MEM Introduction
Ulnar-sided wrist pain is common among athletes, and the usual causes include independent or combined injuries to the triangular fibrocartilage complex (TFCC), the extensor carpi ulnaris (ECU), and the distal radioulnar joint (DRUJ). Sports that require repeated forearm pronation/supination, radial/ulnar deviation, and axial loading can easily lead to ulnar-sided wrist pain in athletes. For example, injuries to the TFCC, ECU, and DRUJ are common in sports such as golf, tennis, baseball, and hockey. In the athletic population, these injuries are also frequent causes of ulnar-sided wrist pain. Therefore, early diagnosis and treatment are crucial for these individuals, helping them return to their sport as soon as possible. In February 2017, Eric Quan Pang and Jeffery Yao published an article titled “Ulnar-sided wrist pain in the athlete (TFCC/DRUJ/ECU)” in Current Reviews in Musculoskeletal Medicine (IF=4.1) that integrated and reviewed a large amount of literature on ulnar-sided wrist pain, introducing five aspects: anatomical structure, injury classification, clinical diagnosis, imaging characteristics, and treatment. It pointed out that there are various options for the diagnosis, treatment, and rehabilitation of ulnar-sided wrist pain, and many factors must be considered, including the purpose of sports, especially when dealing with athlete patients, where factors such as their specific sport and position in competition need to be considered.

MEM Provides Detailed Interpretation
PART 1 Anatomical Overview
ECU (extensor carpi ulnaris) originates from the lateral epicondyle of the humerus and inserts at the base of the fifth metacarpal. At the level of the wrist, it passes through the sixth dorsal compartment of the ulnar side of the wrist, which is stabilized by the extensor retinaculum and an independent sheath located 1.5-2 cm distal to the ulnar styloid. A recent study on human specimens found that the proximal part of the independent sheath is better at maintaining the dynamic stability of the ECU in its groove compared to the distal part. The distal morphology of the ulna may be associated with ECU injuries. In one study, MRI of patients with ECU injuries or subluxation revealed that negative ulnar variance is related to ECU injury and instability. Additionally, the depth of the ulnar groove and the ulnar styloid may also be directly associated with ECU injury; a shallower ulnar groove tends to lead to ECU injury, while an excessively large ulnar styloid can cause changes in the ECU tendon due to direct mechanical stimulation.
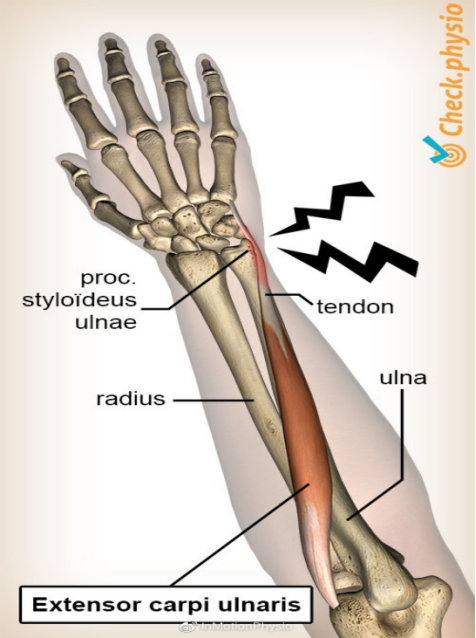
Image source: Internet
TFCC (triangular fibrocartilage complex) consists of the triangular fibrocartilage (TFC), ulnar collateral ligament, dorsal/palmar superficial and deep ligaments, and the sheath of the extensor carpi ulnaris. The superficial radioulnar ligament is connected to the ECU sheath and the deep ligaments, commonly referred to as the ulnar subligament, which connects to the central fossa and base of the ulnar styloid. The TFCC is a load-bearing structure located between the ulna and the carpal bones, absorbing 18%-20% of the load on the wrist. When there is positive ulnar variance, it can lead to increased transmission of forces, while negative variance reduces it. Patients with positive ulnar variance also show reduced TFCC thickness, while those with negative variance show increased thickness. Furthermore, the forces at the ulnar wrist joint increase with gripping activities and wrist pronation. The blood supply to the TFCC mainly comes from branches of the ulnar artery, which reach the peripheral part of the TFCC in a radial pattern from the palmar, dorsal, and ulnar sides, supplying 10%-40% of the peripheral area. The central and radial parts are relatively avascular, limiting their healing capacity. Regarding nerve innervation, a recent study on human specimens found that the dorsal cutaneous branch of the ulnar nerve (100%), the medial cutaneous nerve of the forearm (91%), and the palmar branch of the ulnar nerve (73%) innervate the TFCC.
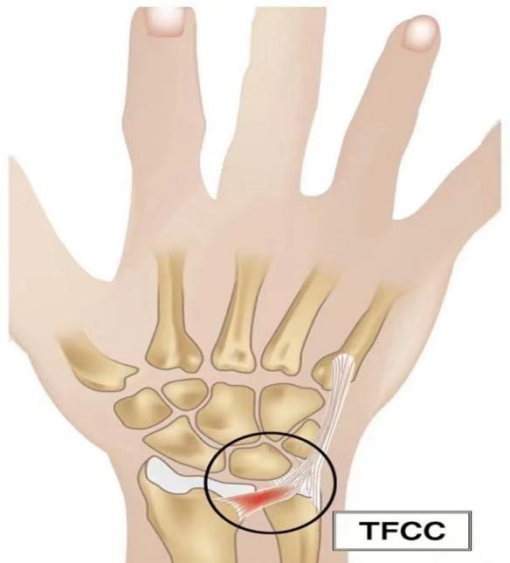 Image source: Internet
Image source: Internet
DRUJ (distal radioulnar joint) is an axle joint formed by the ulnar notch of the radius and the articular surface of the ulna. It is generally believed that the dorsal radioulnar superficial ligament and the deep radioulnar ligament tighten to maintain stability during pronation of the joint. Conversely, during supination, the dorsal radioulnar deep ligament and the superficial radioulnar ligament tighten to maintain stability. Additionally, the stability of the DRUJ is closely related to the ECU and TFCC.
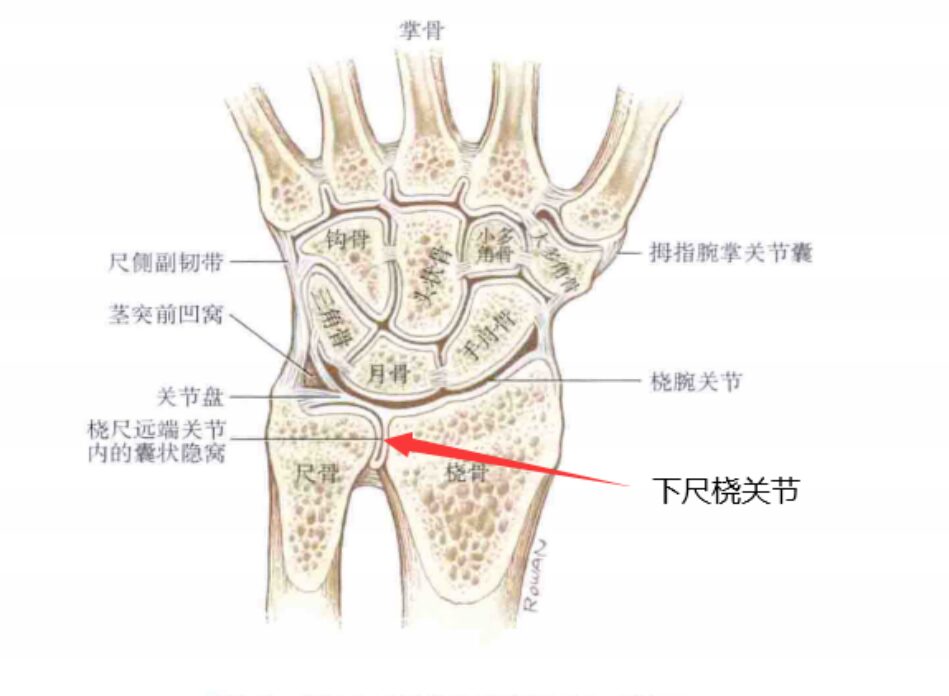 Image source: Internet
Image source: Internet
PART 2 Injury Classification and Diagnosis
01 Classification and Diagnosis of ECU Injuries
Regarding ECU tendon injuries, an earlier study divided 28 tennis players with ulnar-sided wrist pain into three categories: instability, tendinopathy, and tendon rupture. This classification has some guiding effects on treatment. For the ECU sheath, a study based on 12 patients with recurrent ECU dislocation who underwent surgery classified ECU sheath ruptures into three types: ulnar side, radial side, and periosteal avulsion.
In the differential diagnosis of ECU lesions, clinical examination plays a significant role. Studies show that if a patient exhibits tendon instability upon examination, they usually have a history of acute injury; conversely, they may only present with vague ulnar dorsal wrist pain, and the history is more concealed. In physical examinations, patients with tendon instability will show a series of symptoms, and since passive movements may not elicit symptoms to some extent, it is necessary to actively conduct physical examinations. Typically, the sixth dorsal compartment experiences maximum pressure during wrist and forearm supination, and patients with tendinopathy will experience pain at this time. If a feeling of weakness without pain occurs, it indicates an ECU tendon rupture. Common examination methods include the ECU synergy test, where the patient places the affected limb on the table, maintains the elbow at 90 degrees of flexion, and the wrist and arm in supination, then resists resistance while abducting the thumb. If pain occurs at the ECU site, it indicates a positive result.
Imaging techniques commonly used to assess ECU injuries include MRI (magnetic resonance imaging) and musculoskeletal ultrasound.
●MRI is a useful tool for the differential diagnosis of ECU injuries, where tendinitis and tendinopathy appear as areas of increased signal intensity on MRI. A recent study found that MRI has a sensitivity of 57% and specificity of 88% in detecting ECU tendinopathy and can also assess the integrity of other critical structures (such as the extensor retinaculum). Since the position of the ECU is influenced by wrist joint activity, it is necessary to examine it during pronation or supination.
●Musculoskeletal ultrasound is also an effective method for assessing ECU injuries, as it is convenient to use and allows for dynamic evaluation in different positions. However, it is worth noting that studies have found that up to 75% of asymptomatic patients may show tendinopathy or even tendon rupture on ultrasound, making it essential to combine ultrasound results with clinical examinations.
02 Classification and Diagnosis of TFCC Injuries
Regarding TFCC injuries, earlier studies primarily classified them as traumatic changes and degenerative changes, and subsequently subclassified them based on the location of the injury. Due to the complexity of its structure, some studies have divided it into three parts: proximal triangular ligament, distal hammock structure, and ulnar collateral ligament. The injury levels are mainly classified into the following six grades:
Table 1: TFCC Injury Level Classification
|
Grade |
Injury Situation |
Treatment Strategy |
|
0 |
Isolated ulnar styloid fracture withoutTFCC injury |
Splinting; for some refractory cases, surgical removal of bone fragments may be necessary |
|
1 |
Isolated peripheral tear of the distal hammockstructure withoutDRUJ instability |
TFCC suturing |
|
2 |
Complete tear of the proximal or deep fibers from the central fossa,hook test positive,TFCC laxity |
Re-fixation of the central fossa of the TFCC |
|
3 |
Complete tear of the superficial or deep fibers from the proximal,hook test positive,TFCC laxity |
Re-fixation of the central fossa of the TFCC |
|
4 |
IrreparableTFCC tear |
Tendon graft reconstruction |
|
5 |
TFCC tear accompanied byDRUJ arthritis |
Tendon graft reconstruction and arthroplasty |
For the differential diagnosis of TFCC injuries, clinical physical examinations are mainly conducted through a series of tests, including the piano key test, ulnar wrist stress test, and press test. Positive results from these tests may suggest the presence of a TFCC injury. In terms of imaging, the primary methods include X rays, MRI (magnetic resonance imaging), and CT arthrography.
●X rays are usually part of the initial examination for patients, which can rule out potential fractures, osteoarthritis, and malalignment. Ulnar lesions/upright styloid fractures are highly correlated with TFCC injuries, so X rays play a role in diagnosing TFCC injuries.
●MRI (magnetic resonance imaging) is a commonly used imaging tool to assess potential TFCC injuries, but its effectiveness is inconsistent, with sensitivity ranging from 67%-100% and specificity from 71%-100%. It is worth mentioning that MRA (magnetic resonance arthrography) has also been applied to the pathological diagnosis of TFCC, sometimes with accuracy even higher than that of magnetic resonance imaging. In one study, patients with central TFCC tears and peripheral tears underwent both MRA and MRI, with MRA showing an accuracy of 95.8%, while MRI had accuracies of 77.1% and 87.5%, respectively.
●CT arthrography is another method available for diagnosing TFCC injuries. A study based on 10 human specimens found that the sensitivity, specificity, and accuracy of CT arthrography for TFCC tears were all 100%. Subsequent studies have also shown that under different plane conditions, CT arthrography has a sensitivity of 83%, specificity of 40%, and positive predictive value of 76% for central fossa lesions of the TFCC.
PART 3 Treatment and Prognosis
01 ECU Treatment and Prognosis
For ECU tendinopathy, non-surgical treatment is usually recommended, including rest, activity modification, and a certain period of immobilization, which can alleviate symptoms in most cases, followed by a progressive rehabilitation program to help athletes gradually resume activities. For cases with a long duration and ineffective conservative treatment, surgical treatment is recommended, which can clean up the affected area, repair the damaged tendon, and relieve the pressure in the sixth dorsal compartment. For ECU tendon instability, immobilization should be prioritized, using a short-arm cast or even a long-arm cast for 6-8 weeks, while conducting periodic stress checks and evaluations through ultrasound or MRI to ensure ECU sheath healing. If instability persists, continued immobilization or surgical treatment may be necessary.
For acute ECU injuries, some researchers suggest surgery as the primary treatment option. Of course, the treatment principles depend on the type of injury; for patients with complete ECU rupture, surgery is definitely the first choice, but its incidence is relatively rare. In the athlete population, partial palmaris longus grafts are primarily used for ECU tendon reconstruction.
The prognosis is related to the type of injury and surgical method. If only simple synovectomy is performed, short-arm splinting of the wrist joint for about 2 weeks is recommended; if tendon reconstruction surgery is performed, then elbow flexion at 90 degrees, forearm in neutral position, and long-arm cast immobilization for 4-6 weeks are required, with restrictions on vigorous activities within two months after immobilization ends.
02 TFCC and DRUJ Treatment and Prognosis
For TFCC injuries, if assessment shows no DRUJ (distal radioulnar joint) instability, conservative treatment should be adopted, including rest, immobilization, braces, activity modification, and local corticosteroid injections. A recent study found that among a group of patients with pathological changes in the TFCC, 57% experienced symptom relief after 4 weeks of immobilization. However, if conservative treatment is ineffective, surgical treatment is recommended.
For more severe TFCC injuries, surgical treatment is the preferred option. As mentioned earlier, the anatomical structure of the TFCC is complex, and treatment should be classified based on the location of the injury, mainly into three categories:
▷ First, central tears, due to poorer blood supply compared to the peripheral region, have poor healing capacity and often require debridement to stabilize the edges. Additionally, thermal coagulation and denervation of the TFCC have been shown to be effective in treating TFCC injuries, with the former stabilizing the TFCC and the latter alleviating pain. For patients with positive ulnar variance, simple debridement may not resolve the potential hazards caused by ulnar impaction and ulnar styloid, necessitating USO (ulnar shortening osteotomy) or wafer surgery. Although wafer surgery may have smaller incisions and lower chances of nonunion, if significant positive ulnar variance or combined instability of the lunate and triquetrum is present, USO is the preferred surgical method.
▷ Second, peripheral tears, due to better blood supply compared to central tears, have better healing capacity. When conservative treatment is ineffective, repair surgery can be performed. If accompanied by DRUJ instability, further surgical stabilization is required, with options for open surgery or arthroscopic surgery. One study indicated that arthroscopic treatment of acute TFCC injuries may be more effective than chronic injuries. For irreparable TFCC tears accompanied by DRUJ instability, palmaris longus grafts should be used for reconstruction.
▷ Third, radial-sided tears; the blood supply to the radial side of the TFCC is very limited, so lesions in this area usually require debridement. If accompanied by DRUJ instability, further surgical repair is needed. A new technique has been proposed in one study, where the torn radial side of the TFCC is sutured to the radial side of the radius via a bone bridge for repair. The prognosis for TFCC injuries also depends on the surgical method; if only simple debridement is performed, immobilization for two weeks is sufficient. If reconstruction is performed, short-arm cast immobilization for 4 weeks is required, followed by gradual rehabilitation.
The treatment and rehabilitation of TFCC injuries require careful consideration of various factors related to the athlete, as do the aforementioned ECU injuries. Athlete patients are a unique group, as the treatment and rehabilitation of their injuries may impact their career arrangements, cycles, and lifespan. Therefore, before treatment and rehabilitation, it is essential to communicate thoroughly with the athlete and consider various factors, such as their competitiveness, remaining season time, team strength, contracts, and social impacts.
MEM Conclusion
For ulnar-sided wrist pain occurring in various sports, traditional medical practices may not adequately account for the uniqueness of athletes in treatment and rehabilitation. Often, the same diagnostic, treatment, and rehabilitation methods are applied to athletes, which can have significant impacts, potentially leading to misdiagnosis, delayed treatment, and overtreatment. Medical personnel must incorporate the uniqueness and individual factors of athletes into the formulation of diagnosis, treatment, and rehabilitation plans to achieve optimal recovery and early return to the field for athletes.

-End-
Statement: The information contained in this material is derived from the cited papers and does not represent the views of MEM. The post is for reference only; for the original content, please click “Read Original” to read it.