Author: Professor Tao Rong, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine
The anatomical structure of the mitral valve includes leaflets, annulus, chordae tendineae, and papillary muscles. Its normal opening and closing play a crucial role in maintaining left ventricular systolic and diastolic function. Any structural or functional abnormalities in any part can lead to mitral regurgitation. Patients with mild regurgitation may experience slight exertional dyspnea, while severe regurgitation can exacerbate heart failure and even lead to cardiogenic shock.
Mitral regurgitation is mainly classified into primary and secondary lesions, with secondary referring to atrial or ventricular diseases caused by myocardial ischemia or dilated cardiomyopathy. Among these, regurgitation due to left ventricular dilation is termed functional mitral regurgitation (FMR), which is commonly seen in heart failure patients.
With the advancement of interventional treatment techniques, an increasing number of patients with mitral regurgitation can benefit from improvements. However, there is still controversy regarding whether surgical treatment can effectively improve survival rates in patients with mitral regurgitation secondary to severe left ventricular dysfunction. At the same time, with the rise of interventional treatments and improvements in techniques, some high-risk surgical patients can also benefit. Therefore, for patients with heart failure combined with FMR, is medical therapy alone sufficient, or is interventional treatment necessary? The following discussion will focus on the application value of interventional treatment methods in this patient population.
Treatment Strategies for Functional Mitral Regurgitation
The 2017 ESC guidelines updated the intervention indications for secondary mitral regurgitation, including: ① For patients with severe mitral regurgitation, ejection fraction >30%, and persistent symptoms despite optimized medical therapy (including indicated CRT implantation), surgical intervention may be considered (IIb, C); ② For patients with severe mitral regurgitation without indications for revascularization or with high surgical risk, if LVEF >30% and echocardiographic assessment shows good valve morphology, interventional treatment may be performed (IIb, C); ③ If LVEF ≤30%, the patient’s condition should be assessed to determine whether to proceed with surgical or interventional treatment (IIb, C).
It is evident that for patients without indications for revascularization and with high surgical risk, especially those with severe heart failure, interventional treatment has its unique clinical therapeutic value.
Effectiveness of Interventional Treatment for Mitral Regurgitation
Transcatheter mitral valve repair (MitraClip) is currently the most common interventional technique for treating mitral regurgitation. This procedure is usually performed in conjunction with annulus plasty, where the Clip device is delivered to the left atrium via transseptal puncture to grasp the anterior and posterior leaflets of the mitral valve. The EVEREST II study established its feasibility and safety, and subsequent analyses confirmed that patients successfully treated with MitraClip showed significant improvement in regurgitation, with low rates of recurrence and reoperation.
The ACCESS-EU registry study was the first clinical observational cohort study to evaluate the treatment value of MitraClip in patients with FMR, enrolling 567 individuals. The results showed that the 30-day and 1-year mortality rates were 2.8% and 17%, respectively, with 91.6% of patients achieving MR ≤ +2 at discharge, and 78.5% maintaining efficacy at 1 year. Additionally, the 1-year six-minute walk distance of patients also increased. The multicenter SENTINEL study also focused on secondary MR patients, demonstrating the effectiveness of MitraClip treatment.
Although the above results demonstrate the treatment value of MitraClip in FMR patients, most studies are observational, and there has been a lack of higher-level clinical trial evidence until the publication of the COAPT study results.
The COAPT study was a randomized controlled clinical trial aimed at assessing the application value of MitraClip in patients with heart failure combined with FMR. The study included 78 centers across the United States and Canada, enrolling 614 patients with moderate to severe FMR. Patients were randomly assigned to the MitraClip group (surgical group) and the medical therapy group (control group) on the basis of receiving maximum dose optimized medical therapy, with the primary efficacy endpoint being heart failure hospitalization within 24 months, and the primary safety endpoint being device-related complications within 12 months.
After 24 months of follow-up, the annual heart failure hospitalization rate in the surgical group was 35.8%, while the control group was 67.9% (HR: 0.53, 95% CI: 0.40-0.70, P < 0.001); in the surgical group, the all-cause mortality rate within 24 months also decreased from 46.1% in the control group to 29.1% (HR: 0.62, 95% CI: 0.46-0.82, P < 0.001). Meanwhile, the incidence of device-related complications within 12 months post-operation was only 3.4%. (Figure 1)
Figure 1
Primary efficacy endpoints, safety endpoints, and all-cause mortality.
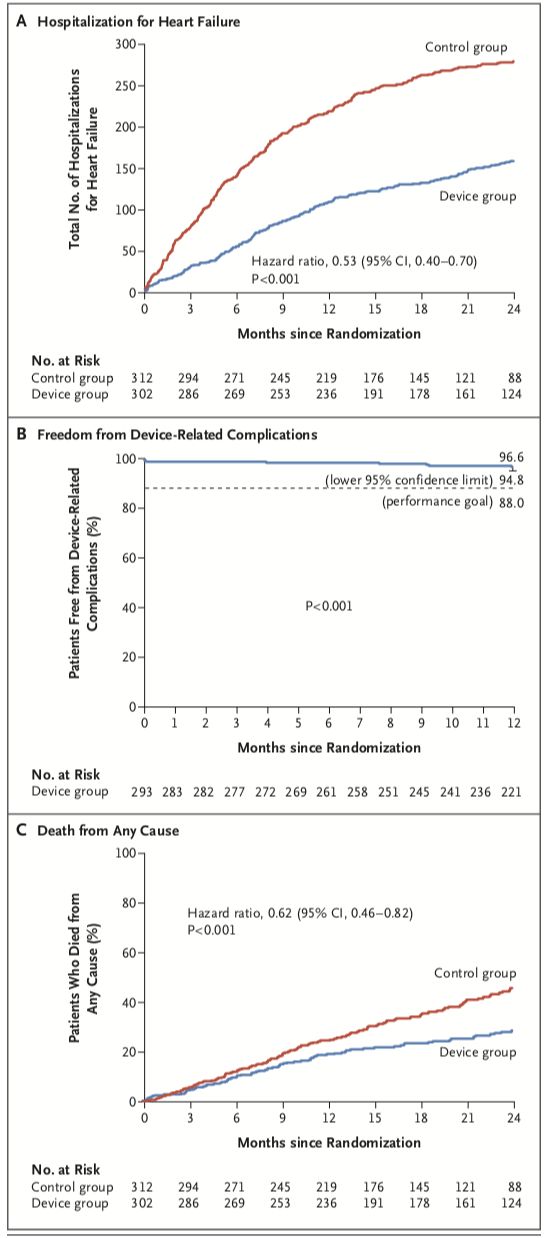
It can be seen that for patients with heart failure combined with moderate to severe functional mitral regurgitation, adopting interventional mitral valve repair methods on the basis of optimized medical therapy can significantly reduce all-cause mortality and heart failure readmission rates compared to medical therapy alone.
The latest analysis of the EVEREST II study recently published clarified the impact of MitraClip on the degree of mitral regurgitation, cardiac size, and cardiac function levels in FMR patients, stratifying patients by surgical risk. The results showed that both high-risk and low-risk surgical patients had a significant reduction in postoperative left ventricular end-diastolic volume, with a 1-year survival rate exceeding 70%, and the vast majority of patients maintained MR ≤ 2+ and NYHA I/II levels, reducing heart failure readmissions.
In addition to MitraClip, other repair methods for leaflets and chordae tendineae include NeoChord, Mitra-Spacer, MitraSpan, etc., which are currently in clinical research stages, and their clinical value, especially in FMR patients, remains to be clarified.
It is worth mentioning the recent publication of multicenter clinical study results based on the Cardioband system. The Cardioband system is a direct annulus plasty technique that can perform mitral valve annulus plasty via catheter to reduce the regurgitation area. This study enrolled 60 patients with moderate to severe MR, undergoing interventional surgery on the basis of optimized medical therapy. The 1-year survival rate was 87%, with a heart failure readmission rate of 66% and a reintervention rate of 78%. At the same time, the degree of mitral regurgitation in patients decreased postoperatively, and improvements were observed in cardiac function levels, quality of life scores, and six-minute walk tests.
Additionally, there is left ventricular remodeling technology, known as the Coapsys annulus plasty system, which was specifically designed for FMR and is often performed concurrently with surgical procedures. This system places two small pads on the left ventricular surface and uses polyethylene lines embedded at the level of the left ventricular papillary muscles, gradually tightening the lines under ultrasound guidance to shorten the distance of the left ventricular wall below the mitral valve, thereby achieving closure of the mitral valve. In the RESTORE-MV phase I clinical study, 19 patients underwent off-pump bypass and Coapsys mitral plasty, showing significant improvement in regurgitation levels postoperatively. Valve replacement options include CardiAQ stent, Tiara system, etc. Although their application prospects are promising, their role in functional mitral regurgitation remains unclear, and various methods are still in the research process.
Outlook
Transcatheter mitral valve repair is still in the development stage, and with research progress and device improvements, it may become an important treatment option for patients with mitral regurgitation, especially those at high surgical risk. Heart failure patients with moderate to severe FMR have shown benefits from MitraClip and Cardioband direct annulus plasty, which can partially reverse left ventricular remodeling and improve patient symptoms, holding significant clinical value. However, regarding various interventional treatment methods, there is still a need for more randomized controlled clinical trials to provide evidence-based medical evidence; on the other hand, safer and more effective treatment measures are continuously being developed and improved, including clinical studies based on the MitralStitch (minimally invasive mitral valve repair system via the apical route) that are being conducted at Fuwai Hospital in China. It is believed that in the future, more heart failure patients with functional mitral regurgitation will benefit from interventional surgical treatment to improve their prognosis based on ideal medical therapy.
Physician Profile
 Professor Tao RongDepartment of Cardiology, Ruijin Hospital, Shanghai Jiao Tong University School of MedicineChief Physician, Doctoral SupervisorHead of the Heart Failure Subspecialty at Ruijin Hospital. Engaged in clinical diagnosis and treatment and basic research of heart failure for a long time. From May 2005 to February 2008, he was a visiting scholar at the University of California, San Francisco (UCSF) Cardiology Department. Currently serves as a member of the Heart Failure Committee of the Chinese Medical Doctor Association, a member of the Women’s Health Group of the Cardiovascular Disease Branch of the Chinese Medical Association, a standing committee member of the Precision Medicine Committee of Cardiovascular Disease of the Chinese Society of Geriatrics, and a member of the Heart Failure Group of the Shanghai Medical Association. He has published more than 20 SCI articles as the first/corresponding author in Circulation, Cardiovasc Res, etc., and has hosted three general projects of the National Natural Science Foundation of China and one major basic research project of the Shanghai Science and Technology Commission. He has been selected for the Shanghai Science and Technology Commission Pujiang Talent Program and the first Peak Plateau Discipline Construction Program of the Shanghai Municipal Education Commission.
Professor Tao RongDepartment of Cardiology, Ruijin Hospital, Shanghai Jiao Tong University School of MedicineChief Physician, Doctoral SupervisorHead of the Heart Failure Subspecialty at Ruijin Hospital. Engaged in clinical diagnosis and treatment and basic research of heart failure for a long time. From May 2005 to February 2008, he was a visiting scholar at the University of California, San Francisco (UCSF) Cardiology Department. Currently serves as a member of the Heart Failure Committee of the Chinese Medical Doctor Association, a member of the Women’s Health Group of the Cardiovascular Disease Branch of the Chinese Medical Association, a standing committee member of the Precision Medicine Committee of Cardiovascular Disease of the Chinese Society of Geriatrics, and a member of the Heart Failure Group of the Shanghai Medical Association. He has published more than 20 SCI articles as the first/corresponding author in Circulation, Cardiovasc Res, etc., and has hosted three general projects of the National Natural Science Foundation of China and one major basic research project of the Shanghai Science and Technology Commission. He has been selected for the Shanghai Science and Technology Commission Pujiang Talent Program and the first Peak Plateau Discipline Construction Program of the Shanghai Municipal Education Commission.
The content of this article is original content from the “Outpatient” magazine. Reproduction requires authorization and please indicate the source.
New Horizons in Outpatient Care |WeChat ID: ClinicMZ

Official WeChat of “Outpatient” magazine
Long press, scan the QR code, and follow us