
Effective postoperative wound management is crucial for preventing potential complications such as surgical site infections (SSI) and wound dehiscence (SWD). Key principles of postoperative wound management include timely wound assessment, appropriate wound cleansing and dressing use, and early recognition and active treatment of wound complications.
Appropriate postoperative surgical wound care is vital for preventing potential complications such as SSI, SWD, and hematoma. Healthcare professionals must understand the principles of postoperative wound management to minimize the occurrence of wound complications.
Wound Healing Phases
Regardless of the mechanism of injury, classical wound healing can be divided into three phases: inflammatory phase, proliferative phase, and remodeling phase.
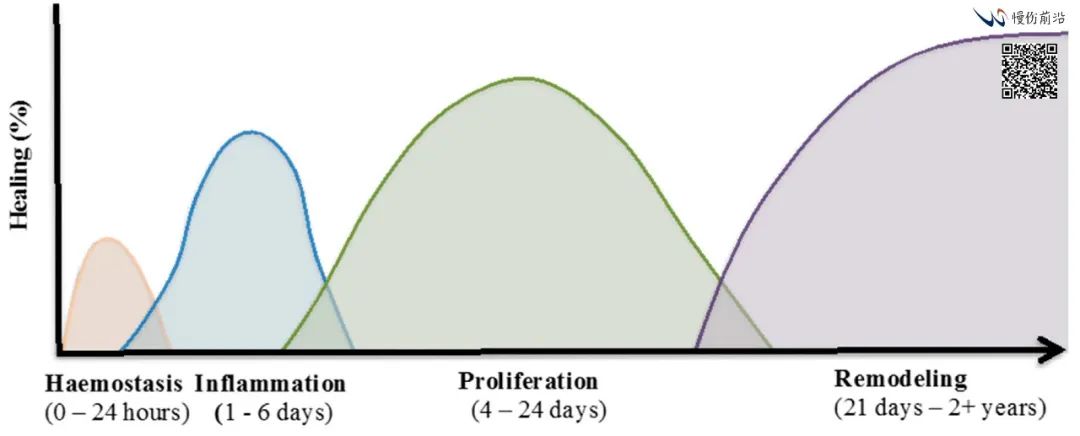
The inflammatory phase is the body’s natural response to injury, occurring immediately after wound formation. The injury triggers the release of local inflammatory mediators, causing vasodilation. Increased local blood flow brings phagocytic white blood cells, such as neutrophils and macrophages, to the wound site, playing a crucial role in phagocytosing bacteria and breaking down necrotic tissue. The body’s response to injury is characterized by typical inflammatory signs: redness, heat, swelling, pain, and limited function.
During the proliferative phase, the wound begins to rebuild. Granulation tissue, composed of collagen and extracellular matrix, fills the wound defect, while angiogenesis occurs. As the wound defect is filled, the wound gradually contracts, and epithelial tissue begins to form at the wound edges. Eventually, after the epithelialization process is complete, new epithelial cells fully cover the wound.
The final stage of wound healing is remodeling, which begins after the wound is closed. During this phase, the tensile strength of the wound is restored as collagen fibers in the wound are reorganized and rearranged. Additionally, during this phase, the wound undergoes de-vascularization, returning to its original blood supply status.
Types of Wound Healing
There are mainly two types of wound healing: primary intention healing and secondary intention healing. Most surgical wounds close by primary intention, with minimal tissue loss and well-approximated wound edges. Wounds healing by primary intention have a rapid epithelialization rate and minimal scarring.
Wounds healing by secondary intention are left intentionally open due to potential infection or unsatisfactory approximation of wound edges. Secondary intention healing involves the processes of granulation tissue proliferation, wound contraction, and re-epithelialization. Wounds healing by secondary intention often result in larger scars.
Postoperative Wound Care
Principles
Regardless of the mechanism of wound healing, the goal of postoperative wound care is the same: to allow the wound to heal quickly without complications, achieving optimal function and aesthetic outcomes.
The edges of primary intention wounds should be properly aligned. In the early stages of healing, the tensile strength of the wound is very low because collagen fiber reorganization has not yet begun. Therefore, external support, including sutures, staples, or tape, is needed until complete reorganization and epithelialization occur.
Keep the Wound Clean
The wound should be kept as clean as possible to prevent the occurrence of SSIs. The UK’s NICE provides recommendations for postoperative wound management to reduce the incidence of SSIs (Table 1). These recommendations include dressing use and wound cleansing, antibiotic therapy and debridement, as well as information on specialized wound care.
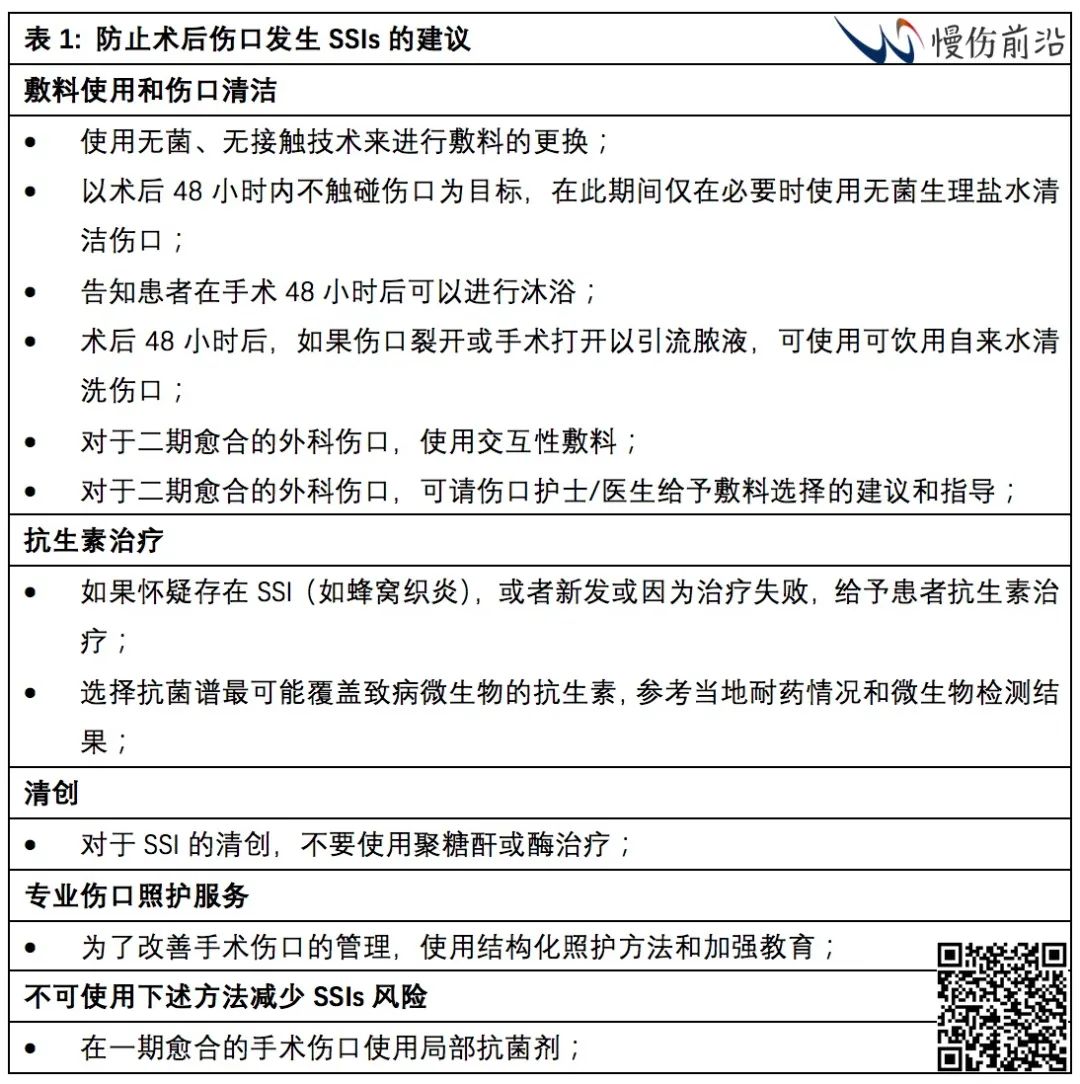
Occasionally, the wound may need to be washed to remove debris, such as necrotic tissue or excessive exudate, to avoid delaying wound healing. In these cases, gentle irrigation of the wound with a syringe and warm saline or water should be performed to minimize trauma to the wound and maintain a good healing environment. Remember, washing itself can also be a disruption to wound healing, and excessive washing may delay the healing process.
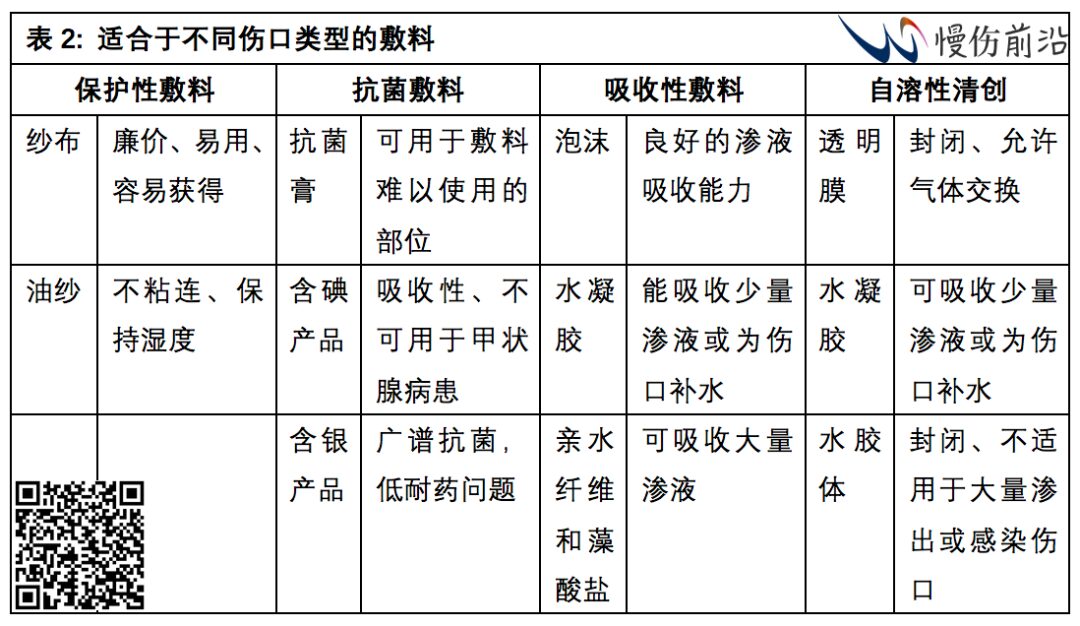
Dressing
Dressing is an important tool in postoperative wound management. A good dressing should maintain a moist wound environment and promote wound healing, remove excess exudate (excessive exudate can lead to maceration), provide a good barrier against bacterial or fluid contamination, have good adherence, and be non-traumatic upon changing. As every wound is different, the choice of dressing should meet the individual needs of each wound. Factors to consider when deciding on dressing selection should include wound location, size, depth, and level of exudate. Table 2 provides general recommendations for dressing selection. Dressings used during surgery should be maintained in a sterile environment for the period required by the surgical team. It is acceptable to open dressings early to inspect the wound; in some cases, a new dressing can be changed. These situations include when the dressing is no longer fulfilling its purpose (e.g., falling off, excessive exudate saturating the dressing and leading to a poor healing environment) or when there is suspicion of wound complications.
Possible Complications
Two common complications of surgical wounds are infection (SSI) and wound dehiscence (SWD). Therefore, careful observation is necessary to identify postoperative wounds that exhibit the following signs: fever, hematoma, seroma, wound edge separation, and purulent discharge. Remember that inflammation of surgical wounds is a physiological component of healing; if there are no other clinical signs of infection, it does not equate to wound complications.
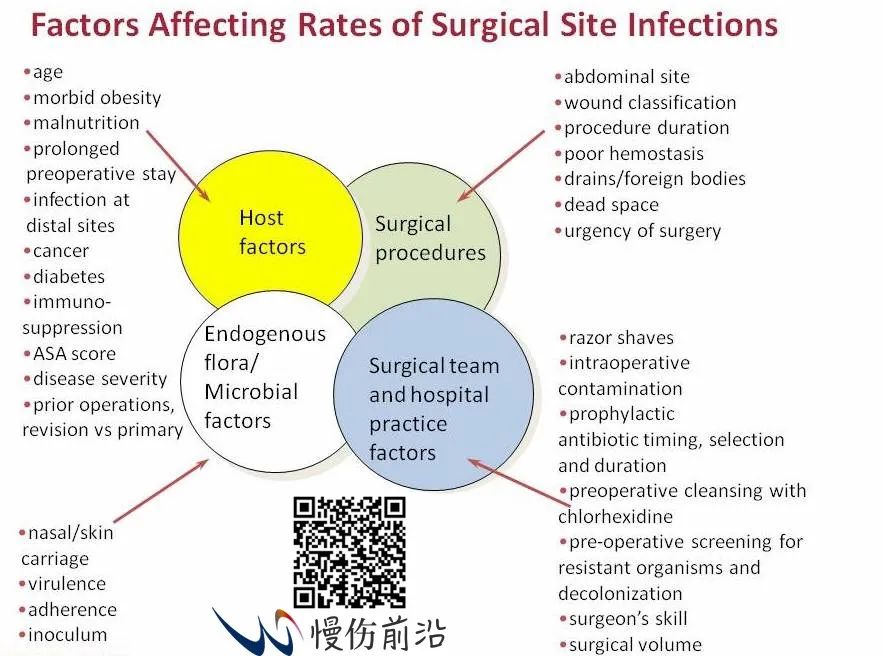
Factors affecting the occurrence of SSI: patient factors, type of surgery, endogenous flora/microorganisms, and practice factors.
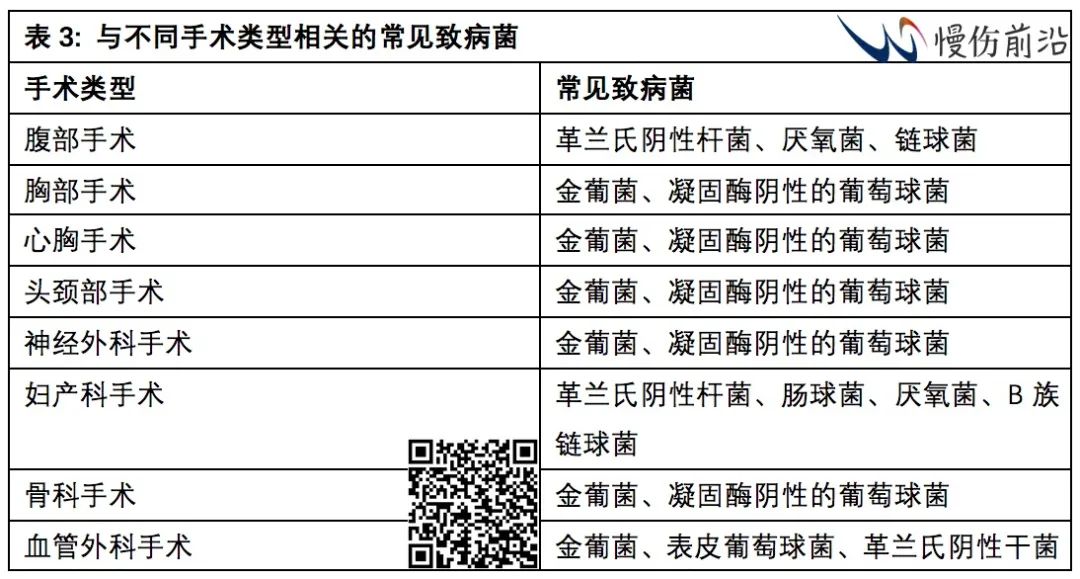
If a wound infection is suspected, active treatment should be considered. First, perform wound swab cultures and sensitivity tests. Secondly, empirical antibiotic therapy can be initiated based on suspected pathogens (Table 3). Targeted treatment should follow after the pathogen is confirmed. Debridement of necrotic and infected tissue is another effective method for treatment and preventing further spread. For wounds with unclear presentations, immediate antibiotic treatment is not necessary, but close and regular monitoring of the progression of signs and symptoms is essential.

Superficial dehiscence can be closed secondarily after necrotic tissue is removed and can be reinforced with dressing. Debridement and primary closure are suitable for small dehiscences, while continuous tension devices and NPWT are appropriate for larger and deeper dehisced wounds. However, professional advice should be sought if there are any doubts at any stage.
Certain patient factors may increase the risk of postoperative wound complications, including type of surgery, duration of surgery, body site, certain medications, immunosuppressive diseases, poorly controlled diabetes, peripheral vascular disease, smoking, malnutrition, radiotherapy, obesity, etc. Immunosuppressants, such as prednisone and methotrexate, and immunosuppressive diseases can inhibit the inflammatory process and delay wound healing. Poorly controlled diabetes can hinder the initial inflammatory response, while hyperglycemic states can reduce neutrophil and macrophage function, thereby delaying the wound healing process. For patients with peripheral vascular disease, tissue oxygenation levels are compromised. Similarly, smoking can cause arterial spasms, affecting oxygen supply. Malnutrition can slow metabolic processes, affecting collagen synthesis. Therefore, careful control of these factors is necessary to prevent the occurrence of wound complications.
Effective management of surgical wounds is a crucial component of postoperative recovery. Healthcare professionals should closely monitor the acute wound healing process, prevent wound complications, and provide appropriate treatment for any complications that arise. Key elements of postoperative wound management include timely wound inspections, appropriate cleansing and dressing use, and early recognition and intervention of wound complications.
