Eye Twitching
“Eye twitching” usually refers to minor eyelid spasms related to fatigue, stress, or caffeine, which typically last from a few seconds to a few minutes before resolving on their own. This symptom is also known as eyelid tremor, characterized by repetitive, involuntary contractions of the eyelid muscles, often occurring in the upper eyelid.
Eye twitching (Image Source: SpongeBob SquarePants)
Blepharospasm
Blepharospasm (BSP) is a focal, segmental dystonia characterized by excessive activity of the orbicularis oculi and other muscles around the eyes, leading to involuntary closure of the eyelids.
It typically affects both sides and progresses over time, most commonly occurring in women aged 50-70, with most cases being sporadic.

Idiopathic BSP (Image Source: BBC News)
Based on the etiology, it is divided into primary and secondary types. Primary eyelid spasms are more common and are also known as benign essential blepharospasm (BEB). Secondary eyelid spasms are often associated with facial spasms, Tourette syndrome, Parkinson’s disease, brain tumors, cerebrovascular diseases, entropion, blepharitis, and keratoconjunctivitis.

The pathogenesis primarily involves compression at the intracranial segment of the facial nerve and the intersection with blood vessels, leading to abnormal discharges of the facial nerve due to vascular pulsations (Image Source: Peak Eye Clinic)
Clinical Manifestations
Initially, it may present as intermittent and persistent minor eyelid twitching, increased blinking, or involuntary eyelid closure, potentially accompanied by frowning, narrowing of the palpebral fissure, drooping of the upper eyelid, and eyelid laxity. In later stages, persistent eyelid spasms can lead to difficulties in seeing, even functional blindness. Symptoms typically worsen in bright light or during stress, and improve during calmness or after sleep. In some patients, specific actions such as speaking, singing, opening the mouth, chewing, or touching the cheeks can alleviate the symptoms, known as “sensory tricks.” Additionally, non-motor symptoms such as psychiatric disorders, sleep disturbances, sensory abnormalities, and eye discomfort may also accompany.
Compared to other focal dystonias, BSP is more likely to spread to adjacent areas, with more than half of patients developing other dystonias within five years of onset, commonly seen as oromandibular dystonia (OMD) and Meige syndrome (also known as idiopathic blepharospasm-oromandibular dystonia syndrome).
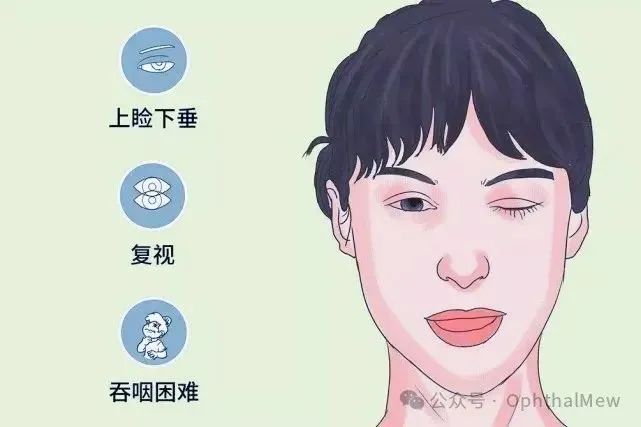
Meige syndrome primarily manifests as involuntary spasms of the oral and facial muscles. Common symptoms include lip movements and jaw muscle contractions, accompanied by dry mouth and difficulty swallowing. Spasms of the facial muscles can also lead to facial twitches and involuntary movements (Image Source: West China Neurology)
Diagnosis and Differential Diagnosis
Primary BSP lacks unified diagnostic criteria and can be preliminarily diagnosed based on the typical synchronous contraction pattern of the bilateral orbicularis oculi, sensory tricks phenomenon, and increased blinking.
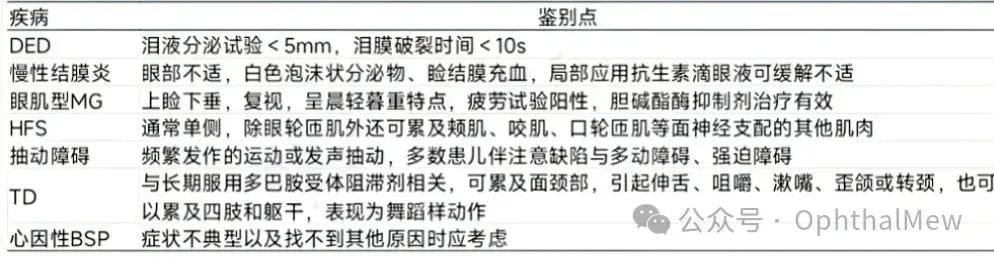
When BSP symptoms are atypical or in the early stages, it should be differentiated from dry eye syndrome (DED), chronic conjunctivitis, myasthenia gravis (MG), hemifacial spasm (HFS), tic disorders, tardive dyskinesia (TD), and psychogenic BSP.
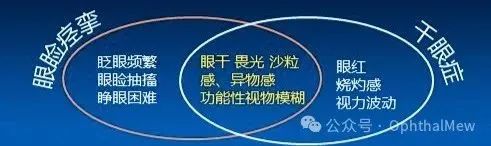
Eyelid spasms vs dry eye syndrome
(Source: Professor Gong Lan: “Beauty Secrets” Botulinum Toxin Transforms into “Eye Treatment”)
Treatment
For mild eyelid spasms, rest, avoiding light (wearing UV-blocking glasses, such as photochromic glasses), applying warm compresses, and avoiding caffeine and prolonged screen use can be effective.
Psychotherapy may be necessary if required.
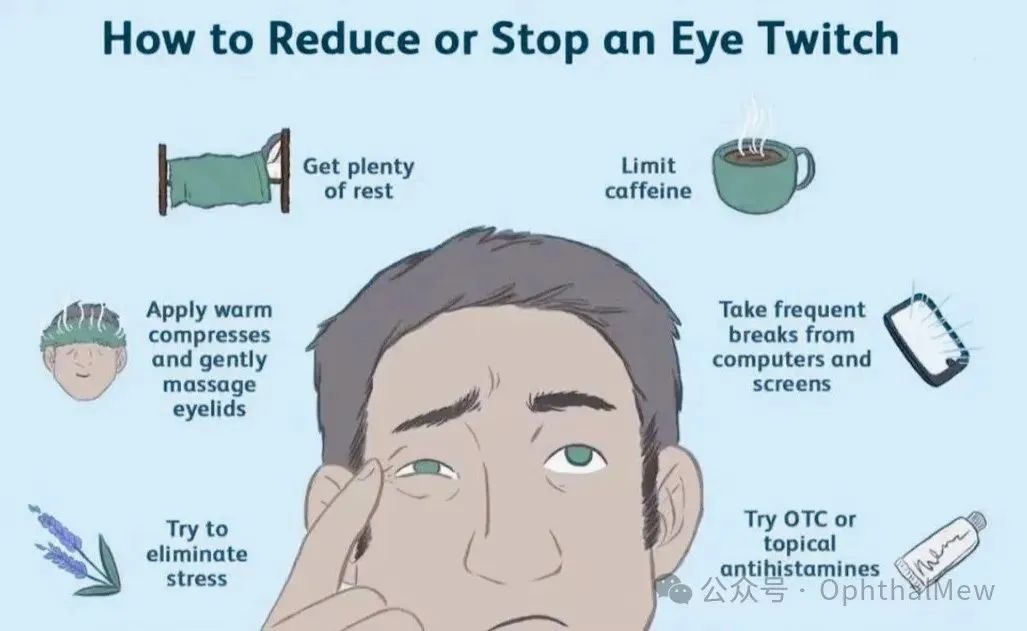
How to Stop Eye Twitching (Image Source: Verywell Health)
Botulinum toxin type A (BTX-A) injection is the first-line treatment for focal dystonias and is also applicable for BSP. Botulinum toxin selectively acts on peripheral cholinergic neuron terminals, inhibiting the release of acetylcholine, causing temporary paralysis of the muscles at the injection site. The average onset time of BTX-A is 2-7 days, with effects lasting 3-4 months, and 90% of patients experience moderate improvement. It is important to note that most patients require repeat injections to maintain efficacy.

Application of Botulinum Toxin in Ophthalmology (Source: Professor Gong Lan: “Beauty Secrets” Botulinum Toxin Transforms into “Eye Treatment”)
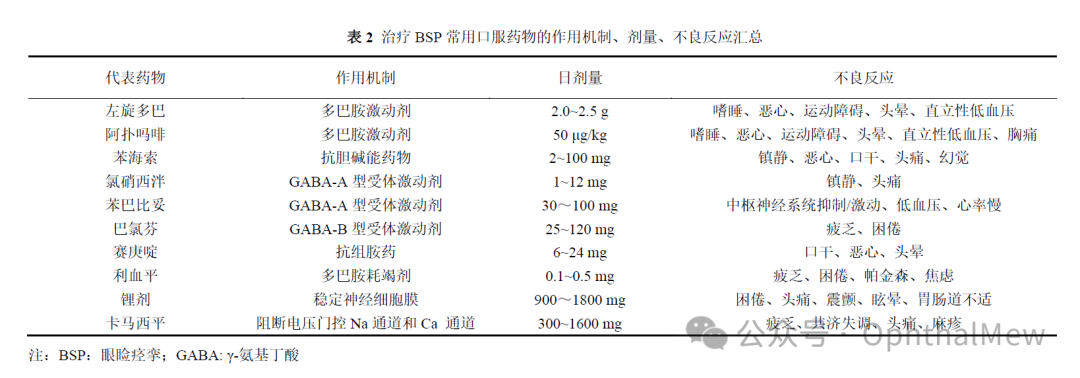
The efficacy of oral medications is uncertain, and drug-related side effects limit their clinical use.
For patients unresponsive to oral medications and BTX injections, eyelid muscle resection may be considered.
Repetitive transcranial magnetic stimulation (rTMS) is a technique that achieves therapeutic effects by modulating cortical and subcortical networks related to clinical symptoms. Deep brain stimulation (DBS) may be used for refractory dystonias that do not respond well to oral medications or BTX-A treatment. The internal globus pallidus (GPi) and subthalamic nucleus (STN) are classic targets for treating dystonias. However, both methods require large-scale clinical studies for further validation.
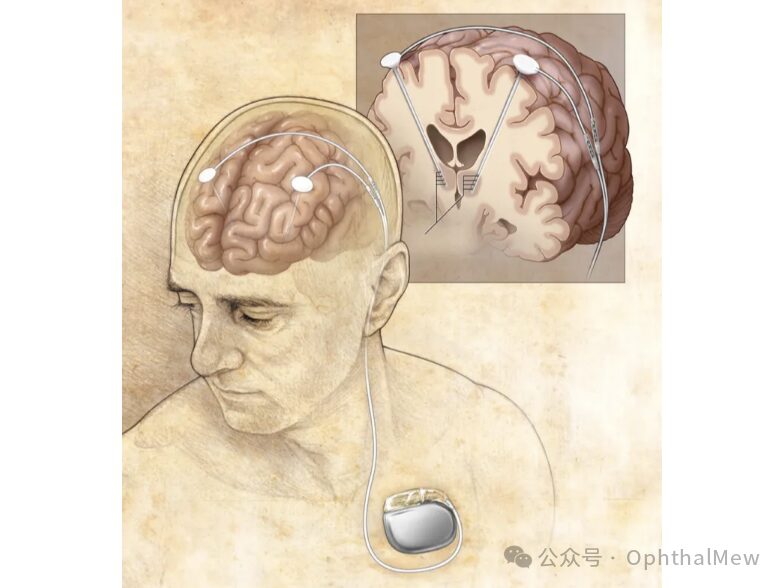
DBS treatment (Image Source: Mayo Foundation for Medical Education and Research)
References:
[1] Wang Xixi, Wan Xin. Research Progress on Blepharospasm [J]. Journal of Chinese Neuroimmunology and Neurology, 2022, 29(5).
[2] Gong Lan, Lin Tong. Blepharospasm [M]. People’s Health Publishing House. Shanghai.
[3] Expert Consensus on the Diagnosis and Treatment of Meige Syndrome in China (2018) [J]. Chinese Journal of Ophthalmology, 2018, 54(02): 93-96.
Source: OphthalMew

Disclaimer: This article is for academic exchange among medical and health professionals only and does not represent the views of this platform. This information cannot replace professional medical guidance in any way and should not be considered as treatment advice. If this information is used for purposes other than information, this platform and the author do not assume any related responsibilities.