 (Long press to scan the QR code for more anesthesia knowledge points)
(Long press to scan the QR code for more anesthesia knowledge points)
Postoperative pain is one of the biggest concerns for patients. According to statistics, 20%-80% of patients experience moderate to severe pain after surgery, while traditional pain management methods—relying on physician experience and subjective patient descriptions—often have inaccuracies.
Today, we will introduce a technique for monitoring pain during surgery: the Surgical Pleth Index (SPI). How does it decode the “pain code” through non-invasive monitoring? What benefits can it bring to patients?

1. What is SPI?
1. Definition
SPI is a non-invasive monitoring tool based on Photoplethysmography (PPG) signals, which quantifies the objective indicators of intraoperative stress response and pain levels by monitoring the patient’s physiological parameters. It is commonly used to guide anesthesia depth and pain management. Its core principle is to reflect pain or stress states by analyzing the patient’s autonomic nervous system responses (such as heart rate and pulse waveform changes).
2. Calculation Principle of SPI
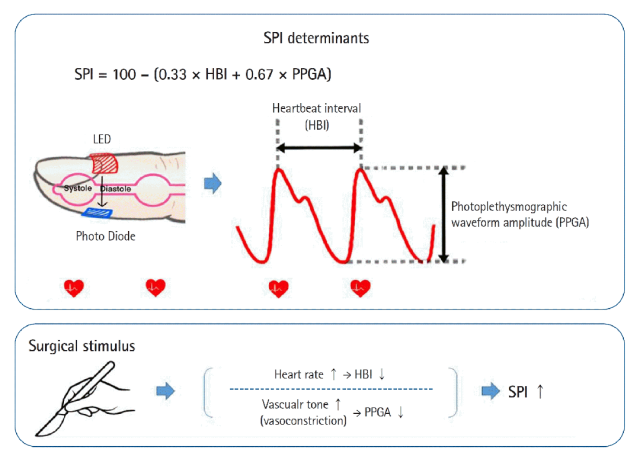
SPI is based on the integrated analysis of two physiological signals:
-
Heart Rate Variability (HRV): Reflects changes in the autonomic nervous system (especially sympathetic nervous activity); pain or stress can lead to sympathetic excitation and decreased heart rate variability.
-
Photoplethysmography (PPG): Pulse wave signals obtained through finger or earlobe sensors, whose amplitude and waveform characteristics (such as rise slope and peak interval) change due to vasoconstriction or vasodilation caused by pain.
The calculation model constructed based on the normalized heart beat interval (HBI) and standardized photoplethysmography pulse wave amplitude (PPGA):
SPI = 100 – (0.33×HBI + 0.67×PPGA)
3. Working Principle
When the body senses pain, sympathetic nervous excitation occurs → heart rate increases, blood vessels constrict → PPG signal fluctuations increase → SPI value rises.
SPI becomes an “electronic stethoscope for pain” by monitoring this physiological response in real-time.
2. Clinical Applications of SPI
1. Intraoperative Pain Monitoring
-
Target Range: Typically maintain SPI between 20-50, indicating adequate analgesia;
-
SPI > 50: Indicates insufficient analgesia, additional opioids (such as remifentanil) are needed;
-
SPI < 20: May indicate excessive analgesia or deep anesthesia.
2. Comparison with Traditional Subjective Scoring
-
SPI has a certain correlation with subjective pain scores (such as VAS, NRS), but is more suitable for patients who cannot report pain (such as during general anesthesia).
-
Studies show that SPI’s sensitivity to harmful stimuli such as skin incision and tracheal intubation can reach 80%-90%.
3. SPI vs Other Pain Monitoring Tools: Who is Superior?
| Tool | Principle | Advantages | Limitations |
|---|---|---|---|
| SPI | PPG signal analysis | Non-invasive, real-time, low cost | Affected by age, drugs, and position |
| Analgesia Nociception Index (ANI) | Heart rate variability analysis | Sensitive to bleeding | Easily interfered with by vasoactive drugs |
| Pupil Measurement Method | Monitoring dynamic changes in pupil | High sensitivity | Complex operation, high cost |
| Nociception Level (NOL) | Multi-parameter comprehensive assessment (PPG, GSR, etc.) | Wide applicability | Requires calibration, validity and reliability need verification |
Conclusion: SPI is the most cost-effective option in most cases, especially suitable for general surgical procedures; complex cases may use it in conjunction with other tools.
4. Limitations of SPI
1. Interfering Factors:
-
Hypovolemia, hypothermia, and vasoactive drugs (such as epinephrine) may affect the accuracy of PPG signals;
-
Data reliability decreases in patients with arrhythmias (such as atrial fibrillation) or peripheral vascular diseases.
2. Individual Differences:
-
Different patients have significant physiological response differences to pain, requiring clinical judgment;
-
In elderly or diabetic patients, autonomic nervous function may decline, potentially reducing SPI sensitivity.
3. Cannot Replace Subjective Assessment:
-
Postoperative awake patients still need to combine VAS/NRS scores for comprehensive pain assessment.
In summary, SPI provides a non-invasive, continuous method for intraoperative pain monitoring by integrating heart rate and pulse waveform changes, but its interpretation must consider individual patient conditions and clinical scenarios.
 Previous Recommendations:Application of Surgical Pleth Index (SPI) in Pain Monitoring
Previous Recommendations:Application of Surgical Pleth Index (SPI) in Pain Monitoring END
END

▼ Click “Read Original“ to experience smart healthcare at your fingertips!!