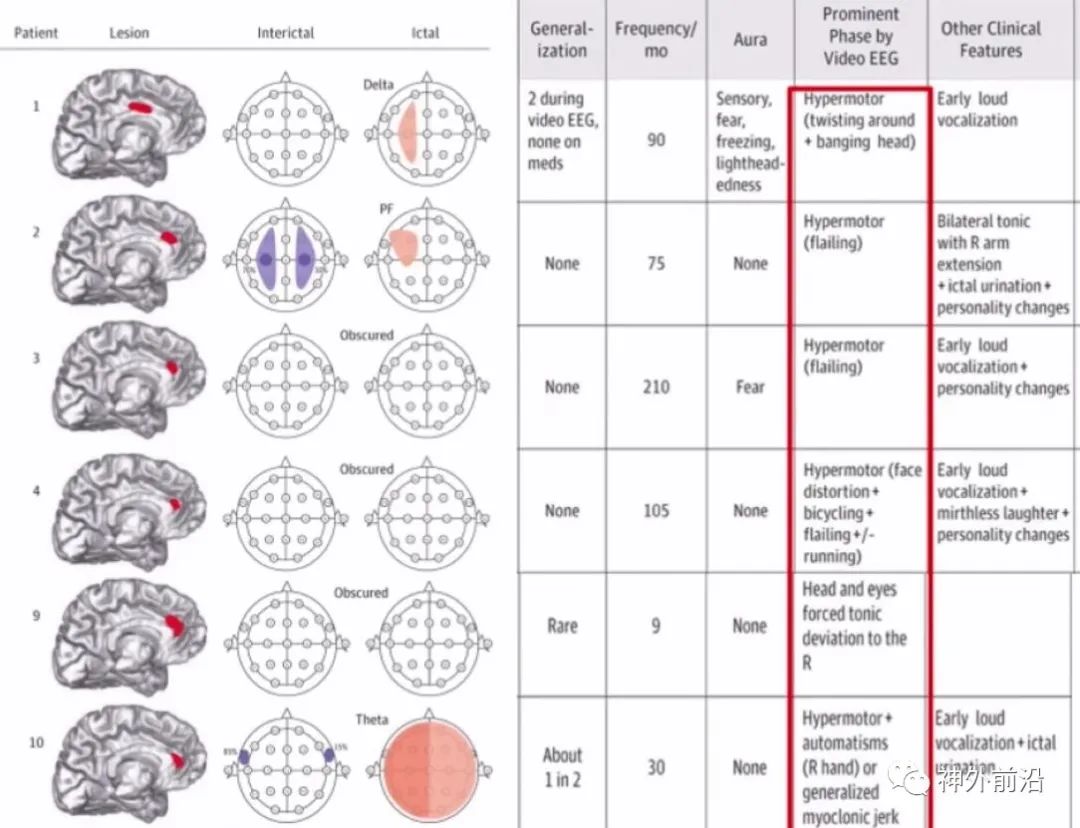
Another article reported on 6 cases of anterior cingulate cortex epilepsy. First, looking at the interictal EEG, 4 cases were normal, showing no obvious discharges, 1 case had bilateral central parietal discharges, and another had bilateral temporal discharges. Thus, there was neither lateralizing nor clear localization value.
Looking at the ictal EEG, among the 6 cases, 3 showed no focal abnormalities, 1 had bilateral widespread discharges, and 2 seemed to have lateralizing value, 1 in the frontal area and 1 in the central parietal area. However, the symptomatology was quite characteristic, with 5 out of the 6 cases exhibiting excessive movement symptoms. Excessive movement symptoms are quite prominent in the anterior cingulate cortex.
Additionally, another article reported that 3 patients had excessive movement symptoms, indicating anterior cingulate cortex lesions.
【First Symptom: Excessive Movement】
Excessive movement can be divided into two types, Type I and Type II. Type I shows more significant agitated behavior and excessive movement, along with more pronounced facial emotional expressions of fear and anger, and autonomic symptoms, with little response to external stimuli. Type II is relatively atypical, and the facial emotional and autonomic manifestations are also atypical, with some patients having partial memory of external stimuli.
The relationship between excessive movement and the anterior cingulate cortex generally divides the ACC into two parts: the anterior cingulate cortex mouth area and the anterior cingulate cortex back area. The mouth area mainly exhibits Type I symptoms, while the back area mainly shows Type II symptoms.
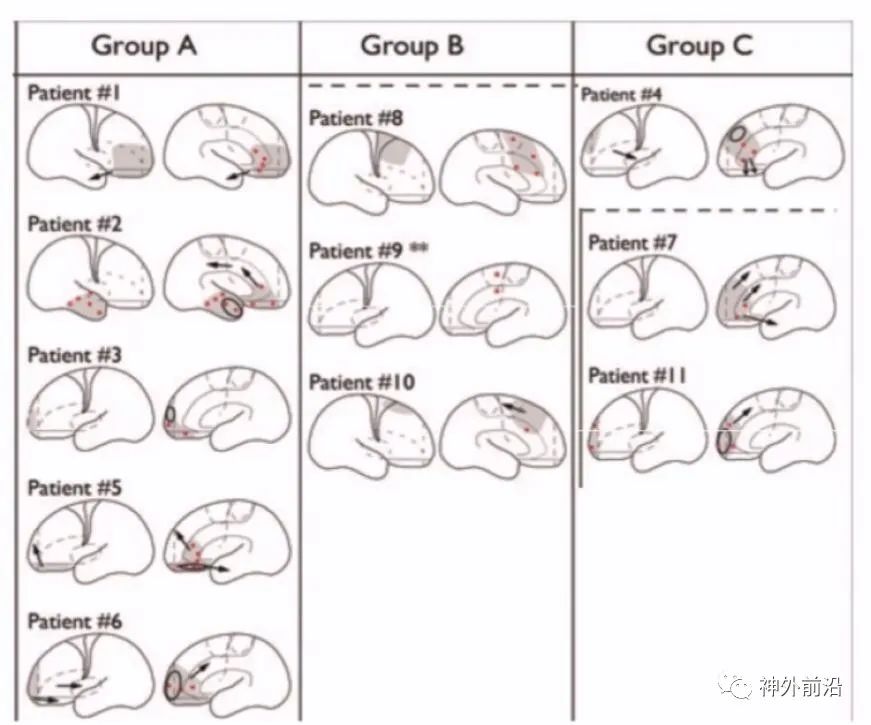
If it is more anterior, Group A shows excessive movement Type I symptoms, while Group B is more posterior, showing Type II symptoms, and Group C, which is in between, may exhibit either Type I or Type II symptoms.

Excessive movement is not a unique symptom of the anterior cingulate cortex; as pointed out in a paper by Professor Yutao from Xuanwu Hospital, excessive movement symptoms can also occur in the temporal and insular lobes. Excessive movement is a significant manifestation of the anterior cingulate cortex but does not have unique localization significance.
【Second Symptom: Fear】
Fear is closely linked to the amygdala and anterior insula; in conditioned reflexes, it is believed that the lateral and central nuclei of the amygdala and their projections to the brainstem and hypothalamus are involved in fear response control. Besides the medial frontal lobe anterior cingulate cortex, other areas such as the nucleus accumbens, amygdala, and gray matter around the cerebral aqueduct also participate in fear responses.
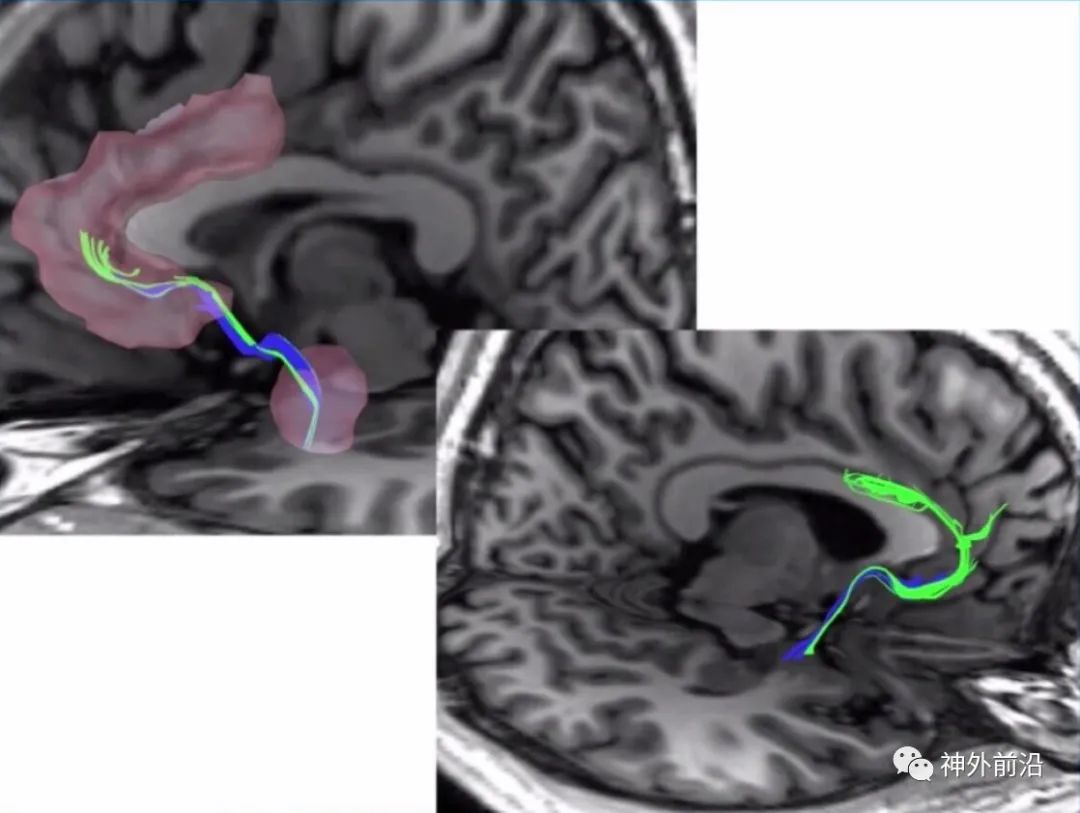
Currently, fiber bundle diffusion spectrum imaging (DSI) can show the medial frontal lobe and amygdala with clear fiber connections.
【Third Symptom: Laughter】
This is also an emotional symptom where laughter is related to lesions, which can occur not only with hypothalamic hamartomas but also in the frontal lobe, midbrain, pons, and cingulate cortex. fMRI shows that areas such as the superior temporal gyrus, superior temporal sulcus, fusiform gyrus, and amygdala may be associated with laughter. Studies indicate that laughter from tickling is related to the superior temporal gyrus, while genuine emotional laughter may be related to the anterior cingulate cortex.
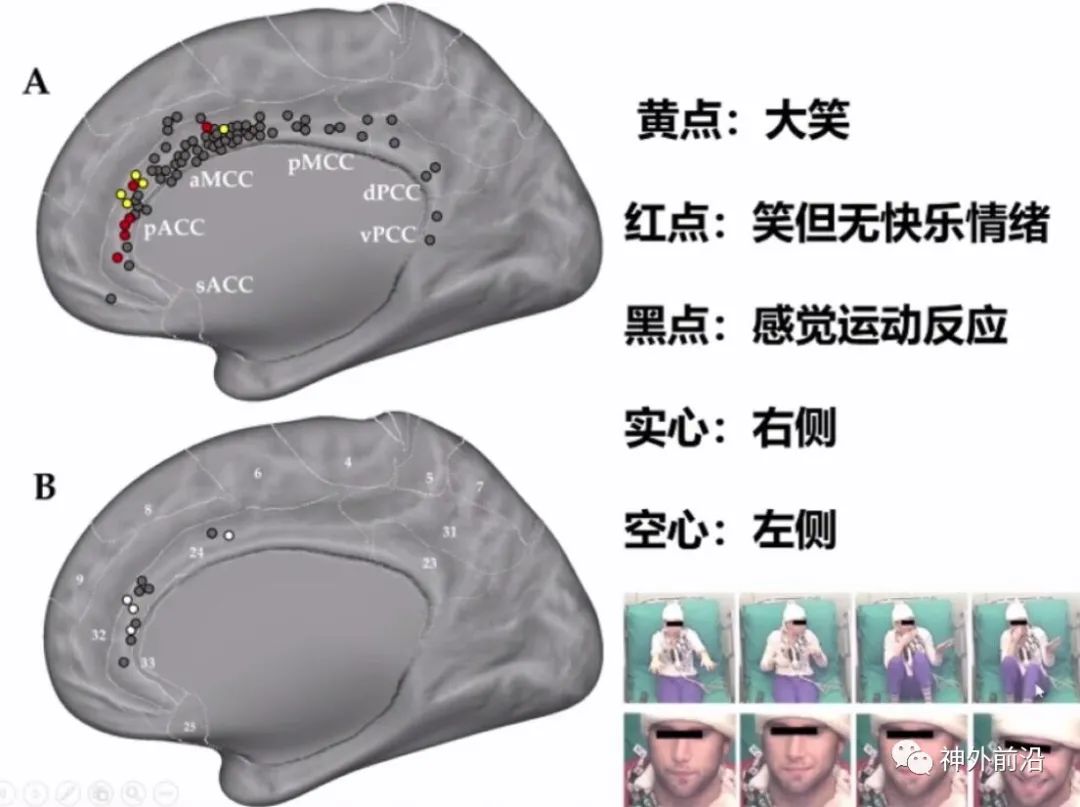
In this article, the yellow dots indicate laughter, which stimulates laughter, while the red dots stimulate laughter without evoking happy emotions. Research shows that patients initially do not respond, but later exhibit laughter actions after increasing the stimulus intensity, indicating laughter emotions.
Besides hypothalamic hamartomas, laughter-related epilepsy has been statistically reported in 93 cases from 1953 to 2014, with only 27 cases having clear localization, of which 5 were in the medial temporal lobe and 3 in the lateral temporal lobe, with the most being anterior cingulate cortex at 11 cases, as well as frontal operculum and insula.
Caruana (Emotion, 2017) reported that stimulating the anterior ACC can trigger laughter, and recognizing laughter expressions also activates the ACC, indicating its importance in laughter production and expression recognition.
It can be observed that when a female celebrity’s smiling expression is seen, the anterior cingulate cortex is activated; however, hearing laughter does not activate it. The smiling expression is more likely to induce anterior cingulate cortex epilepsy, indicating its significance.
【Fourth: Pouting/Disgust】
Commonly known as the “gendarme hat sign”, this is actually the expression of disgust characterized by pouting, as noted in a 2014 paper, where the authors reported on 79 cases of frontal lobe resections from 1992 to 2001, with 55 patients remaining seizure-free for more than two years, and complete data available for 36 cases.
In these 36 cases, 11 patients exhibited pouting actions. Some resections were relatively limited, while most had a broader range; both anterior cingulate cortex initiation and affected areas were included. From this perspective, the pouting action may be closely related to the anterior cingulate cortex but does not necessarily indicate its initiation.
Many articles, such as those on the insula and insular operculum, indicate that as long as the pathways connect to the anterior cingulate cortex, similar symptoms can occur; the cingulate cortex can produce oropharyngeal automatisms, and electrical stimulation of the cingulate cortex can change vocalization.
3. Middle Cingulate Cortex (MCC)
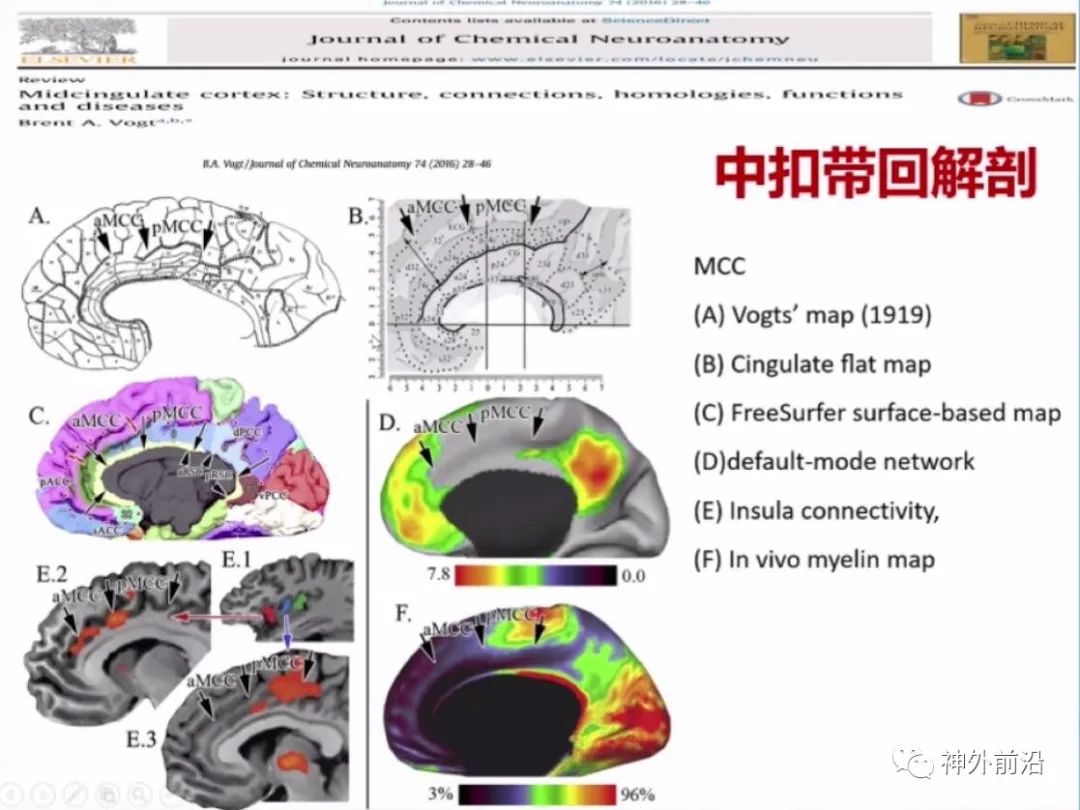
The middle cingulate cortex was differentiated later, with very few references to it before 2000, but since 2010, the concept of the middle cingulate cortex has gained wider acceptance. As early as 1919, the scope of the middle cingulate cortex was defined, and it was divided into anterior and posterior middle cingulate cortex.
From cellular architecture and analyses based on Freesurfer or default networks, the three arrows indicate the locations of the anterior, middle, and posterior cingulate cortex, showing significant differences in various analyses.
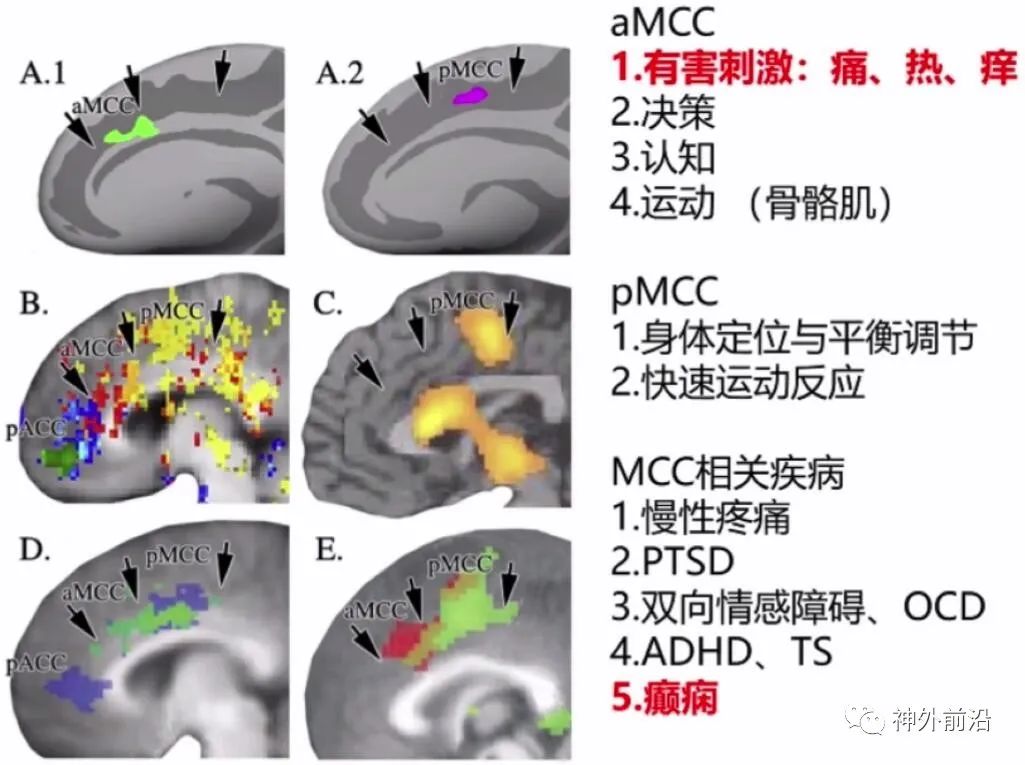
The middle cingulate cortex is associated with many diseases, including pain, PTSD, OCD, ADHD, TS, and epilepsy.
【Case A-1】
We look at a case of middle cingulate cortex epilepsy. An 8-year-old male, right-handed, with onset at age two, exhibited asymmetric tonic seizures lasting about 20 seconds. Scalp EEG showed spike waves in the central parietal area, with the most significant discharges at Cz and FCz during seizures; MRI and PET-CT were negative. Subdural electrodes covering the bilateral dorsal and medial frontal lobes showed discharges originating from the anterior medial frontal area of the left supplementary motor area.
During craniotomy, a focal resection of the left dorsal medial frontal lobe was performed, with no significant functional impairment post-surgery, but epilepsy did not improve. A year later, preoperative assessments showed the same EEG pattern as before surgery, with seizures starting more left lateralized, with F3 and FC3 showing discharges, and MRI displayed the resection site; subsequently, deep electrode implantation was performed, leading to another surgical resection, revealing FCD type II, with a reduction in seizures, but still some episodes. Finally, SEEG implantation was performed, indicating that the resection range was still too shallow, leading to a middle cingulate cortex resection. Electrical stimulation results showed that the cingulate cortex preferentially spreads externally rather than internally, indicating that the dorsal cingulate cortex has motor functions.
As previously mentioned, the article included 5 cases of middle cingulate cortex epilepsy, with interictal and ictal EEG showing no localization significance. Among the 5 patients, 3 exhibited excessive movement, while the posterior cases may have shown excessive movement Type II, indicative of transitional movement.
【Case A-2】
A 48-year-old male developed epilepsy after trauma, experiencing fearful abnormal sensations, kicking and hitting when out of bed, with awareness, possibly exhibiting both Type I and Type II symptoms. MRI showed widespread abnormal signals in the middle and posterior cingulate cortex, with abnormal signals in the frontal operculum, indicating possible brain softening or scarring, showing low metabolism in the lesion area, with the middle cingulate cortex being more pronounced. PET showed bilateral low metabolism, with EEG not very notable. SEEG implantation combined with high-frequency analysis indicated that the middle cingulate cortex lesion led to discharge initiation, resulting in resection of this area, with satisfactory control of seizures post-surgery.
Research conclusion: The implanted electrodes covered the frontal lobe, middle cingulate cortex, and posterior cingulate cortex, concluding that excessive movement can occur independently within the cingulate cortex, and the conduction of excessive movement is better outside the cingulate cortex than within it. Middle cingulate cortex epilepsy does not necessarily conduct first to the posterior or anterior cingulate cortex but may first conduct to the contralateral side or to the frontal lobe cortex.
4. Posterior Cingulate Cortex Epilepsy (PCC)
Currently, research on posterior cingulate cortex epilepsy is more extensive. Wada’s 1995 publication reported that stimulation of the posterior cingulate cortex produced gaze-evoked non-convulsive seizures. Later studies suggested that while symptoms of posterior cingulate cortex epilepsy may not be obvious, they can diffuse to other brain lobes and produce clinical symptoms, with some studies indicating complex subjective sensations such as “out-of-body experiences” and asymmetric tonic seizures.
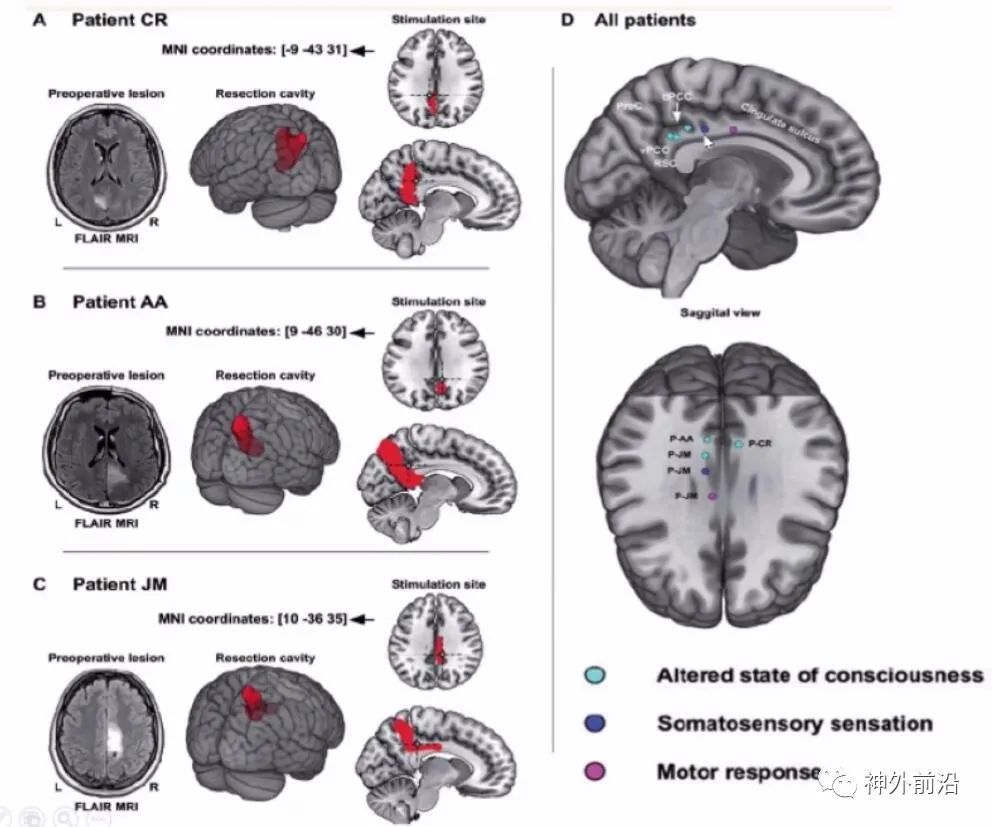
Here are three cases of posterior cingulate cortex epilepsy. During cortical stimulation, anterior stimulation can produce excessive movement symptoms, while posterior stimulation mainly results in altered states of consciousness. Further posterior can lead to sensory symptoms, and even further back primarily affects consciousness, indicating that posterior cingulate cortex is mainly involved in altered states of consciousness.
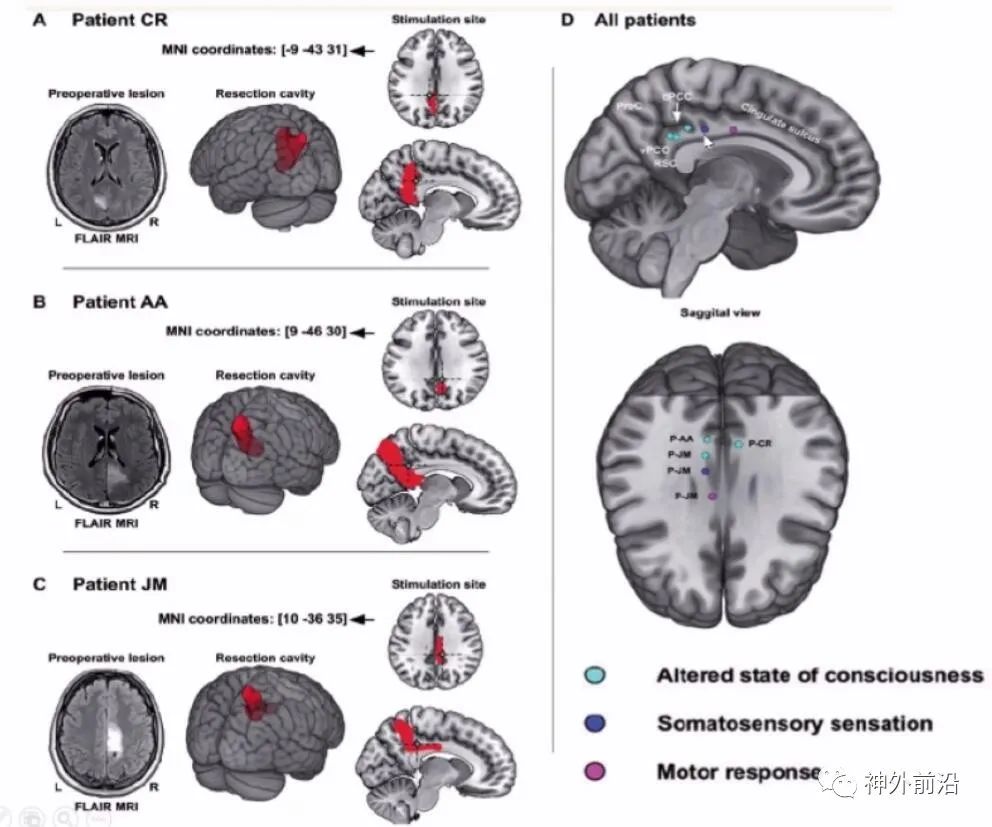
Similarly, the earlier article included 4 cases of posterior cingulate cortex epilepsy, suggesting some lateralizing significance, though the localization value remains poor. Notably, no excessive movement symptoms were observed.
【Case A-3】
A 22-year-old male, right-handed, mainly experienced CPS and occasional GCTS, with gaze and unresponsive episodes, oropharyngeal automatisms, postictal confusion, and occasional abnormal postures in the right hand, experiencing several seizures monthly while on antiepileptic medication. EEG showed discharges in the right temporal area. MRI revealed a small lesion in the posterior cingulate cortex. Intracranial electrodes and high-frequency discharges confirmed that the seizures originated from the posterior cingulate cortex.
5. Surgical Outcomes for Cingulate Cortex Epilepsy
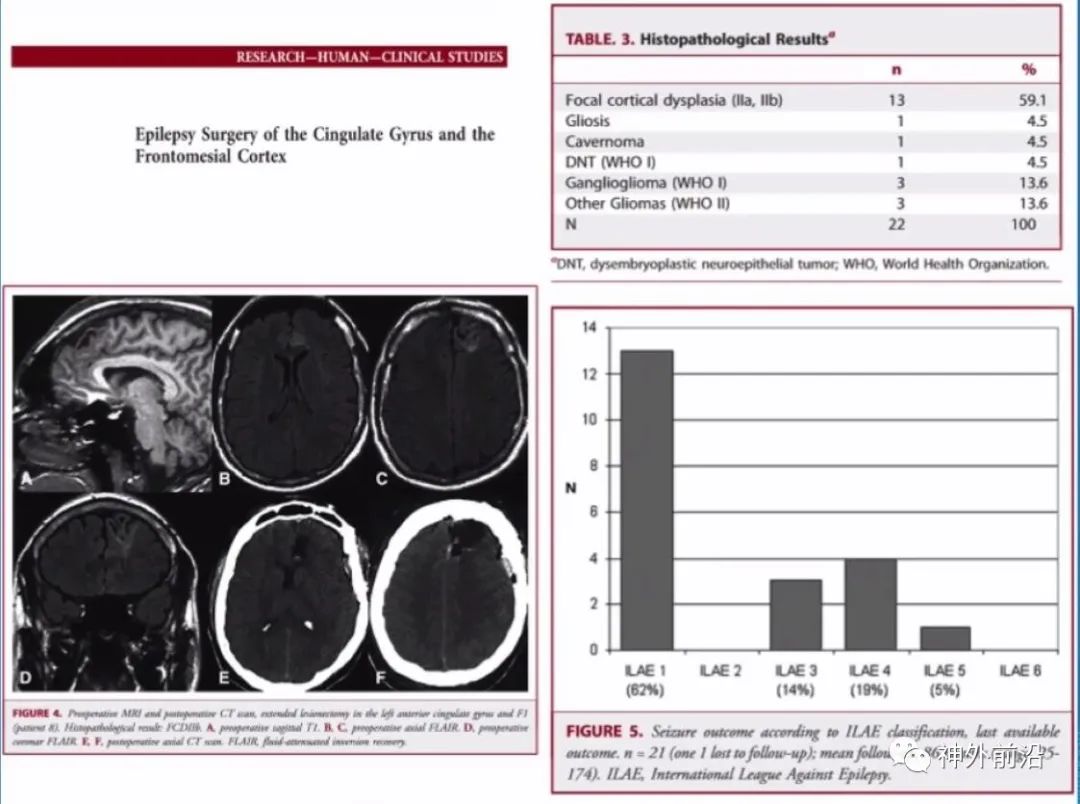
Reports on cingulate cortex epilepsy are not particularly numerous. This article reported on 22 cases, with the most common being FCD IIa and IIb. Gangliogliomas and other gliomas each had three cases, with one case of a cavernous angioma, and one case of DNT. Among the 22 cases, 21 showed focal abnormalities on MRI, with positive results, and the postoperative outcomes were also good, with approximately 62% achieving Engel I level, indicating a good effect.
Long-term follow-up showed that among the 20 cases, 13 achieved ILAE level I, with an overall effect of about 65%.
Additionally, a separate article on posterior cingulate cortex epilepsy reported on 7 cases, with 5 achieving Engel I level, including 4 at level Ia and 1 at level Ib, indicating good overall outcomes.
【Case A-5】
A 30-year-old male with negative MRI and PET results for cingulate cortex epilepsy, considering excessive movement, presented with bilateral discomfort in the head. Bilateral SEEG implantation was performed, but the origin was not particularly clear, relying entirely on high-frequency discharges, identifying the right anterior cingulate cortex, followed by extensive resection of the right medial frontal cortex, revealing cortical dysplasia post-surgery.
Reports of MRI-negative cingulate cortex epilepsy are quite rare. A 2012 article reported 19 cases, including two MRI-negative cases, indicating the scarcity of such reports.
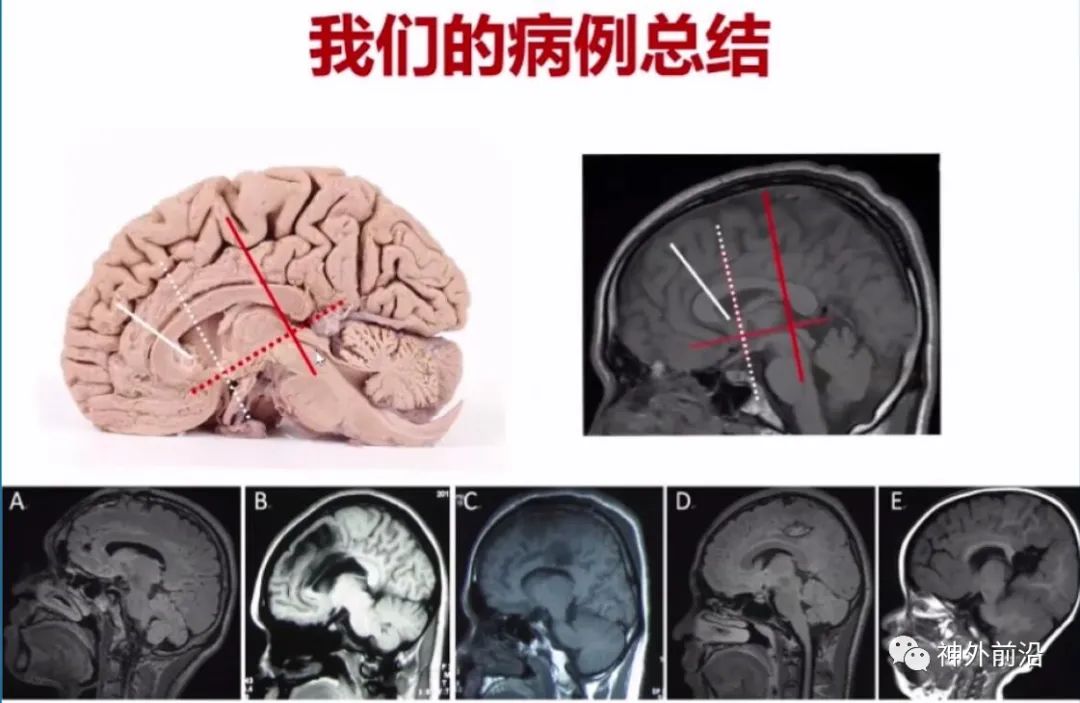
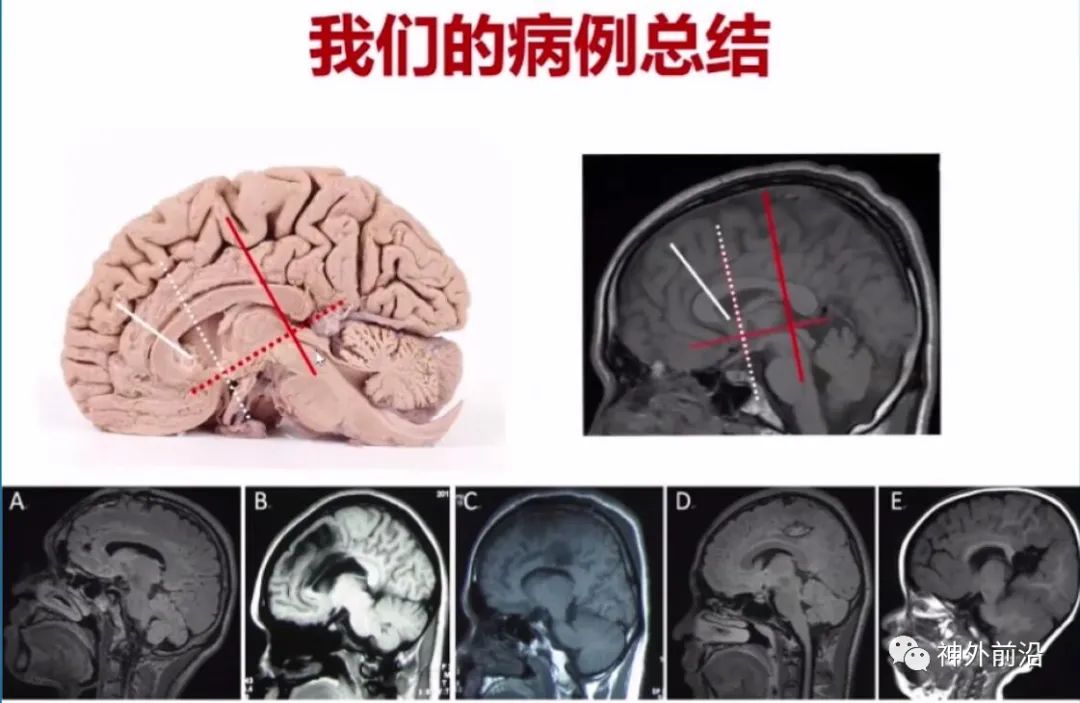
6. Summary of Our Cases
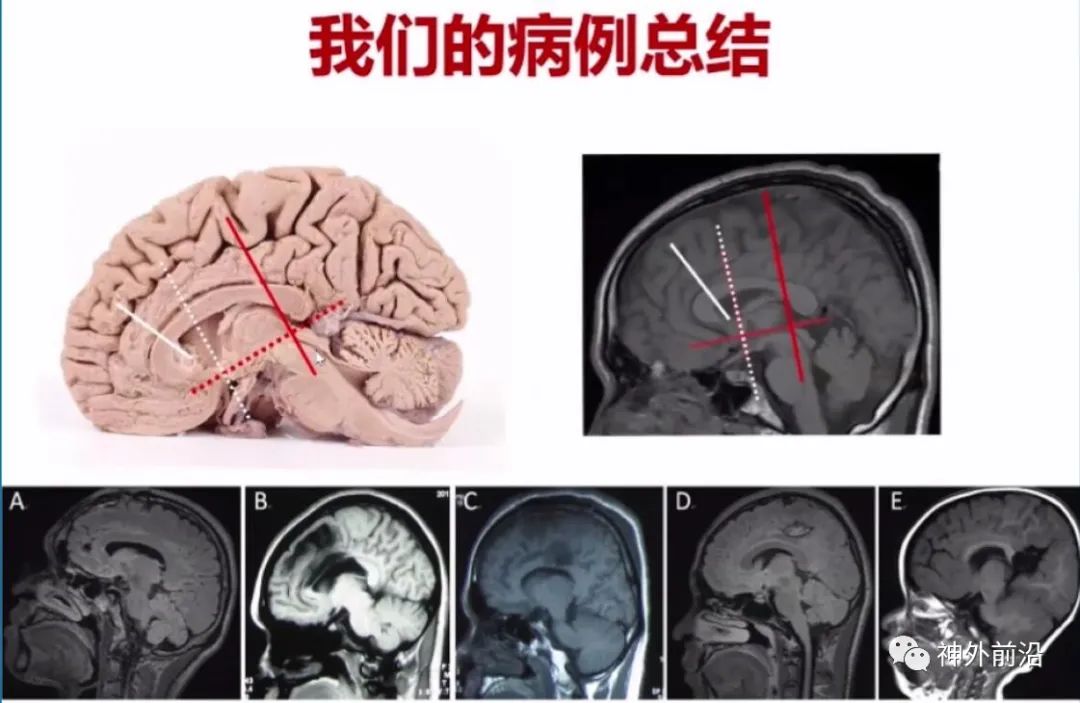
We have conducted morphological analyses of the cingulate cortex, with cases showing localized lesions, widespread lesions, and some extending beyond the cingulate cortex.
In 2019, Professor Zhang Kai’s group reported on 37 patients, with 12 cases of anterior cingulate cortex, 12 of middle cingulate cortex, and 16 of posterior cingulate cortex, with some spanning anterior-middle or middle-posterior cingulate cortex. Of the 12 anterior cingulate cases, 50% exhibited excessive movement symptoms, but GTCS was also common; middle cingulate cortex cases mainly presented with asymmetric tonic seizures, while posterior cingulate cortex cases mainly showed asymmetric tonic seizures and GTCS.
EEG results may have greater localization significance, especially ictal EEG being better than interictal EEG. Only 37.8% showed focal abnormalities within the cingulate cortex, while other abnormalities involving the cingulate cortex accounted for 54%. Most patients did not present with localized manifestations of the cingulate cortex; if lesions accumulate in the cingulate cortex, abnormalities are easier to detect on EEG, indicating that the localization value of EEG may relate to case selection.
Overall prognosis is good, with most being focal abnormal patients, indicating relatively good outcomes.
【Case】
A 19-year-old female patient with transient consciousness impairment and bilateral hand exploration for three years, is a case we handled early on. At that time, our understanding of FCD was not very clear, but MRI revealed cortical dysplasia in the posterior head. A localized lesion in the cingulate cortex was resected, revealing an oligodendroglioma, WHO grade II.
7. Summary of Cingulate Cortex Epilepsy and Surgical Treatment
The cingulate cortex can be divided into the anterior cingulate cortex (ACC), middle cingulate cortex (MCC), and posterior cingulate cortex (PCC);
It has extensive connections, and clinical symptoms are diverse, making scalp EEG localization challenging. In cases without lesions, intracranial electrode EEG localization is necessary;
The ACC is primarily associated with excessive movement and emotions, the MCC with cognition and movement, and the PCC mainly with temporal lobe epilepsy manifestations and complex subjective sensations.
Overall surgical prognosis is good; currently, good outcomes are typically achieved without lesions, and focal lesions do not necessarily require intracranial electrode EEG examinations.

Yang Anchao Associate Professor, Chief Physician of Functional Neurosurgery at Beijing Tiantan Hospital, Doctor of Medicine, Member of the Chinese Medical Association, Reviewer for “Chinese Journal of Neurosurgery (English Edition)”. Member of the Neurological Surgery Physician Committee of the Chinese Medical Association; Vice Group Leader of the Neuroregulation and Artificial Intelligence Group of the Neurorehabilitation Committee of the Chinese Medical Association; Member of the Neuronetwork Reconstruction Group of the Neurorehabilitation Committee of the Chinese Medical Association; Youth Member of the Chinese Anti-Epilepsy Association; Youth Member of the Parkinson’s Disease and Movement Disorders Committee of the Beijing Medical Association; Expert in Medical Device Technology Review; Member of the Expert Guidance Committee for the Demonstration Project of Neurosurgical Robot Applications; Secretary of the Chinese Neuroregulation Alliance.
Functional Neurosurgery Issue 27 | The Value of Brain Magnetometry in Determining the True Origin Side of Temporal Lobe Epilepsy – Sanbo Brain Hospital Zhou Jian Teng Pengfei
Xuanwu Hospital Yutao: Why is DBS Effective in Treating Refractory Epilepsy? Need to Study Cortical-Subcortical Networks | Functional Neurosurgery Issue 26
Functional Neurosurgery Issue 25 | Peking University First Hospital Cai Lixin: Preoperative Evaluation of Refractory Epilepsy in Children in the Posterior Head Area
Functional Neurosurgery Issue 24 | Anatomy, Electrophysiological Characteristics, and Surgical Applications of the Vim-DBS Target in Functional Neurological Diseases by Niu Chaoshi from the First Affiliated Hospital of the University of Science and Technology of China
Functional Neurosurgery Issue 23 | Liu Ruen from Peking University People’s Hospital: Comparative Study of Neuroregulatory Treatments for Meige Syndrome Targeting STN and GPI
Functional Neurosurgery Issue 22 | Yang Anchao from Tiantan Hospital: CM-Pf DBS Treatment for Tourette Syndrome
Functional Neurosurgery Issue 21 | Zheng Zhong from Beijing Fengtai Hospital: How to Achieve Target Visualization in ANT-DBS Treatment for Drug-Resistant Epilepsy
Functional Neurosurgery Issue 20 | How Effective is DBS in Awakening Vegetative Patients? – He Jianghong from Bayi Brain Hospital
Functional Neurosurgery Issue 19 | Hu Xiaowu from Changhai Hospital: The Relationship Between Levodopa Improvement Rate and DBS Efficacy in Parkinson’s Disease
Functional Neurosurgery Issue 18 | Wang Wei from West China Hospital: Neuroregulatory Treatment of Secondary Dystonia
Functional Neurosurgery Issue 17 | Ling Zhiping from 301 Hospital: Initial Exploration of 5G and DBS Applications – Remote Support for Surgical Planning and Intraoperative MER
Functional Neurosurgery Issue 16 | Wang Xuelian from Tangdu Hospital: Mechanism and Prospective Research of the Medial Forebrain Bundle in DBS Treatment of Mental Disorders
Functional Neurosurgery Issue 15 | Video Recording – Zhang Jianguo from Tiantan Hospital: Twenty Years of Deep Brain Stimulation for Epilepsy – Over 20,000 Surgeries Conducted in China
Functional Neurosurgery Issue 14 | Interview with Niu Chaoshi from the First Affiliated Hospital of the University of Science and Technology of China:Precise Positioning by Surgical Robots, Future Needs Further Intelligence
Functional Neurosurgery Issue 13 | Interview with Niu Chaoshi from the First Affiliated Hospital of the University of Science and Technology of China: How to Better Achieve the Transformation from Basic to Clinical under the Cross-Disciplinary Integration of Science, Engineering, and Medicine
Functional Neurosurgery Issue 12 | Yang Anchao from Tiantan Hospital: Robot-Assisted Resection of Epileptogenic Lesions (Part 2)
Functional Neurosurgery Issue 11 | Yang Anchao from Tiantan Hospital: Robot-Assisted Resection of Epileptogenic Lesions (Part 1)
Functional Neurosurgery Issue 10 | Interview with Zhang Jianguo from Tiantan Hospital: What Have We Discovered When the Total Number of Epilepsy VNS Surgeries in China Exceeds 3,000?
Functional Neurosurgery Issue 9 Interview | Zhang Jianguo from Tiantan Hospital Answers Hot Topics such as Functional Neurosurgery and Brain Science
[Review] 2017 Advances in Functional Neurosurgery and Brain Science – A Compilation of 230 Reports Categorized | Zhang Guojun, Zhang Jianguo Commentary
Cingulate Cortex Weekly

“Cingulate Cortex Weekly” is supported by Remebot, a leading medical robotics organization in China, co-written and produced by the Functional Neurosurgery Department of Beijing Tiantan Hospital and the Frontier Neurosurgery New Media, reporting the latest cutting-edge developments in the field, with Academic Editor Professor Zhang Jianguo welcoming contributions and support from industry experts; for reprints, please indicate the source and ensure the integrity of the article, contact email [email protected].