
☞ Different reflective signals of normal retinal tissue in OCT:
1. The nerve fiber layer and the retinal pigment epithelium exhibit high reflectivity.
2. The plexiform layer and nuclear layer show moderate reflectivity.
3. Photoreceptor cells have low reflectivity.
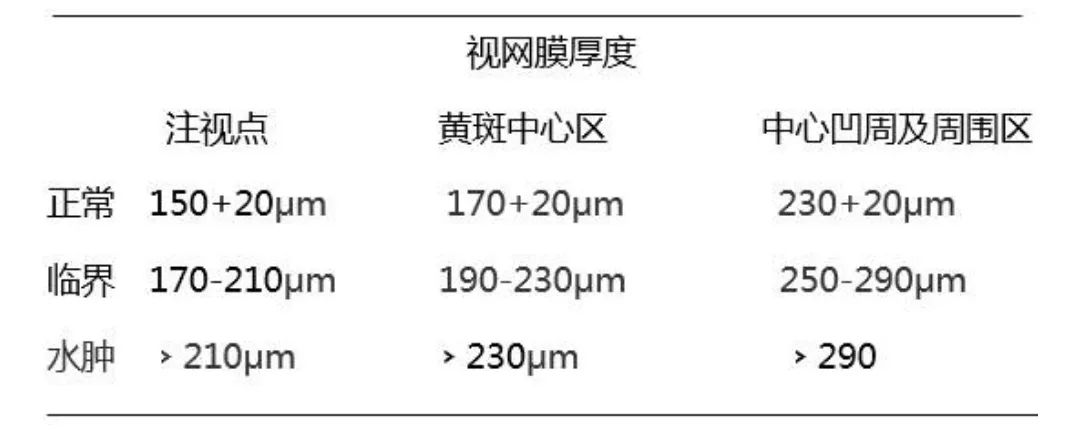
☞ Normal retinal thickness:
1. The distance from the vitreoretinal interface to the anterior surface of the retinal pigment epithelium is approximately 200μm to 275μm.
2. The depression of the fovea is about 170μm to 190μm.
3. The peripheral retinal thickness is generally about 220μm to 280μm.
☞ Retinal thickness in DME
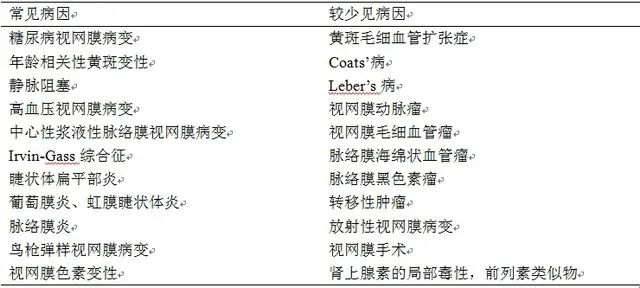
☞ Common causes of macular edema (ME):
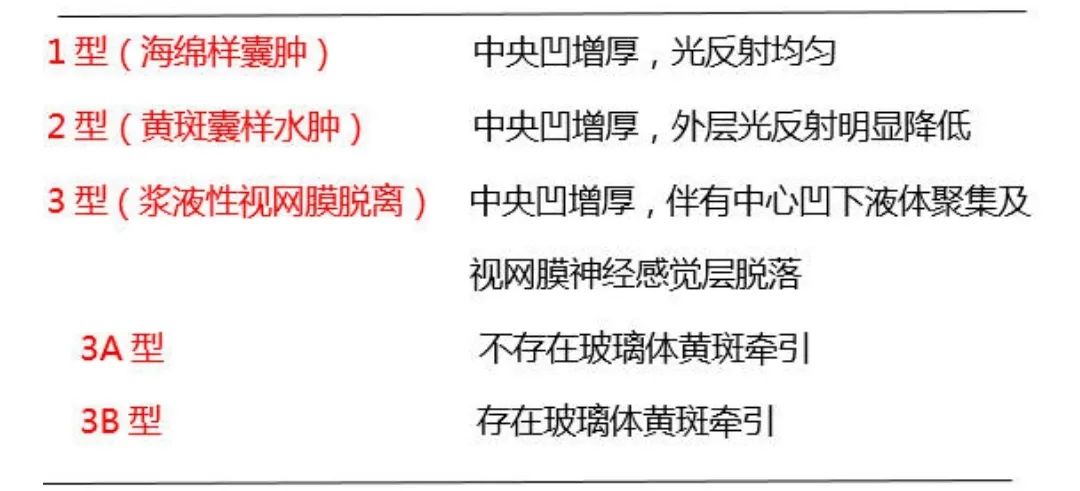
☞ OCT shows three structural changes in diabetic macular edema (DME):
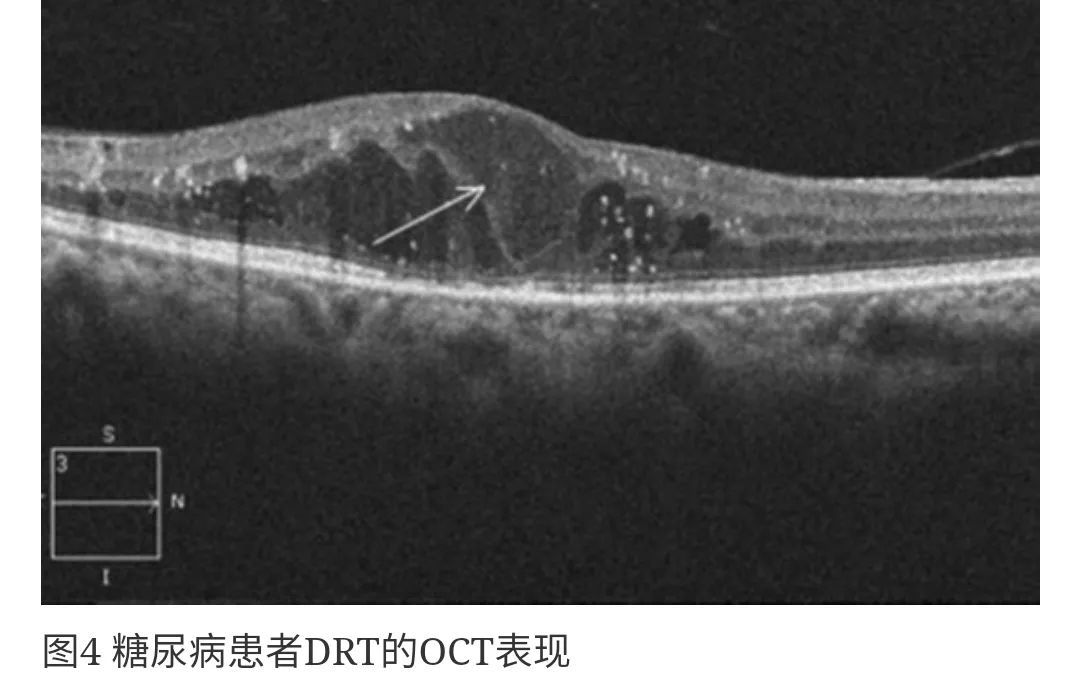
1. Diffuse retinal thickening (DRT) 97% — Localized or diffuse edema initially presents as a decrease in inter-retinal reflective signals, an increase in retinal thickness, and a spongy appearance of the retina (Figure 4).
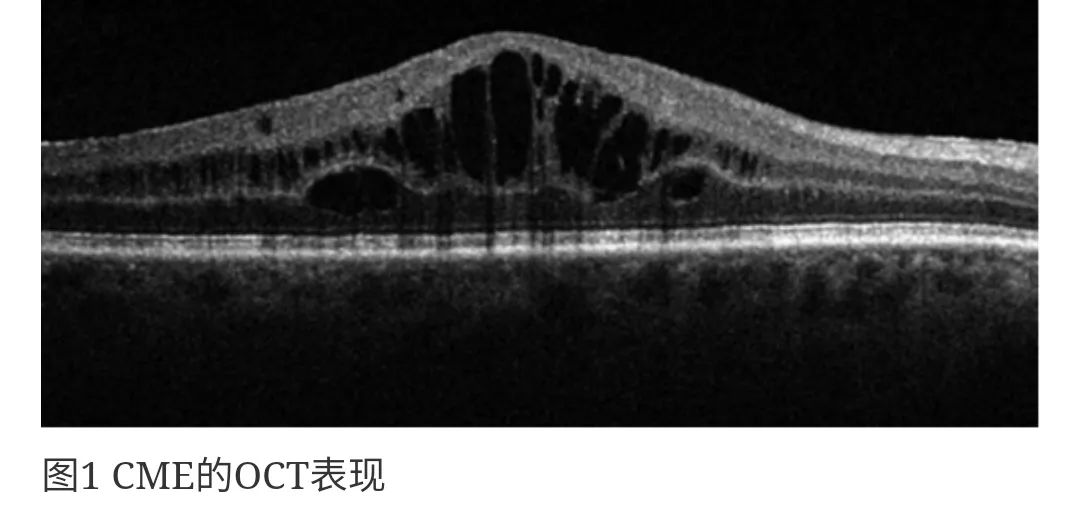
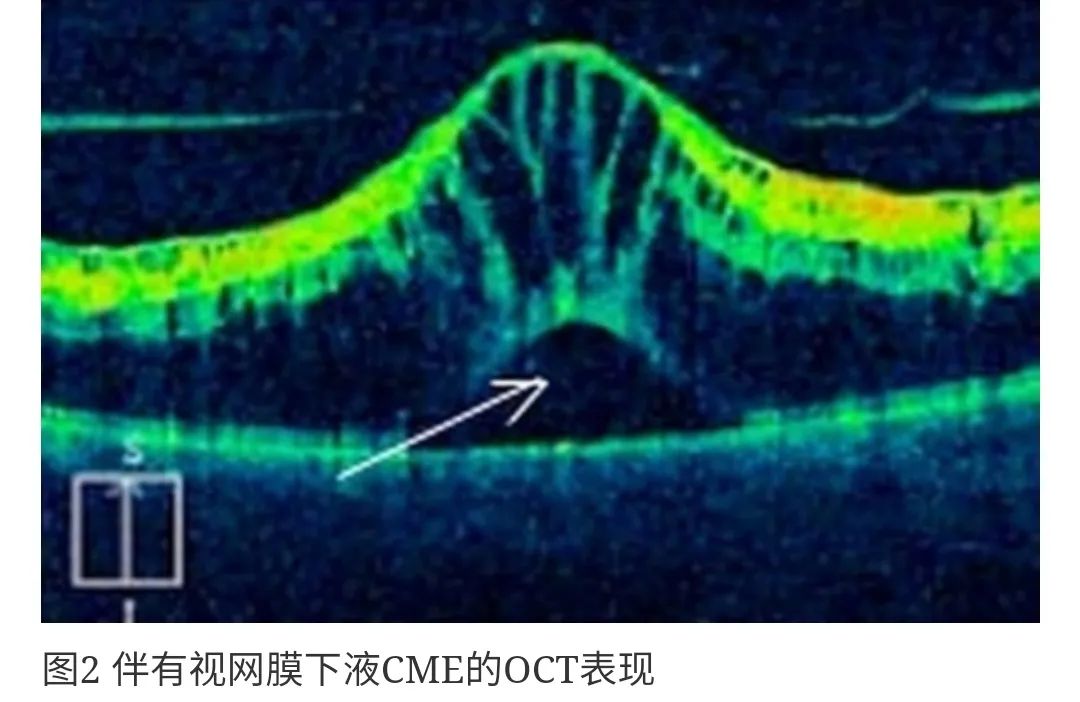
2. Cystoid macular edema (CME) 55% — Fluid accumulates in a limited space within the retinal layers, forming cystic structures in the outer plexiform layer, characterized by high reflective intervals and low reflective cystic cavities, resulting in a rose-like appearance in late fluorescein angiography. The arrangement of CME cavities mainly depends on the vertical Müller fibers (Figures 1 and 2).
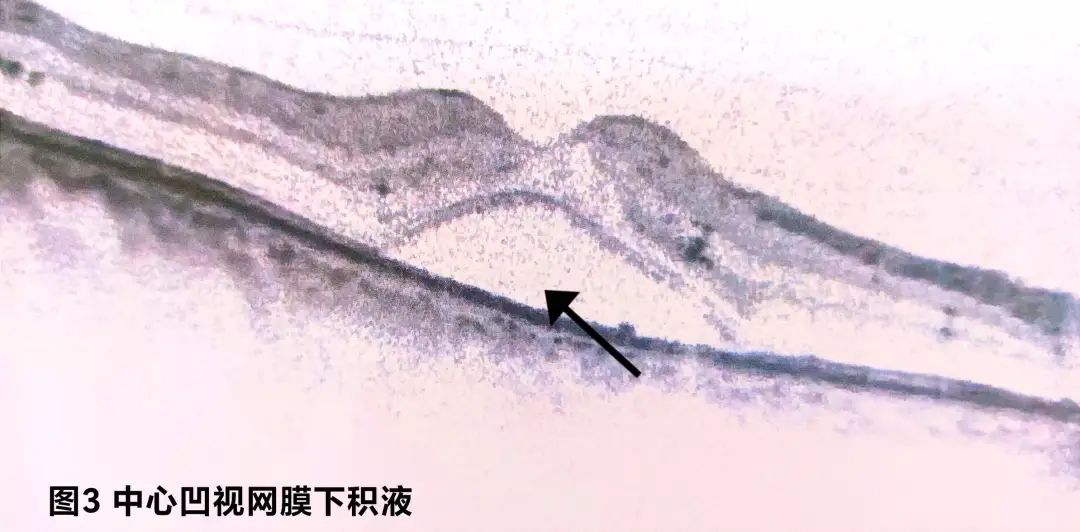
3. Serous retinal detachment (SRD) 7% — Often caused by chronic edema, presenting as a dome-shaped high reflective detachment of the retina with subretinal fluid appearing black (Figure 3). SRD is classified into two subtypes based on the presence or absence of retinal traction.
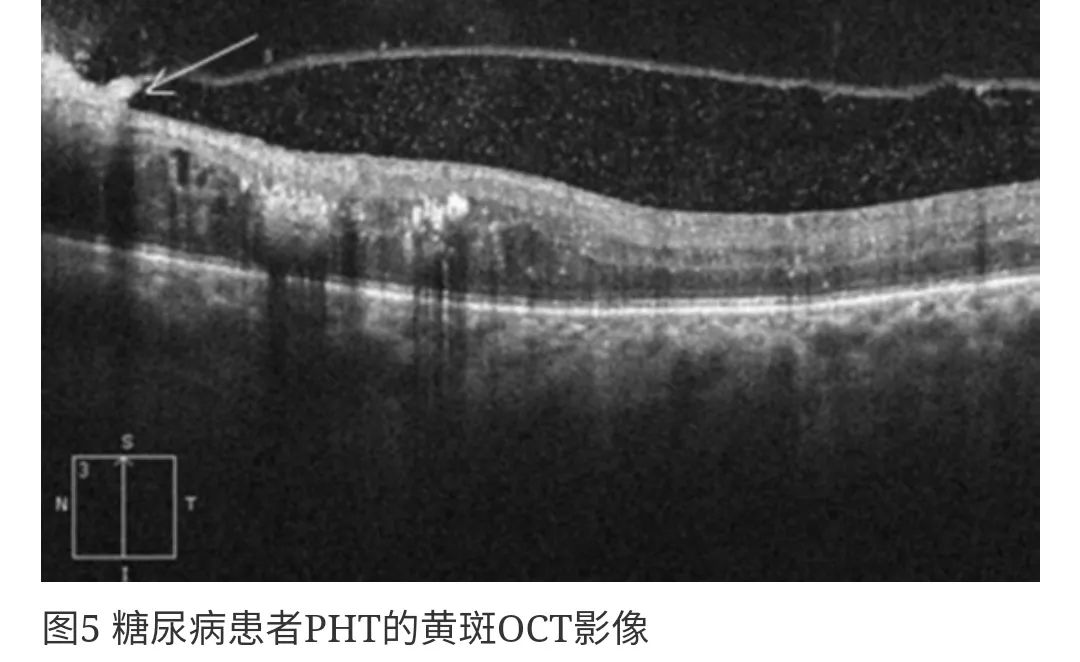
3A. Posterior vitreous traction (PHT) without tractional retinal detachment (TRD) 12.7%
3B. Posterior vitreous traction (PHT) with tractional retinal detachment (TRD) 2.9% — TRD presents as a low reflective signal area beneath the high reflective external surface of the detached retina, often appearing as a peak (Figure 5).
Research indicates: There is a correlation between retinal thickness and visual acuity in DME patients.
For every 100μm increase in retinal thickness, visual acuity (logMAR) decreases by 0.16. The OCT type with the worst visual acuity is CME, where the presence of CME results in a decrease of 0.40, while other types result in a decrease of 0.16.
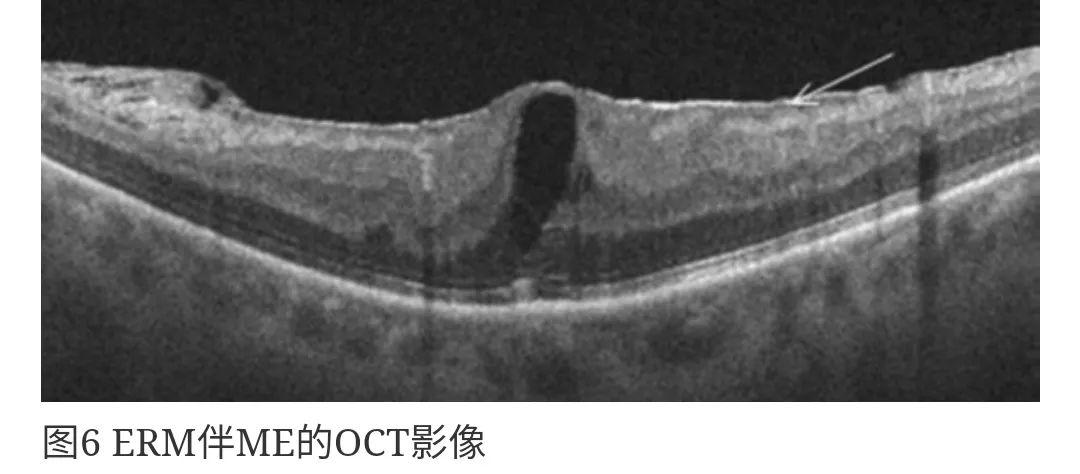
☞ Epiretinal membrane (ERM)
Characterized by a fibrous cell membrane on the inner surface of the retina that is avascular (Figure 6), also known as glassy membrane retinal disease, often caused by idiopathic or secondary proliferative changes at the vitreoretinal interface.
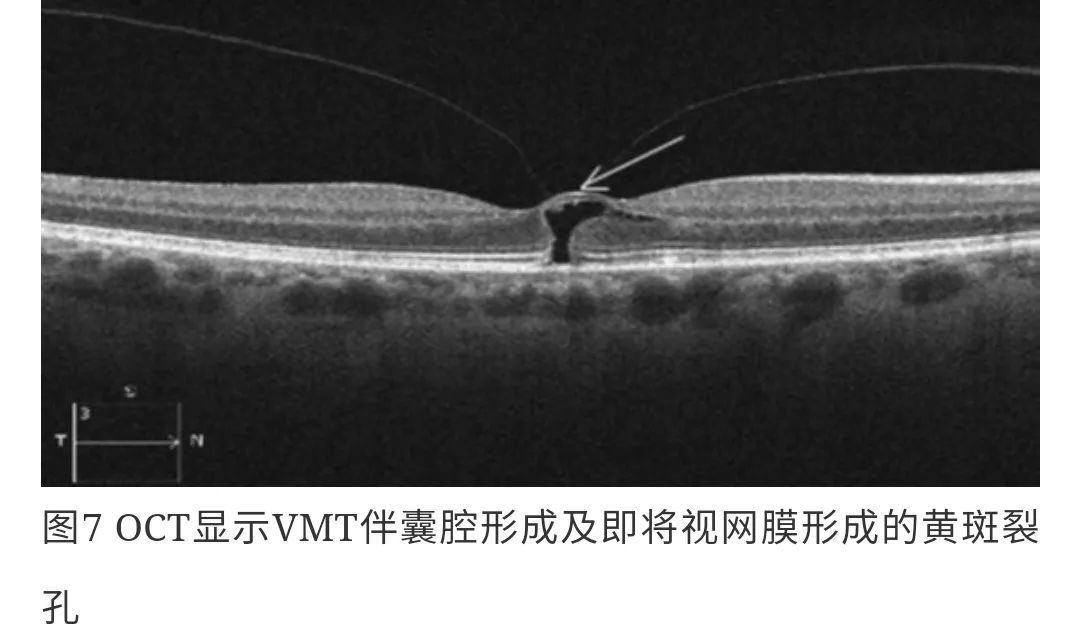
☞ Vitreomacular traction (VMT)
Characterized by partial incomplete PVD, residual adherent vitreous pulling on the retina in the macular region (Figure 7). The adherent vitreous cortex surrounds the macular area and optic nerve, being relatively wide and often dumbbell-shaped, which can lead to cystoid thickening of the macula.
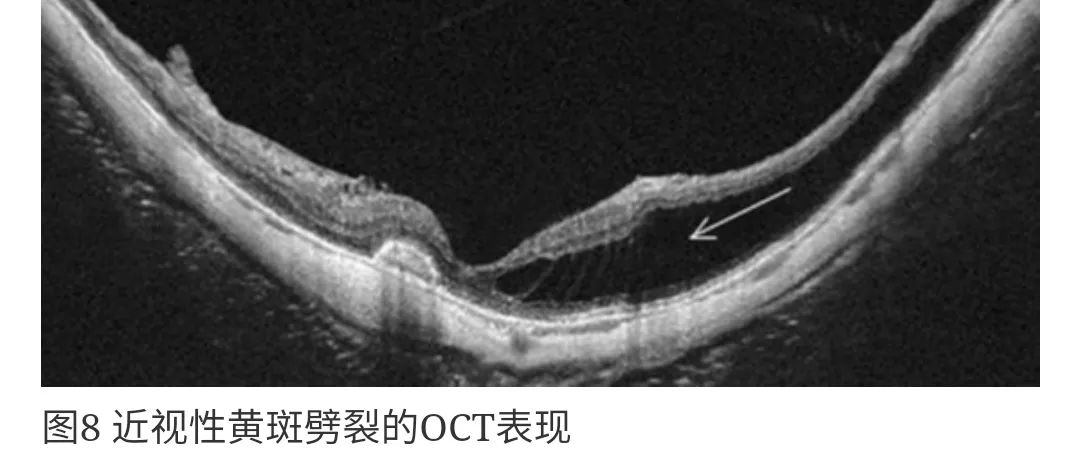
☞ Retinal tear
Commonly seen in high myopia and posterior scleral staphyloma (Figure 8), diagnosis can be challenging with the naked eye, but OCT can assist in diagnosis.
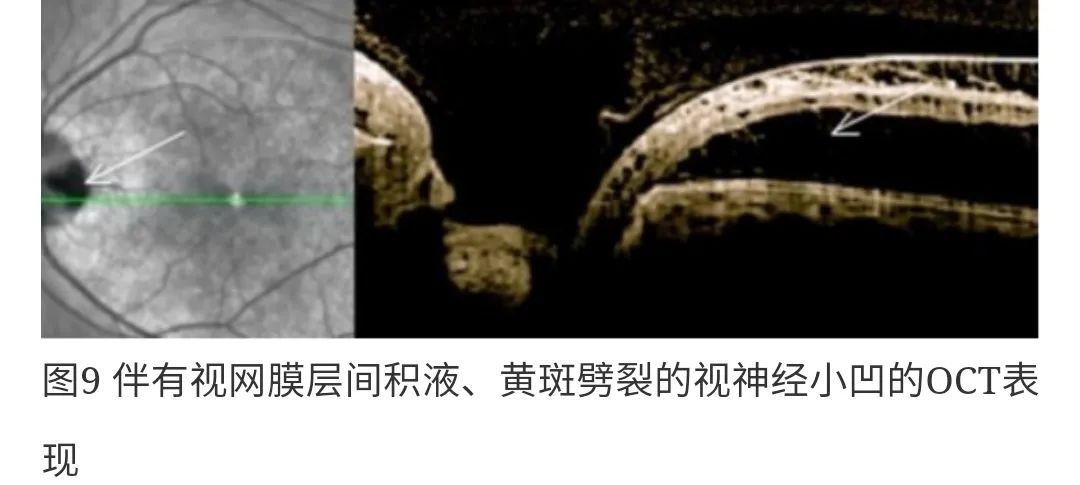
☞ Optic nerve cupping and macular tearing due to defects
OCT helps to identify ME caused by optic disc cupping or defects, as well as the characteristics of tearing (Figure 9). In these cases, inter-retinal fluid accumulation and tear-like cyst formation can be observed.
OCT has become one of the effective means for detecting, assessing, and treating in our clinical practice, achieving qualitative and quantitative assessment of retinal thickness for the first time, and correlating it with visual acuity. In summary, this non-invasive imaging technique plays a crucial role in accurately assessing macular edema and guiding treatment.
