Recently, a “heart” measuring 2.5 centimeters was created using 3D printing. Although it has defects, it seems to bring us one step closer to the future of organ transplantation propelled by biological 3D printing.
The First Vascularized 3D Printed Heart
On April 15, Tel Aviv University announced that its laboratory had 3D printed a “heart,” with the experimental results published in the comprehensive scientific journal Advanced Science.
This heart is not merely a shape. It contains cells, blood vessels, and other supporting structures. It can even contract like a heart—but its length is only 2.5 centimeters, roughly the size of a rabbit’s heart. Professor Assaf Shapira, one of the leaders of the Tel Aviv University research team, told this journal: “Compared to the past, the breakthrough of this 3D printed heart research is that this is not just an appearance of a printed heart; it is the world’s first 3D vascularized engineered heart made using the patient’s own cells and biological materials, which means it has vascular tissue.” Prior to this, scientists had only successfully printed simple tissues without blood vessels.
 3D Printing Process of the Heart
3D Printing Process of the Heart
Assaf Shapira added: “The materials we used to print the heart were extracted from the patient. We extracted slices of adipose tissue, edited them to become stem cells, and then converted them into cardiomyocytes and endothelial cells. Additionally, we extracted non-cellular tissue and transformed it into a ‘personalized gel’ to act as the printing ‘ink.’ These materials, composed of sugars and proteins, can be used to 3D print complex tissue models, and then using tissue engineering principles, fill the scaffolds with cells to allow the cells to regenerate better.” He said, the ‘printing materials’ and ‘adhesives’ used in this experiment come from the patient’s own cells, which is crucial for successfully constructing tissues and organs, meaning the printed heart will not cause rejection when transplanted into the patient’s body.
In fact, heart transplantation has been hailed as the pinnacle of 21st-century medicine. Currently, thousands of people around the world undergo heart transplant surgeries each year using traditional methods, where hearts from brain-dead patients are provided while still beating, and hospitals place the hearts in special materials, collaborating with commercial airlines to transport them—brain-dead donor ischemia time is limited to 6 hours—the receiving hospital must obtain the heart and perform the transplant within this timeframe. Currently, the mortality rate after heart transplantation remains high, primarily related to rejection reactions. In 1978, Zhang Shize and other doctors completed the first heart transplant surgery in mainland China at Ruijin Hospital in Shanghai, but the patient survived only 109 days post-surgery. Even now, the 5-year survival rate after heart transplant surgery is just over 50%.
Thus, if the technology from Tel Aviv University can prove effective in future human trials and address the rejection issues associated with traditional heart transplant surgeries, it would indeed be a significant breakthrough.
When asked why they chose to 3D print a heart instead of a kidney or other organ tissues, Assaf responded: “In terms of difficulty, I cannot discern which is easier. But currently, the traditional method of heart transplantation is the only available treatment for patients with end-stage heart failure. The severe shortage of heart donors compels us to strive to develop new methods.”
The heart, due to its large size, diverse cell types, and the need to beat, requires nearly all cardiomyocytes to contract almost simultaneously to function. Even after years of development in 3D printing technology, in the medical field, cases of 3D printed prosthetics in craniofacial surgery, orthopedics, and dentistry are common today. Although scientists have long mastered the technology of artificially cultivating simple human tissues, it remains challenging to 3D print a heart that matches the patient’s cellular, biochemical, and anatomical characteristics.
Assaf does not shy away from expressing some regrets about this experiment, stating, “Due to the limitations of our 3D printer’s precision, we currently cannot print all the blood vessels on the heart, and this heart also does not have pumping functionality.” The 3D printed “heart” is still far from being applicable in animal experiments.
So, what exactly makes 3D printing a heart so difficult? The root cause can be traced back to the issue of Earth’s gravity—the inability of the printed heart to pump blood is due to the heart not being able to beat uniformly; a uniform heartbeat requires tight connections between heart cells, etc. The existence of Earth’s gravity directly or indirectly leads to the inability to achieve these conditions.
How can we make the printed heart beat?
3D printing a heart is far more than just stacking a bunch of cells to resemble a heart. The experiment at Tel Aviv University falls under the category of “bioprinting” in 3D printing. The core difference between a 3D printer and a traditional printer is: on one hand, traditional printing is two-dimensional flat printing, while 3D printing is three-dimensional spatial printing, layering materials; traditional printing uses ink, while a 3D printer’s ink varies according to different experimental purposes. Unlike the lasers or heat commonly used in other 3D printing, bioprinting uses cells, and to ensure cell viability, light and heat cannot be present. Bioprinting requires setting printing parameters based on different cellular growth environments, accurately controlling the density of cells in the biological material, the location of growth factors in the overall 3D structure, and their related functions, to ensure that the printed tissue has biological activity.
The heart is more complex than general organs, mainly because it beats. The heartbeat occurs because cardiomyocytes are tightly connected, and the electrical signals generated by cells cause large groups of cardiomyocytes to contract together. Furthermore, to coordinate the synchronous contraction of the two atria and two ventricles, the heart has a special conduction system.
While producing tens of millions of cardiomyocytes in vitro is not difficult, even if the heart is 3D printed, whether it can beat is one issue, and how it beats is another. For example, in clinical conditions, ventricular fibrillation occurs when cardiomyocytes cannot beat synchronously. Once “synchronization” is lost, the cells will beat in a chaotic manner, causing the heart to instantly lose its pumping function, leading to death. In other words, to achieve the heart’s pumping function, it must beat very uniformly.
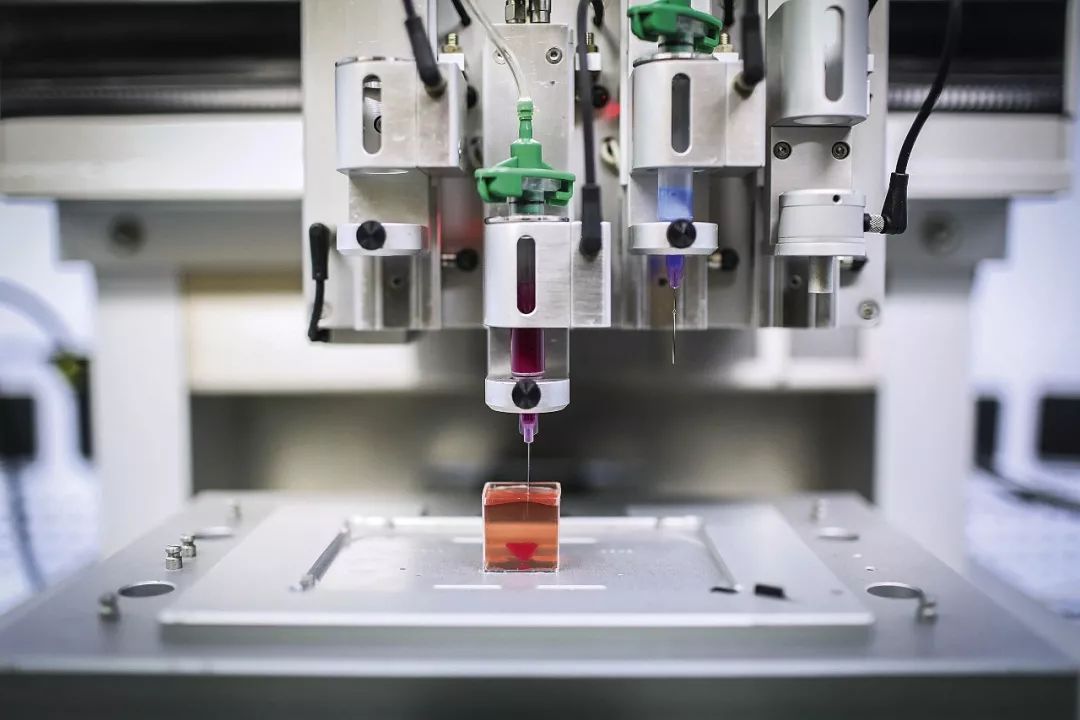
On April 15, at Tel Aviv University’s laboratory, a 3D printer is currently printing a 3D heart (Photo | AFP)
The heart printed by Tel Aviv University has not yet reached the point of synchronous beating of a large number of cells and generating sufficient force. A professor from a neuroscience department at an American university told this journal: “According to the paper published on this experiment, there is electrical connectivity between the printed tissues, and there is a phenomenon of synchronous beating among adjacent cells. However, this is still far from meeting the requirements for synchronous beating.”
So, why can’t the heart printed by the Tel Aviv University team beat uniformly? The answer is related to Earth’s gravity. “The adhesion of 3D printed materials is insufficient to support large organs like the heart or kidneys, and the influence of Earth’s gravity can cause tearing between cells.” Xin Xie, a researcher at Harvard University, told this journal. He is also a co-founder of the organ-on-a-chip company ApreX. His main research areas include microelectromechanical systems, bioprinting, microfluidic chips, and organ chips. “The core issue of bioprinting is to address the impact of biological materials and gravity on 3D printed cells.”
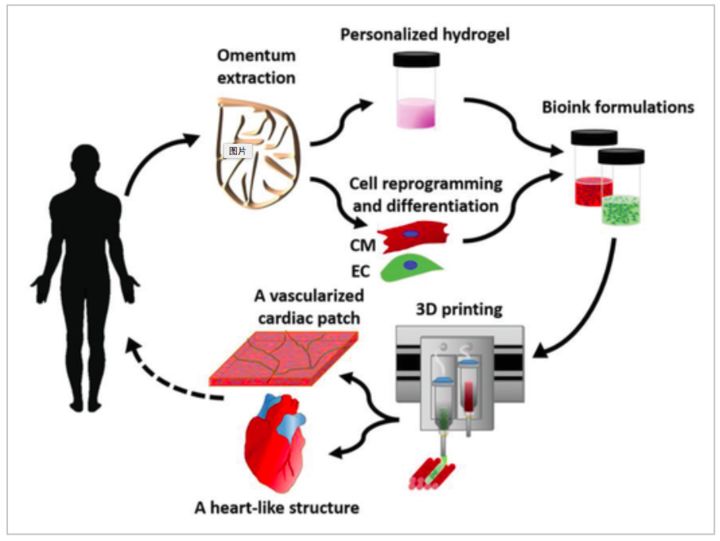
Image from Tel Aviv University official website
In the field of microelectromechanical systems, Xin Xie studies micron and nanoscale devices. In such micro-scale specific situations, the electrostatic adhesion force is much greater than the weight of the device, so researchers often overlook the impact of gravity and focus more on calculating electrostatic adhesion force. “This law inversely explains why it is feasible to print small organ cell models in bioprinting, but once it comes to printing real sizes (such as a 250-gram heart), due to the supporting and adhesive forces between cells being constant (not changing with the size of the printed object), it can lead to two outcomes: on one hand, the lower cells may collapse under the increasing pressure from the upper cells; on the other hand, if they do not collapse under pressure, during transfer and transportation, the upper cells may not withstand the weight of the lower cells and tear apart.”
What does tearing between cells mean? Cells in the body can only “grow” together through mutual contact and recognition, and this contact and recognition are achieved through protein molecules. The contact between protein molecules is like a key opening a lock, finely connecting and activating many machines within the cells, gradually strengthening the connection between the two cells. During the heart printing process, the cardiomyocytes in the “ink” are spherical and do not contact each other; after printing, the cells need to grow together to become mature cardiomyocytes, and a large number of protein molecules need to connect between cells. The aforementioned American university neuroscience professor described the microscopic scene during the bioprinting process: when cells drop from the print head, they will contact other cells, at which point the protein molecules will recognize each other, but initially, only a few molecules contact each other, creating a very weak bond. If a large number of cells drop, gravity can tear apart the newly established connections, just like an elephant can easily break a hair.

Using patient cells and biological materials to 3D print a three-dimensional vascularized engineered heart
In summary, due to the existence of gravity, the printed heart’s cells lack tight connections, which in turn affects the heart’s beating frequency, preventing it from having normal pumping functionality. If in a zero-gravity environment in space, the cells could float together, protein molecules could gradually strengthen the connections between cells, allowing the heart to potentially beat uniformly.
3D Printing a Heart in Outer Space
Five years ago, NASA began systematically funding outstanding 3D printing projects. This May, the International Space Station (ISS) may witness the first 3D printed heart in a zero-gravity environment, with the total cost of the process estimated at around $7 million, of which launch costs account for 80%.
“NASA hopes to eliminate factors that affect material synthesis during the 3D printing process in a weightless environment,” Xin Xie added. His startup is exploring how to use the microgravity environment on the International Space Station for research on artificial organ tissues, and he is very supportive of the idea of 3D printing large organs in a zero-gravity environment.
Assaf Shapira is also aware of NASA’s plans to attempt 3D printing a heart in outer space. “That’s too expensive; I personally don’t think we need to go to outer space to achieve this result. Indeed, current bioprinting technology does not yet allow for the printing of intricate, naturally dense vascular systems. Printing on Earth requires the use of a load-bearing scaffold (Support Medium) to some extent to control the effects of Earth’s gravity. Currently, the operation involves mixing cells with materials similar to hydrogels for printing; the hydrogel itself lacks mechanical structure support, so external scaffolding is needed to fill the cells into the pores.”

Assaf Shapira, one of the leaders of the Tel Aviv University experimental team
In this regard, Xin Xie insists that the small-sized heart printed by Assaf’s team requires support from a load-bearing scaffold to complete the printing, so the difficulty of printing large-sized organs can be imagined. “It is extremely challenging to 3D print a complete human organ on Earth without scaffolding, as the presence of scaffolding affects the contact between cells. Although hydrogel scaffolding can adjust softness and hardness, in this Israeli case, to ensure load-bearing capacity, a hard scaffold must be used, making it difficult for cells to grow together.”
Among the several projects accompanying SpaceX to the International Space Station is a company called Techshot, which has developed technology for NASA, space exploration companies, and other partners for over 25 years. It developed a bioprinter in collaboration with nScrypt, which created the world’s first 3D bioprinter in 2003. Since last year, Techshot has been researching how to automate experiments on the International Space Station, helping meet the medical needs for long-term deep space exploration missions, with the ultimate goal of establishing an organ manufacturing factory in space to ensure that humans do not have to wait too long for 3D printed organs. The company has publicly declared a mission-driven goal: “Our aim is to achieve transplantable organs in space.”
In 2016, Techshot and nScrypt successfully 3D printed the vascular structure of a heart using adult human stem cells in a zero-gravity environment. If all goes as planned, the International Space Station will soon have a personalized, customized bioprinter suitable for the outer space environment, capable of 3D printing more detailed and complex tissues. The key word here is “detailed”; Kenneth Church, CEO of nScrypt, has stated publicly that the cell layers printed by nScrypt’s 3D bioprinter are several times finer than a human hair. “You can imagine this difference as holding a fine pen instead of a crayon while painting.” The nScrypt BAT 3D printer uses Smart Pump patented technology to achieve precise control of the flow rate of biological materials, with volume control as low as 100 microliters and can use nozzles as small as 10 microns. This is essential for printing the fine details of human organs.
It is worth noting that 3D printing in outer space is just one step towards complete human organ printing. Even if achieved, there is still a long way to go before animal experiments.“The first challenge of bioprinting large organs is to solve the tearing problem caused by their own weight; otherwise, all subsequent issues are meaningless. After solving this problem, we can continue to optimize the cell culture environment, intercellular communication, and selection of biological materials, gradually moving towards the direction we want to see,” Xin Xie added.
Even if the gravity issue is eliminated and the heart can beat uniformly, the difficulty of 3D printing a heart is not over—only with a continuous supply of blood can the printed organ or tissue survive for an extended period.There is still no clear answer on how to establish a vascular network, and the issue of blood circulation is almost a deadlock for 3D printed solid organs. The heart itself requires about 10% of the total blood circulation to nourish itself; once deprived of blood, all organs can only “survive” at 4 degrees Celsius. If the printed cells require a body temperature of 37 degrees, there is almost no time to complete the printing because the cells printed first will die from lack of oxygen before the printing is finished. This is also one of the difficulties mentioned by Professor Assaf Shapira during the interview. “One of the bottlenecks we need to solve is how to provide oxygen and nutrients to the growing tissue, to maintain cell viability from ‘day zero’—from the moment the printed structure is extracted from the supporting culture medium. To this end, we have ordered a customized special bioreactor that can circulate oxygenated growth medium within the main blood vessels and chambers of the printed heart.”
Will this special “bioreactor” solve the problem? It cannot be verified at this time. However, if this bioreactor proves effective, it should have already made significant contributions in the field of organ transplantation, and today’s organ transplantation would not have to rush to catch flights; it could be done leisurely in the “bioreactor” for a few days before transplantation.
Even as bioprinting takes steps towards the scenarios seen in science fiction novels, Assaf emphasized at the end of the interview: “I hope we can never print a complete human being. We do not want to play God; we just want to help those with heart diseases.”
(This article was published in Sanlian Life Weekly, Issue 20, 2019)
Everyone is watching

⊙ All article copyrights belong to Sanlian Life Weekly. Welcome to share to Moments, please contact the backstage for reprinting.
Click the image, one-click order
【Why “I Love My Family”】
▼ Click to read the original text, enter the weekly bookstore,to purchase more good books.