Wan Xue Mei, Yang Jun. Clinical Study on Retention Time and Recurrence After Tympanostomy in Children with Secretory Otitis Media. Journal of Clinical Otorhinolaryngology Head and Neck Surgery, 2017, 31(7): 500-503, 509.
Secretory otitis media (SOM) is commonly seen in preschool children, with an incidence of about 90%, and is a leading cause of hearing loss in children. Tympanostomy is the most common and effective surgery for treating pediatric SOM. In the United States, about 6.8% of children under three years old have undergone tympanostomy, and some patients require multiple insertions due to recurrent SOM. The duration of tympanostomy tube placement significantly impacts the recurrence rate of SOM and postoperative complications, yet optimal tube retention duration is rarely reported in literature. This study followed up on children who underwent tympanostomy for SOM, comparing the clinical characteristics of those who experienced recurrence and required re-insertion with those who recovered after their first insertion, analyzing factors influencing SOM recurrence and the need for re-insertion, providing clinical evidence to reduce recurrence and lower the risk of re-insertion.
1. Clinical Data
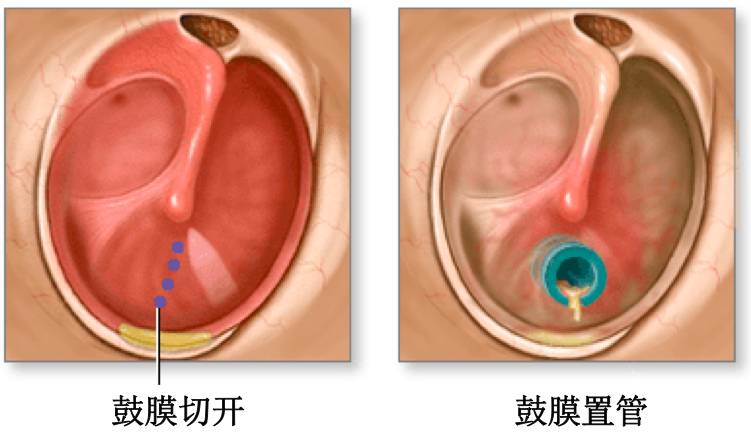
From June 2011 to December 2012, 465 children diagnosed with SOM and admitted for tympanostomy at Xinhua Hospital affiliated with Shanghai Jiao Tong University were followed up, with 331 cases included. All SOM patients underwent tympanostomy, with surgical indications following the 2004 American clinical guidelines for secretory otitis media. Regarding the choice of tympanostomy tubes, our department initially used a 1.14mm diameter button tube due to its small incision and self-falling advantage. For re-insertion after recurrence, a longer retention T-tube was selected. Adenoidectomy was performed simultaneously during the first tympanostomy.
2. Methods
Data collected included gender, age at surgery, preoperative history, surgical plan, etc., through outpatient visits and phone follow-ups. Follow-up contents included: ① calculation of tympanostomy tube retention time by reviewing outpatient medical records; ② symptoms during retention such as ear pain, purulent discharge, tinnitus, and whether there were any residual tympanic membrane perforations after tube removal; ③ recurrence after tube removal, triggering factors, recurrence frequency, and whether re-insertion was needed; ④ history of allergic rhinitis (AR) in children. Statistical analyses were performed on the distribution of gender, age at insertion, and retention time, as well as the relationship between retention time, gender, age, and SOM recurrence rate, and the correlation between AR incidence and SOM recurrence rate. All patients were regularly followed up postoperatively, once every three months, and if the tube had not fallen out after 7 to 18 months, it was removed in the outpatient department.
3. Statistical Methods
SPSS 19.0 software was used for analysis, with t-tests and χ2 tests employed to compare differences between groups. A p-value <0.05 was considered statistically significant.
1. Basic Follow-Up Conditions
Among 465 cases, 331 were followed up (total of 576 ears), including 220 males (66.47%), with 57 cases being unilateral and 163 bilateral; 111 females (33.53%), with 31 unilateral and 80 bilateral.
2. Tube Removal and Self-Removal
Patients in this group had their tubes removed in the outpatient department or self-removed before March 2014. Those with a retention time of 1-6 months all self-removed, while those with a retention time greater than 7 months included both self-removal and outpatient removal, with 63 ears (10.94%) requiring removal.
3. Age of Children at First Tympanostomy and Age at Recurrence
The average age of children undergoing the first tympanostomy was (4.69±2.18) years, with males averaging (4.76±2.25) years and females averaging (4.55±2.04) years. Comparisons of average ages between males and the overall average showed t=0.456, p>0.05; similarly, comparisons of females showed t=-0.726, p>0.05.
Among 331 children, 104 experienced recurrence after tube removal, resulting in a recurrence rate of 31.21%, with parents reporting upper respiratory infections as triggering factors. The recurrence rate varied with age; follow-up data indicated that most recurrent cases were concentrated in children aged 3-6 at the time of first insertion, totaling 97 recurrent cases, accounting for 93.27% of all recurrent cases.
4. Relationship Between Recurrence Rate and Gender After Tube Removal
Among 220 male children, 73 experienced recurrence after tube removal, giving a recurrence rate of 33.18%. Among 111 female children, 31 experienced recurrence, resulting in a rate of 27.93%. Chi-square test analysis showed no statistically significant difference in recurrence rates between males and females (p>0.05).
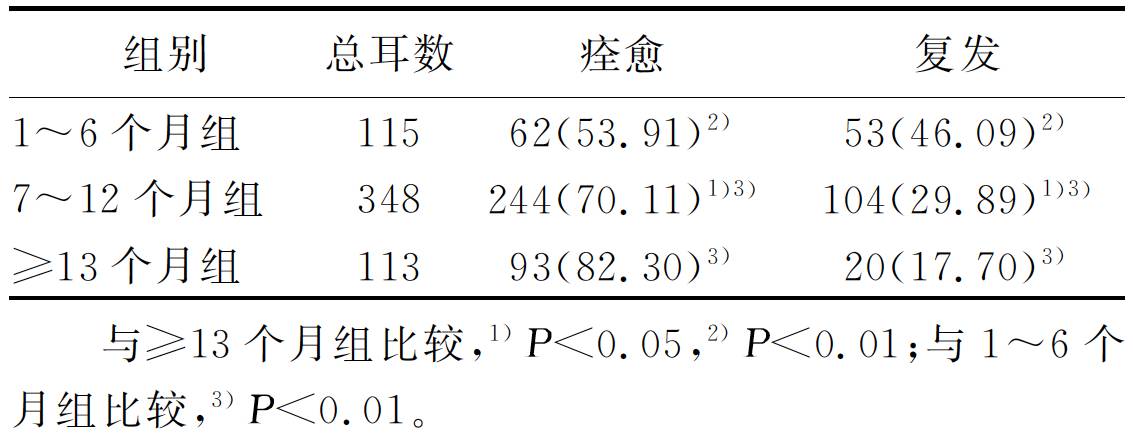
5. Relationship Between Retention Time and Recurrence After Tube Removal
In the initial tympanostomy, a short-term button-type tympanostomy tube was implanted (576 ears), with retention times ranging from 1 to 23 months and an average retention time of (9.96±3.72) months. Most ears had retention times concentrated between 6 and 14 months. For recurrent ears (177 ears), the average retention time was (8.59±3.49) months, while for cured ears (399 ears), it was (10.57±3.65) months. Independent sample t-tests indicated a statistically significant difference in retention times between recurrent and cured ears (t=6.078, p<0.01). The retention times were categorized into three groups based on distribution and average values: 1-6 months, 7-12 months, and ≥13 months, with significant differences in recurrence rates among the three groups (p<0.01). The 1-6 months group and the 7-12 months group had a significant difference in recurrence rates after tube removal (p<0.01); similarly, the 1-6 months group and the ≥13 months group (p<0.01); and the 7-12 months group and the ≥13 months group (p<0.05). Results indicated that shorter retention times correlated with higher recurrence rates, with a significantly increased recurrence rate for retention times shorter than 6 months. Distribution and recurrence rate data for different groups are shown in Table 1.
Table 1 Comparison of Retention Time and Recurrence Rate After Initial Insertion Among Three Groups (Ear %)
Among the recurrent ears (177 ears), 79 underwent re-insertion, with an average retention time of (7.50±3.40) months for re-inserted ears, which was 3 months shorter than that of the cured group (399 ears). Independent sample t-tests indicated a statistically significant difference in retention times between the two groups (t=6.929, p<0.01).
6. Relationship Between AR and Recurrence After Tympanostomy
According to the diagnostic criteria for AR: ① one or more symptoms of seasonal nasal mucosal congestion, rhinorrhea, sneezing, or nasal itching; ② allergen testing indicating clear allergens. Among 331 children, 128 (38.67%) were diagnosed with AR after clinical evaluation. Among the children who underwent tube removal or self-removal, 104 experienced recurrence, with 62 (59.62%) having AR. Chi-square test analysis indicated a statistically significant difference in AR prevalence between the two groups (χ2=14.112, p<0.01).
Of the 47 children who required re-insertion due to recurrence, 32 (68.09%) had AR. Among the 227 children who recovered after initial tube removal or self-removal, 66 (29.07%) had AR. Chi-square test analysis showed a statistically significant difference in AR prevalence between the two groups (χ2=25.792, p<0.01).
7. Postoperative Complications After Tympanostomy
According to follow-up data, the incidence of complications after tympanostomy was 6.34%, including ear effusion, acute suppurative otitis media, middle ear granulation, tympanic membrane perforation, and tinnitus. Ear effusion was the most common complication, and all complications resolved after conservative treatment. Three cases (0.91%) of tympanic membrane perforation did not heal.
According to large sample statistics from Europe and America, about 90% of children under 10 years old have experienced SOM, with 80% being unilateral cases, and the incidence age mostly concentrated between 6 months to 4 years, exceeding 50% in those under 1 year old and over 60% by the age of 2, averaging four occurrences per year. Particularly for children with congenital cleft palate, Down syndrome, and other craniofacial anatomical abnormalities, the risk of developing SOM is higher due to affected normal structure and function of the Eustachian tube. Studies by Tos et al. (1984) indicate that children from India, Alaska, and Asia have a higher incidence risk.
Most children with SOM do not have prolonged illness and typically recover within three months, but 30%-40% may experience recurrence, and 5%-10% may persist for over a year. Although SOM is a self-limiting disease, its occurrence between 6 months and 4 years significantly impacts children’s hearing and language development, with some children even displaying behavioral clumsiness and decreased balance ability. Therefore, despite most SOM children recovering through observation or conservative treatment, some still require surgical intervention. The 2013 American tympanostomy clinical guidelines and the 2016 American guidelines for secretory otitis media recommend tympanostomy as the first-line surgical option for SOM. Tympanostomy can significantly reduce the recurrence rate and duration of middle ear effusion in children during the first year post-operation, while also improving average hearing by 6-12 dB HL during the tube retention period. Approximately 6.7% of children under 3 years old in the United States have undergone tympanostomy. Preschool children are a high-risk group for SOM, and this study reached a similar conclusion, with most tube-inserted children concentrated between the ages of 3-6, and no gender differences in age at first insertion. The distribution of recurrent patients’ ages was also uneven, primarily concentrated in children aged 3-6 at the time of first insertion, accounting for 93.27% of all recurrent patients. Reports indicate that 20%-50% of children experience SOM recurrence after the initial tympanostomy tube falls out, and this study similarly found a recurrence rate of 31.21% after the initial tube fell out, with no correlation to the gender of recurrent patients.
The recommended retention time for tympanostomy tubes by our hospital’s physicians is between 7-18 months, which may vary for several reasons: ① no literature reports on the optimal retention time, leading to a lack of experience; ② some doctors believe prolonged retention time may affect children’s daily life (bathing) and activities (swimming), thus recommending shorter retention times; ③ individual physician experiences vary, with some suggesting removal and others recommending waiting for natural fall-out. For the initial tympanostomy, we generally use a button-type short-term tympanostomy tube, which is reported to have a typical retention time of 8-16 months. This study found that most tympanostomy tubes were retained for 6-14 months, which is 2 months shorter than previously reported literature. The average retention time for cured ears was significantly different from that of recurrent ears, with recurrent ears having a retention time 2 months shorter than cured ears. This study also compared recurrence rates for different retention times, finding significant differences in recurrence rates for retention times of 1-6 months, 7-12 months, and ≥13 months, with recurrence rates significantly decreasing as retention time increased, which aligns with reports by Yaman et al.
Daniel et al. reported that among children who underwent initial tympanostomy with short-term tympanostomy tubes, 20%-25% required re-insertion due to recurrence within two years post-operation. This study found that 14.20% of children required re-insertion after the initial tube fell out, with their average initial retention time being 3 months shorter than that of the cured group. The results suggest that the need for re-insertion is related to the duration of the initial tympanostomy tube retention, with longer retention times potentially reducing the recurrence rate of SOM. Although some literature indicates that longer retention times do not reduce recurrence rates, most current literature supports that longer retention times correlate with lower SOM recurrence rates. If retention times exceed 3 years, the incidence of long-term postoperative complications such as tympanic membrane perforation, tympanosclerosis, and cholesteatoma will significantly increase, thus tubes should be removed timely if retention times exceed 2 years.
In recent years, more studies have begun to focus on the role of AR in the incidence and recurrence of SOM in children. It is currently believed that AR can affect the normal function of the Eustachian tube, with reports of AR incidence among SOM children ranging from less than 10% to greater than 80%. This study found AR prevalence rates of 38.67%, 59.62%, and 68.09% among children with tympanostomy, recurrent children, and those requiring re-insertion, respectively, indicating that AR is a significant factor for recurrence after tube removal. Doner et al. studied the impact of AR on postoperative recurrence rates, comparing a group of recurrent children after tympanostomy with a control group of healthy children without recurrence, and found a positive rate of inhalant and/or food allergens of 36.4% in the experimental group, compared to only 8.3% in the control group, with significant differences between the two. Hurst et al. found that refractory recurrent SOM is associated with AR and analyzed the efficacy of anti-allergic treatment in allergen-positive children, reporting that 85% of the treatment group achieved recovery, whereas the control group showed no significant improvement. There are also reports indicating that asthmatic children are more likely to require multiple insertions. Compared to primary SOM, the impact of allergies on recurrent SOM is more significant, with mechanisms including direct inflammation of the middle ear mucosa, leading to inflammation of the Eustachian tube mucosa, causing swelling and obstruction of the tube, promoting the reflux of bacterial-laden secretions from the nasopharynx to the middle ear; these mechanisms may individually or collectively affect postoperative recurrence rates. Therefore, it is clinically necessary to conduct comprehensive allergen testing for children with postoperative recurrence, and if positive, anti-allergic and desensitization treatments should be provided as needed. Other studies have also found chronic sinusitis and gastroesophageal reflux associated with the incidence and recurrence of SOM in children, potentially due to inflammatory secretions or reflux stimulating Eustachian tube dysfunction. Additionally, some studies have found a high incidence of SOM among children with adenoid hypertrophy, thus clinical work should screen for adenoid hyperplasia in SOM children, and adenoidectomy may be performed during surgery based on the condition to help reduce SOM recurrence rates.
Postoperative complications such as ear effusion, acute suppurative otitis media, middle ear granulation, tympanic membrane perforation, and tinnitus are relatively common. This study found a complication incidence rate of 6.34% after tympanostomy, but all complications, except for 3 cases of tympanic membrane perforation, resolved with conservative treatment. This indicates that tympanostomy with short-term tympanostomy tubes is a relatively safe procedure with a low incidence of long-term complications, making it suitable as the first-line surgical treatment for SOM. Tympanostomy does not lead to serious complications, but shorter retention times are associated with a higher likelihood of recurrence, with a significantly reduced recurrence rate for retention times exceeding 13 months. Therefore, it is recommended that tympanostomy retention times should exceed 13 months.
In summary, children aged 3-6 are prone to recurrence after tympanostomy, with shorter tympanostomy tube retention times correlating with higher recurrence risks, especially in children with AR. There are currently no unified standards regarding the choice of tympanostomy tubes and postoperative retention times, and clinical studies and guidelines both domestically and internationally have not provided definitive guidance. This study, through a large sample retrospective analysis, provides strong evidence for clinicians regarding the choice of tympanostomy tubes and retention times for children undergoing tympanostomy. To reduce recurrence rates after tube removal, we recommend using T-tubes for first tympanostomies in children aged 3-6, especially those with AR, with appropriate retention times extended to over 13 months; the younger the age, the longer the retention time, to avoid peak incidence; after age 6, button-type tubes can be used, allowing for natural fall-out.

More content
Please follow our WeChat account

Long press the QR code to follow